Abstract
Background
Withdrawal movement during rocuronium injection is a common, unresolved adverse effect. We aimed to investigate the effect of IV acetaminophen pretreatment on withdrawal movement during rocuronium injection.
Methods
This study enrolled 120 American Society of Anesthesiologists (ASA) I-II patients undergoing general anesthesia. They were randomly assigned to three treatment groups. After occluding venous drainage using a tourniquet on the upper arm, the saline group received 5 ml of 0.9% sodium chloride solution, the lidocaine group received 40 mg of lidocaine, and the acetaminophen group received 50 mg of acetaminophen. During injection of pretreatment drug, pain was assessed on a four-point scale. The tourniquet was released after 120 seconds and anesthesia was performed using thiopental sodium 5 mg/kg followed by rocuronium 0.6 mg/kg. The withdrawal movement was graded on a four-point scale in a double-blind manner.
Pain from the injection of rocuronium is a common side effect in anesthetic practice, with incidence of 50-80% [1,2]. The pain is at times severe, with a burning sensation [2,3]. Rocuronium injection pain can elicit withdrawal movement of the arm or generalized movement of the body, even after loss of consciousness, during induction of anesthesia [1,4]. These withdrawal movements may dislodge a venous catheter or cause injury during induction [5]. Pretreatment with midazolam, lidocaine, and ondansetron have been used in attempts to reduce this pain [4,6].
Acetaminophen is widely used for pain management and antipyresis as an alternative to aspirin and NSAIDsbut its action at the molecular level is remaining largely unknown. It is believed to be centrally active, producing analgesia and antipyresis by inhibiting cyclooxygenase (COX) in the hypothalamus [7]. From animal studies, its anti-nociceptive effects reflect a combination of peripheral and central actions resulting from COX-2 inhibition [8,9]. The peripheral action of acetaminophen suggests that IV acetaminophen with venous occlusion could decrease rocuronium injection pain and decrease the incidence of withdrawal movements. In this randomized, double-blind, placebo-controlled study, we aimed to compare the effect of IV acetaminophen with that of lidocaine to prevent rocuroinum-induced withdrawal movements during the induction of anesthesia.
The Ethics Committee of our hospital approved the study protocol. Patients aged 19-69 years, of ASA physical status I and II, were randomly selected from all elective surgical lists using a random number generator (http://www.random.org), and 132 patients were assessed for eligibility. Patients with chronic pain syndrome, neurological deficits, thrombophlebitis, difficult venous access, and clinical conditions that contraindicated the administration of any of the drugs used in the study were excluded.
After written informed consent was obtained, a total of 120 patients were randomly allocated into 3 groups using a sealed envelope method - 120 sealed envelopes (40 for each group) containing the names of groups were prepared before study. None of the patients was premedicated before entering the operation room. On arrival in the operating room, patients were monitored with electrocardiogram, non-invasive arterial pressure, and pulse oximeter. A 20-gauge catheter was inserted into a superficial radial vein on the patient's non-dominant hand, and its position was confirmed by a free flow of lactated Ringer's solution infusion by gravity. The lactated Ringer's solution was infused at 100 ml/h for five minutes. After five minutes, the infusion was stopped and the arm with the IV line was elevated for 15 seconds for gravity drainage of venous blood. After occluding venous drainage using a rubber tourniquet on the upper arm, the patients were pretreated with test drug. An independent anesthetist prepared the solutions and the investigator was oblivious to the contents of the solutions. The test drug was administered over 10 seconds. Patients in group I (saline) received 5 ml normal saline, group II (lidocaine) received lidocaine 40 mg (0.8% lidocaine 5 ml) and group III (acetaminophen) received 50 mg (5 ml) of acetaminophen (Perfalgan®, Bristol-Myers Squibb, France). We asked the patients if they felt any pain during injection of the test drug and the pain was assessed on a four-point scale: 0, no pain; 1, mild pain (pain reported only in response to questioning without any behavioral signs); 2, moderate pain (pain reported in response to questioning and accompanied by a behavioral signs); and 3, severe pain (strong vocal response or response accompanied by facial grimacing, arm withdrawal, or tears) [6].
After 2 minutes, the rubber tourniquet was released and 2.5% thiopental sodium 5 mg/kg was injected over 10-15 seconds. Twenty seconds after the administration of thiopental, the anesthetist checked unconsciousness (as assessed by no verbal response and loss of the eyelash reflex). After loss of consciousness, 1% rocuronium (0.6 mg/kg) was injected over 5 seconds. During and after the injection of rocuronium, withdrawal movement was observed by the study-blinded investigator. Withdrawal movement was graded by the investigator according to the following scale: 1, no response; 2, movement at wrist only; 3, movement/withdrawal involving arm only (elbow/shoulder); and 4, generalized response (movement/withdrawal in more than one extremity, cough, or breath holding) [4]. The anesthesia continued with an appropriate technique at the discretion of the attending anesthesiologist. Twenty-four hours after the operation, the injection site was checked for pain, edema, wheal, or flare response.
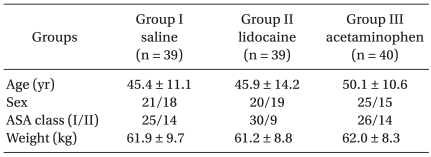
A total of 118 patients were successfully examined in the study. Two patients were dropped due to difficulty of IV placement on dorsum of hand. Groups were similar with regard to age, weight, gender, and American Society of Anesthesiologist physical status (Table 1).
We estimated the incidence of withdrawal movement to be around 70% from other studies [2,4]. A power analysis indicated that a sample size of 37 in each group was sufficient to have 80% power (Type II error β = 0.2) of detecting a 30% difference in incidence of withdrawal movement among the 3 groups at a 95% significance level (Type I error α = 0.05). To compensate for patient dropout, the sample size was increased to 40 patients per group.
Statistical analyses were performed using a statistical package (SPSS 13.0 for windows, SPSS Inc., Chicago, IL, USA). Data are presented as a mean (±SD) or number of patients. Demographic data were analyzed using the χ2 test and one-way analysis of variance. The incidence of pain on test drug injection and the incidence of withdrawal movement were analyzed using the Kruskal-Wallis test. Post hoc test were done by Mann-Whitney U test with Bonferroni correction. Statistical significance was defined as P < 0.05.
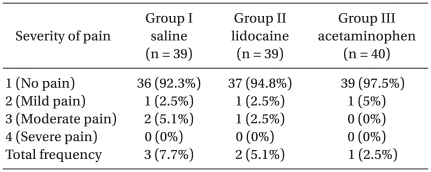
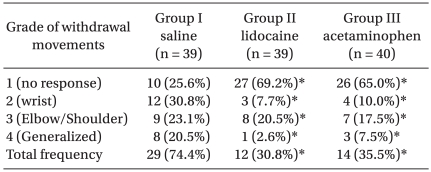
The overall incidence of pain on pretreatment drug injection was 7.7% (3/39), 5.1% (2/39), and 2.5% (1/40) in groups I, II, and III, respectively (Table 2), with no significant difference between groups. The overall incidence of withdrawal movement after rocuronium injection (grade 2 or more) was 74.4% (29/39), 30.8% (12/39), and 35.0% (14/40) in groups I, II, and III, respectively (Table 3), with group II and group III showing significantly fewer withdrawal movements than group I (P = 0.00). There were no significant differences in the degree of withdrawal movement between groups II and III. There were no complications, such as pain, edema, wheal, or flare, observed at the injection site within the first 24 hours after the operation in any of the treatment groups.
In this study, acetaminophen pretreatment with venous occlusion significantly reduced the incidence of rocuronium-induced withdrawal movements, from 74.4% in the saline group to 35.0% in the acetaminophen group, similar to the 30.8% after lidocaine. This suggests that acetaminophen pretreatment also attenuated withdrawal movement during rocuronium injection to the same extent as lidocaine. The overall incidence of injection pain during drug pretreatment was 7.7%, 5.1%, and 2.5% in the saline, lidocaine, and acetaminophen groups, respectively, indicating that acetaminophen causes less injection pain and is suitable for pretreatment.
Peripheral veins are innervated with polymodal nociceptors that mediate pain responses to injected drugs [10]. Rocuronium is formulated using sodium acetate, sodium chloride, or acetic acid to produce a solution of pH 4, and therefore can cause burning pain and withdrawal movements. This pain may be caused by osmolality [11], pH of the solution [12], or local release of mediators such as kininogen cascade [13]. Rocuronium injection increases bradykinin concentrations in the skin [14], and the algogenic effect of rocuronium may result from direct activation of C-nociceptors with concomitant release of the calcitonin gene-related peptide (CGRP) and prostaglandin (PG) E2.
Acetaminophen can act centrally, as PG production in the brain is 10 time more sensitive to inhibition by acetaminophen than that in the spleen [7], although later studies showed different tissue effects. For example, Swierkosz et al. [15] showed the greatest reduction of PG E2 synthesis was in the lung followed by the spleen and brain. Abbott and Hellemans [8] showed the analgesic effects of acetaminophen reflect central and peripheral actions. Lee et al. [16] showed that acetaminophen selectively suppresses peripheral PG E2 release and increases COX-2 gene expression in a clinical model of acute inflammation. Hinz et al. [9] showed acetaminophen inhibits COX-2 activity in human blood cells and suppresses PG E2 generation in human blood monocytes. Thus, acetaminophen inhibition of PGE2 may influence the intensity of rocuronium injection pain and withdrawal movements.
Tourniquet use is a common technique to minimize rocuronium injection pain [4,6]. Shevchenko et al. [4] showed pretreatment with lidocaine and venous occlusion decreased the incidence of withdrawal movements to 46%. Memis et al. [6] showed that pretreatment of lidocaine with venous occlusion was more effective than ondansetron, tramadol, or fentanyl. Venous occlusion allows study of the peripheral action of drugs without a central effect, similar to a Bier block [17]. Huang et al. [18] showed that 10 mg ketorolac and longer venous occlusion (120 seconds, but not 30 or 60 seconds) reduced propofol injection pain. IV acetaminophen shows a systemic analgesic effect in 3 minutes [19], so we used a 120-second occlusion time. In our study, we used rubber tourniquet. That is easy to use, but it may have inconsistent pressure for different patients, a potential limitation of our study.
Lidocaine, a local anesthetic, reversibly blocks peripheral nerve pathways by blocking excitable membranes and is commonly used to reduce pain and withdrawal movements after rocuronium injection to 28-46% [4,6]. Here, lidocaine pretreatment decreased withdrawal movement to 30.8%. A novel ready-to-use formulation of intravenous acetaminophen does not cause pain on injection and offers improved local safety [20]. We did not find complications after pretreatment, and pain after IV injection of acetaminophen is normally 2-4.1% [21,22], similar to our study (2.5%).
In conclusion, pretreatment with acetaminophen (50 mg) reduced the incidence of rocuronium-induced withdrawal movement as much as lidocaine. Further studies are required to determine the optimal dose of IV acetaminophen to control rocuronium-induced withdrawal movement and suppress CGRP and PG E2 release.
References
1. Borgeat A, Kwiatkowski D. Spontaneous movements associated with rocuronium: is pain on injection the cause? Br J Anaesth. 1997; 79:382–383. PMID: 9389860.

2. Steegers MA, Robertson EN. Pain on injection of rocuronium bromide. Anesth Analg. 1996; 83:203. PMID: 8659757.

3. Cheong KF, Wong WH. Pain on injection of rocuronium: influence of two doses of lidocaine pretreatment. Br J Anaesth. 2000; 84:106–107. PMID: 10740559.

4. Shevchenko Y, Jocson JC, McRae VA, Stayer SA, Schwartz RE, Rehman M, et al. The use of lidocaine for preventing the withdrawal associated with the injection of rocuronium in children and adolescents. Anesth Analg. 1999; 88:746–748. PMID: 10195516.

5. Lui JT, Huang SJ, Yang CY, Hsu JC, Lui PW. Rocuronium-induced generalized spontaneous movements cause pulmonary aspiration. Chang Gung Med J. 2002; 25:617–620. PMID: 12479624.
6. Memiş D, Turan A, Karamanlioğlu B, Süt N, Pamukçu Z. The prevention of pain from injection of rocuronium by ondansetron, lidocaine, tramadol, and fentanyl. Anesth Analg. 2002; 94:1517–1520. PMID: 12032018.

7. Flower RJ, Vane JR. Inhibition of prostaglandin synthetase in brain explains the anti-pyretic activity of paracetamol (4-acetamidophenol). Nature. 1972; 240:410–411. PMID: 4564318.

8. Abbott FV, Hellemans KG. Phenacetin, acetaminophen and dipyrone: analgesic and rewarding effects. Behav Brain Res. 2000; 112:177–186. PMID: 10862949.

9. Hinz B, Cheremina O, Brune K. Acetaminophen (paracetamol) is a selective cyclooxygenase-2 inhibitor in man. FASEB J. 2008; 22:383–390. PMID: 17884974.

10. Arndt JO, Klement W. Pain evoked by polymodal stimulation of hand veins in humans. J Physiol. 1991; 440:467–478. PMID: 1804973.

11. Tuncali B, Karci A, Tuncali BE, Mavioglu O, Olguner CG, Ayhan S, et al. Dilution of rocuronium to 0.5 mg/ml with 0.9% NaCl eliminates the pain during intravenous injection in awake patients. Anesth Analg. 2004; 99:740–743. PMID: 15333404.

12. Lockey D, Coleman P. Pain during injection of rocuronium bromide. Anaesthesia. 1995; 50:474. PMID: 7793569.

13. Borgeat A, Kwiatkowski D, Ruetsch YA. Spontaneous movements associated with rocuronium injection: the effects of prior administration of fentanyl. J Clin Anesth. 1997; 9:650–652. PMID: 9438893.

14. Blunk JA, Seifert F, Schmelz M, Reeh PW, Koppert W. Injection pain of rocuronium and vecuronium is evoked by direct activation of nociceptive nerve endings. Eur J Anaesthesiol. 2003; 20:245–253. PMID: 12650497.

15. Swierkosz TA, Jordan L, McBride M, McGough K, Devlin J, Botting RM. Actions of paracetamol on cyclooxygenases in tissue and cell homogenates of mouse and rabbit. Med Sci Monit. 2002; 8:BR496–BR503. PMID: 12503027.
16. Lee YS, Kim H, Brahim JS, Rowan J, Lee G, Dionne RA. Acetaminophen selectively suppresses peripheral prostaglandin E2 release and increases COX-2 gene expression in a clinical model of acute inflammation. Pain. 2007; 129:279–286. PMID: 17175104.

17. Koppert W, Sittl R, Schmelz M. The Bier block as an experimental tool to differentiate peripheral and central effects of analgesics on people. Schmerz. 2000; 14:69–76. PMID: 12800042.
18. Huang YW, Buerkle H, Lee TH, Lu CY, Lin CR, Lin SH, et al. Effect of pretreatment with ketorolac on propofol injection pain. Acta Anaesthesiol Scand. 2002; 46:1021–1024. PMID: 12190806.

19. Moller PL, Sindet-Pedersen S, Petersen CT, Juhl GI, Dillenschneider A, Skoglund LA. Onset of acetaminophen analgesia: comparison of oral and intravenous routes after third molar surgery. Br J Anaesth. 2005; 94:642–648. PMID: 15790675.

20. Flouvat B, Leneveu A, Fitoussi S, Delhotal-Landes B, Gendron A. Bioequivalence study comparing a new paracetamol solution for injection and propacetamol after single intravenous infusion in healthy subjects. Int J Clin Pharmacol Ther. 2004; 42:50–57. PMID: 14756388.

21. Sinatra RS, Jahr JS, Reynolds LW, Viscusi ER, Groudine SB, Payen-Champenois C. Efficacy and safety of single and repeated administration of 1 gram intravenous acetaminophen injection (paracetamol) for pain management after major orthopedic surgery. Anesthesiology. 2005; 102:822–831. PMID: 15791113.

22. Canbay O, Celebi N, Arun O, Karagöz AH, Saricaoğlu F, Ozgen S. Efficacy of intravenous acetaminophen and lidocaine on propofol injection pain. Br J Anaesth. 2008; 100:95–98. PMID: 17959585.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download