Abstract
Background and Objectives
Kawasaki disease (KD) is the leading cause of acquired heart disease, which predominantly occurs in children under the age of 5 years. However, there are fewer cases of KD in infants younger than 6 months, which makes it difficult to diagnose. We investigated the clinical manifestations of KD in this age group and compared them with those in the older age group.
Subjects and Methods
We retrospectively reviewed the medical records of 239 patients with KD admitted to the Hallym Sacred Heart Hospital from January 2013 to June 2015. The data were categorized into 2 groups by age: Group A (≤6 months, n=26) and Group B (>6 months, n=213).
Results
Group A had a longer hospitalization period than Group B (6.69 vs. 5.19 days, p=0.002). Group A had fewer clinical manifestations upon admission, due to which there was a higher incidence of incomplete KD (1.88 vs. 3.54 of the diagnostic criteria, p<0.05; and 19.2% vs. 4.2% incomplete KD incidence, p=0.002). The rate of cardiac complications was higher in Group A (30.8% vs. 11.7%, p=0.011).
Conclusion
The rate of cardiac complications of the patients younger than 6 months was significantly higher than that of the older patients. Therefore, infants younger than 6 months with unexplained fever for more than 5 days should be suspected as having KD, even if the principal clinical features are not fully presented. Echocardiography must be appropriately used for diagnosis of KD in suspected patients.
Kawasaki disease (KD) is an acute, self-limiting febrile vasculitis with the highest incidence in East Asian children. It is the leading cause of acquired heart disease, which predominantly occurs in children younger than 5 years.1)2) The etiology is unknown, and it has no specific diagnostic test. Thus, diagnosis of KD is based on clinical findings of its signs and symptoms.3)4) Complete KD has been diagnosed with ≥5 days of fever and ≥4 of its 5 clinical features that include bilateral conjunctival injection without exudates, polymorphous exanthem, erythematous changes in the lips and the oral cavity, swelling and erythema of the hands and feet, and cervical lymphadenopathy (>1.5 cm). Incomplete KD should be considered in patients with unexplained fever for ≥5 days and with 2 or 3 of the clinical features of KD.5)
The peak incidence of KD is from 6 months to 2 years of age. However, there are fewer cases in infants younger than 6 months, which makes it difficult to diagnose. KD patients younger than 6 months are more likely to have an incomplete clinical presentation. Therefore, the diagnosis could be delayed, which results in more frequent cardiac complications than in older children.6)7)8)
We comparatively investigated the clinical manifestations of KD patients aged younger than 6 months and those of older KD patients, in order to help in early diagnosis.
We retrospectively reviewed the medical records of 239 patients with KD admitted to the Hallym University Sacred Heart Hospital from January 2013 to June 2015. Their demographic, clinical, laboratory, and echocardiographic data were extracted from each medical record after approval by the Institutional Review Board of Hallym University Sacred Heart Hospital (2015-I085).
KD was diagnosed when the fever duration was ≥5 days and when ≥4 of the 5 major clinical manifestations were observed. The patients who were suspected with KD but who did not satisfy the diagnostic criteria or did not undergo intravenous immunoglobulin (IVIG) after the diagnosis was made were excluded from this study. In addition, when ≥4 of the 5 major clinical manifestations were confirmed, KD was diagnosed even though fever was observed for 4 days. Incomplete KD was diagnosed when 2 or 3 of the 5 major clinical manifestations were confirmed with abnormal echocardiographic findings.5)
The data were categorized into 2 groups by age: Group A (≤6 months, n=26) and Group B (>6 months, n=213). The demographic variables studied were the median age, sex, fever duration, full hospitalization period, hospitalization period before the IVIG administration, number of diagnostic criteria, and rate of incomplete KD. A blood test and urinalysis were performed on the day of the admission. The laboratory variables included the white blood cell (WBC) count, neutrophils percentage, hemoglobin, hematocrit, platelet count, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), albumin, total bilirubin, direct bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transpeptidase, brain natriuretic peptide (BNP), pyuria, and proteinuria. Echocardiography was performed initially before or shortly after the IVIG administration, then 6 to 8 weeks later.
Cardiac complications were determined when ≥1 of the following 3 echocardiographic findings were confirmed: 1) the Z-score of the left anterior descending (LAD) coronary artery or right coronary artery (RCA) was 2.5 or higher; 2) the coronary artery (CA) satisfied the aneurysm criteria of the Japanese Ministry of Health (in the patients aged <5, a ≥3 mm CA inner diameter; in the patients aged ≥5 years, a >4 mm CA inner diameter; a CA inner diameter at least 1.5 times the inner diameter of the surrounding blood vessels; or a CA inner diameter that is not absolutely even); and 3) when ≥3 of the following criteria were satisfied: mild or severe mitral or aortic valve regurgitation; valve disorder, including intermediate or severe tricuspid or pulmonary valve regurgitation; ≥2 mm pericardial effusion in the patients aged <1 and ≥3 mm in the patients aged ≥1 year; left ventricular contraction disorder; brightness in the surrounding areas of the bold vessel; tapering blood vessels; and a 2-2.5 Z-score in the LAD coronary artery or RCA.3)4)5)
Aspirin (50 mg/kg/day) and IVIG (2 g/kg) were administered during the acute phase of the illness. After the patient became afebrile, the dose of aspirin was reduced to 5 mg/kg/day and maintained for 6-8 weeks. If the patient showed abnormalities in his/her coronary arteries, the aspirin administration was continued until the patient no longer showed evidence of coronary changes. If the patient had recurrent or persistent fever for ≥36 hours after the IVIG administration, a second dose of IVIG was administered. Furthermore, methylprednisolone was intravenously administered if the patient had recurrent or persistent fever even after the second IVIG administration.9)10)
The Statistical Package for the Social Sciences version 16.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. The variables were compared with the results of the chi-square test for the categorical variables, and with the results of the Mann-Whitney U test for the continuous variables. A p of <0.05 was considered statistically significant.
A total of 239 patients with KD were admitted to Hallym Sacred Heart Hospital from January 2013 to June 2015. Of these patients, 26 (10.8%) were 6 months of age or younger (Group A), and 213 (89.2%) were older than 6 months (Group B) (Table 1).
Table 2 compared the clinical data of Group A and Group B. The fever duration before the admission was significantly shorter in Group A (3.4 days) than in Group B (4.3 days) (p=0.001), and the hospitalization period was longer in Group A (6.9 days) than in Group B (5.0 days) (p=0.001). Especially, the hospitalization period before the IVIG administration was longer in Group A (p=0.001). The fever duration before the IVIG administration and the total fever
duration were longer in Group A, without statistical significance.
The patients in Group A expressed each symptom less than those in Group B. Upon admission, the rates of expression of cervical lymphadenopathy, conjunctival injection, lip & tongue erythema, and peripheral edema & erythema were significantly lower in Group A. At the time of the diagnosis and the IVIG administration, the rates of expression of cervical lymphadenopathy and conjunctival injection were significantly lower in Group A (Table 3). As a result, the rate of incomplete KD was significantly higher in Group A (23.1% vs. 2.9%, p=0.002).
Eight patients in Group A and 26 in Group B had cardiac complications, and the rate of cardiac complications of Group A was significantly higher than that of Group B (30.8% vs. 12.2%, p=0.011). Six of the 8 patients with cardiac complications in Group A had abnormalities in their initial examination; of which, 2 had a small aneurysm, and 6 had dilated coronary arteries (Table 4).
According to the laboratory data, the Group A patients had significantly higher WBC (16546/uL vs. 14372/uL, p=0.015) and platelet counts (483000/uL vs. 357000/uL, p=0.001). Moreover, their hematocrit and hemoglobin levels were significantly lower (32% vs. 34% for hematocrit, p=0.006; and 10.47 g/dL vs. 11.56 g/dL for hemoglobin, p<0.05). However, the ESR was significantly higher in Group B (44.2 mm/hr vs. 54.5 mm/hr, p=0.008). The BNP and CRP levels were higher in Group A, without significance (178.45 pg/mL vs. 139.19 pg/mL of BNP, p=0.321; and 94.57 mg/L vs. 82.66mg/L of CRP, p=0.167). In addition, the AST and ALT were higher in Group B, without significance (61.5 IU/L vs. 116.1 IU/L of AST, p=0.835; 46.0 IU/L vs. 121.7 IU/L of ALT, p=0.668). The albumin was higher in Group B, though insignificantly (4.06 g/dL vs. 4.18 g/dL, p=0.059). There was no significant difference between the other laboratory variables of Group A and Group B (Table 5).
The rates of administration of the second IVIG and the intravenous methylprednisolone (IMPD) were higher in Group A, though insignificantly (rate of the second IVIG administration, 19.2% vs. 14.1%, p=0.484; rate of the first IMPD administration, 3.8% vs. 1.9%, p=0.508; and rate of the second IMPD administration, 3.8% vs. 0.5%, p=0.074). Also, the rate of antibiotics administration before using intravenous immunoglobulin therapy was higher in Group A (50.0%) than Group B (39.4%), without significance (Table 6).
KD is an acquired heart disease most common in infants aged 6 months to 2 years. It is challenging to make a diagnosis of incomplete KD, particularly in infants younger than 6 months with fewer clinical manifestations.1)7)11) The diseases that must be differentiated from KD because of similar clinical findings include viral infection (measles, adenovirus, enterovirus, and Epstein-Barr virus), scarlet fever, staphylococcal scalded skin syndrome, toxic shock syndrome, polyarteritis nodosa, bacterial cervical lymphadenitis, and Juvenile rheumatoid arthritis.5)12)
The clinical manifestations of KD in this study were similar to those in other studies. Kim et al.13) surveyed the epidemiologic features of KD in South Korea in 2009-2011 and noted that conjunctival injection, redness of the lips and the oral mucosa, and polymorphic rash were the most common findings in the KD patients. In this study, the most common symptom in Group B was conjunctival injection, followed by erythema of the lips and the oral cavity, and skin rash. However, in the KD patients aged ≤6 months, skin rash was the most common symptom, followed by conjunctival injection and erythema of the lips and the oral cavity. In addition, 93.8% of the KD patients aged ≤ 6 months with skin rash experienced redness at the Bacille Calmette-Guerin site.
Joffe et al.14) reported that infants had fewer of the accepted criteria and a higher incidence of incomplete KD. Chuang et al.15) found that infants aged ≤3 months with KD usually presented incomplete clinical manifestations. Similarly, in this study, Group A showed fewer diagnostic criteria than Group B. Group A showed a significantly higher incomplete KD rate of 23.1% than Group B (2.9%).
Ram Krishna et al.16) studied the predictors of coronary artery aneurysm. They suggested that anemia, low albumin, elevated ESR, elevated CRP, and pyuria are the risk factors of coronary artery abnormalities. Bayers et al.17) reported that an elevated neutrophil count, an elevated ESR, low albumin, and low hemoglobin are associated with coronary artery lesions. In this study, Group A showed an elevated WBC count, thrombocytosis, and a low hemoglobin level. These suggest the more severe inflammatory reaction of the KD patients aged≤6 months. The low hemoglobin level in Group A might be due to physiologic anemia, which is commonly shown in infants aged≤6 months. The significantly high WBC count in Group A might be normal as it is common in healthy infants aged ≤6 months.18) Contrary to expectations, the ESR of Group A was lower than that of Group B, possibly because the patients younger than 6 months were admitted earlier and underwent blood tests in the earlier stage of their fever than the older patients. Group A showed higher levels of CRP than Group B, though insignificantly.
The most common complications of KD include coronary artery dilatation caused by coronary artery vasculitis and aneurysm. Other complications include decreased coronary arterial compliance, myopericarditis, arrhythmias, ischemic heart disease, pericardial effusion, valvular regurgitation, myocardial infarction, and sudden cardiac death. The complications of untreated KD can be severe and life-threatening.10)19) Thus, early diagnosis is important, but no specific diagnostic test has been introduced as yet. In previous studies,16)20)21) a fever duration and an age<1 year were confirmed as the risk factors of coronary complications. On the other hand, Hangai et al.2) in a review of neonatal KD in Japan reported similar rates of coronary abnormalities between neonatal and older patients. In addition, Lee et al.22) studied the prevalence of coronary abnormalities in KD patients younger and older than 3 months, respectively, and found that the rate of coronary abnormalities in the KD patients younger than 3 months was only insignificantly higher than that in the older patients.
However, Chang et al.18) showed a higher rate of incomplete KD and coronary complications in KD patients<6 months than in older patients, and Rosenfeld et al.,23) who studied KD in infants <1 year, noted that the KD patients younger than 6 months had a higher risk of developing coronary artery aneurysm. Similarly, in this study, the rate of cardiac complications of Group A (30.8%) was significantly higher than that of Group B (12.2%). Moreover, the rate of incomplete KD was also higher in the infants aged ≤6 months. The reasons for the low KD incidence and the high incomplete KD ratio in infants may be the protective effects of the passive maternal antibody and the immature immune reaction in infants.2)7)
This study had several limitations. First, the number of KD patients aged ≤6 months was significantly smaller than the number of older KD patients, thereby causing difficulties in statistical comparison. Second, in many cases, the blood test was conducted only once on admission; as such, it was challenging to compare the laboratory data before and after the use of IVIG.
In conclusion, infants <6 months with unexplained fever for >5 days should be suspected of KD, even if the principal clinical features are not fully presented. Echocardiography must be appropriately used for diagnosis of KD in suspected patients.
Figures and Tables
Table 1
Demographic data of Kawasaki disease patients

Table 2
Comparison of the clinical features of infantile Kawasaki disease patients and older patients
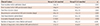
Table 3
Comparison of the clinical manifestations of infantile Kawasaki disease patients and older patients

Table 4
Echocardiographic abnormal findings and Z-score in Kawasaki disease patients aged 6 months or younger
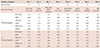
Table 5
Comparison of laboratory data of infantile Kawasaki disease patients and older patients
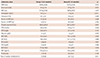
Data are expressed as mean±standard deviation or n (%). WBC: white blood cell, ANC: absolute neutrophil count, HPF: high power field, ESR: erythrocyte sedimentation rate, CRP: C-reactive protein, AST: aspartate aminotransferase, ALT: alanine aminotransferase, TB: total bilirubin, DB: direct bilirubin, GGT: gamma-glutamyl transpeptidase, BNP: brain natriuretic peptide
Table 6
Comparison of treatments of infantile Kawasaki disease patients and older patients

References
1. Yeom JS, Woo HO, Park JS, Park ES, Seo JH, Youn HS. Kawasaki disease in infants. Korean J Pediatr. 2013; 56:377–382.
2. Hangai M, Kubota Y, Kagawa J, et al. Neonatal Kawasaki disease: case report and data from nationwide survey in Japan. Eur J Pediatr. 2014; 173:1533–1536.
3. Yu JJ. Diagnosis of incomplete Kawasaki disease. Korean J Pediatr. 2012; 55:83–87.
4. Freeman AF, Shulman ST. Kawasaki disease: summary of the American Heart Association guidelines. Am Fam Physician. 2006; 74:1141–1148.
5. Newburger JW, Takahashi M, Gerber MA, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation. 2004; 110:2747–2771.
6. No SJ, Kim DO, Choi KM, Eun LY. Do predictors of incomplete Kawasaki disease exist for infants? Pediatr Cardiol. 2013; 34:286–290.
7. Park YW, Han JW, Park IS, et al. Epidemiologic study of Kawasaki disease in 6 months old and younger infants. Korean J Pediatr. 2008; 51:1320–1323.
8. Burns JC, Wiggins JW Jr, Toews WH, et al. Clinical spectrum of Kawasaki disease in infants younger than 6 months of age. J Pediatr. 1986; 109:759–763.
9. Sánchez-Manubens J, Bou R, Anton J. Diagnosis and classification of Kawasaki disease. J Autoimmun. 2014; 48-49:113–117.
10. Bayers S, Shulman ST, Paller AS. Kawasaki disease: part II. Complications and treatment. J Am Acad Dermatol. 2013; 69:513.
11. Uysal F, Bostan OM, Celebi S, Uysal B, Hamitoglu S, Cil E. Outcomes of Kawasaki disease: a single-center experience. Clin Pediatr (Phila). 2015; 54:579–584.
12. Verma P, Agarwal N, Maheshwari M. Recurrent Kawasaki disease. Indian Pediatr. 2015; 52:152–154.
13. Kim GB, Han JW, Park YW, et al. Epidemiologic features of Kawasaki disease in South Korea: data from nationwide survey, 2009-2011. Pediatr Infect Dis J. 2014; 33:24–27.
14. Joffe A, Kabani A, Jadavji T. Atypical and complicated Kawasaki disease in infants. Do we need criteria? West J Med. 1995; 162:322–327.
15. Chuang CH, Hsiao MH, Chiu CH, Huang YC, Lin TY. Kawasaki disease in infants three months of age or younger. J Microbiol Immunol Infect. 2006; 39:387–391.
16. Ram Krishna M, Sundaram B, Dhanalakshmi K. Predictors of coronary artery aneurysms in Kawasaki disease. Clin Pediatr (Phila). 2014; 53:561–565.
17. Bayers S, Shulman ST, Paller AS. Kawasaki disease: part I. Diagnosis, clinical features, and pathogenesis. J Am Acad Dermatol. 2013; 69:501.e1–501.e11. quiz 511-2.
18. Chang FY, Hwang B, Chen SJ, Lee PC, Meng CC, Lu JH. Characteristics of Kawasaki disease in infants younger than six months of age. Pediatr Infect Dis J. 2006; 25:241–244.
19. Kim JJ, Hong YM, Yun SW, et al. Assessment of risk factors for Korean children with Kawasaki disease. Pediatr Cardiol. 2012; 33:513–520.
20. Jamieson N, Singh-Grewal D. Kawasaki disease: a clinician’s update. Int J Pediatr. 2013; 2013:645391.
21. Yeo Y, Kim T, Ha K, et al. Incomplete Kawasaki disease in patients younger than 1 year of age: a possible inherent risk factor. Eur J Pediatr. 2009; 168:157–162.
22. Lee EJ, Park YW, Hong YM, Lee JS, Han JW. Epidemiology of Kawasaki disease in infants 3 months of age and younger. Korean J Pediatr. 2012; 55:202–205.
23. Rosenfeld EA, Corydon KE, Shulman ST. Kawasaki disease in infants less than one year of age. J Pediatr. 1995; 126:524–529.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download