Abstract
Background and Objectives
Subjects and Methods
Results
Figures and Tables
Fig. 1
The benefit of statin on MACE before and after propensity matching in each of the 4 groups, which were divided according to the baseline level of high density lipoprotein cholesterol and triglyceride. Group A (HDL-C≥40 mg/dL and triglyceride<150 mg/dL; n=11819), group B (HDL-C≥40 mg/dL and triglyceride≥150 mg/dL; n=3329), group C (HDL-C<40 mg/dL and triglyceride<150 mg/dL; n=6062) and group D (HDL-C<40 mg/dL and triglyceride≥150 mg/dL; n=3443). MACE: major adverse cardiac event, HDL-C: high density lipoprotein cholesterol, HR: hazard ratio, CI: confidence interval.

Fig. 2
The benefit of statin on the secondary end point in each of the 4 groups. Group A (HDL-C≥40 mg/dL and triglyceride<150 mg/dL; n=11819), group B (HDL-C≥ 40 mg/dL and triglyceride≥150 mg/dL; n=3329), group C (HDL-C<40 mg/dL and triglyceride<150 mg/dL; n=6062), and group D (HDL-C<40 mg/dL and triglyceride≥150 mg/dL; n=3443). HDL-C: high density lipoprotein cholesterol, CD: cardiac death, MI: myocardial infarction, TVR: target vessel revascularization, TLR: target lesion revascularization, HR: hazard ratio, CI: confidence interval.

Fig. 3
Comparison of changes of the levels of triglyceride (A), HDL-C (B), LDL-C (C), and hs-CRP (D) after statin therapy between group A and group D. HDL-C: high density lipoprotein cholesterol, LDL-C: low density lipoprotein cholesterol, hs-CRP: high sensitivity C-reactive protein.
Table 1
Comparison of clinical baseline characteristics after propensity score matching in group A (HDL-C≥40 mg/dL and TG<150 mg/dL) and group B (HDL-C≥40 mg/dL and TG≥150 mg/dL)

Values are n (%) or mean±standard deviation. HDL-C: high density lipoprotein cholesterol, TG: triglyceride, BMI: body mass index, SBP: systolic blood pressure, DBP: diastolic blood pressure, HR: hazard ratio, IHD Hx.: ischemic heart disease history, HTN Hx.: hypertension history, DM: diabetes mellitus, HL Hx.: hyperlipidemia history, MI: myocardial infarction, STEMI: ST-segment elevation myocardial infarction, NSTEMI: non-ST segment elevation myocardial infarction, PCI: percutaneous coronary intervention, LVEF: left ventricular ejection fraction, CK-MB: creatine kinase-MB, LDL-C: low density lipoprotein cholesterol, Hs CRP: high sensitivity C-reactive protein, NT pro BNP: N-terminal pro-brain natriuretic peptide, HbA1c: hemoglobin A1C, LMWH: low molecular weight heparin, RAAS: rennin angiotensin aldosterone system
Table 2
Comparison of clinical baseline characteristics after propensity score matching in group C (HDL-C<40 mg/dL and TG<150 mg/dL) and group D (HDL-C<40 mg/dL and TG≥150 mg/dL)

Values are n (%) or mean±standard deviation. HDL-C: high density lipoprotein cholesterol, TG: triglyceride, BMI: body mass index, SBP: systolic blood pressure, DBP: diastolic blood pressure, HR: hazard ratio, IHD Hx.: ischemic heart disease history, HTN: hypertension, DM: diabetes mellitus, HL: hyperlipidemia, MI: myocardial infarction, STEMI: ST-segment elevation myocardial infarction, NSTEMI: non-ST segment elevation myocardial infarction, PCI: percutaneous coronary intervention, LVEF: left ventricular ejection fraction, CK-MB: creatine kinase-MB, LDL-C: low density lipoprotein cholesterol, Hs CRP: high sensitivity C-reactive protein, NT pro BNP: N-terminal pro-brain natriuretic peptide, HbA1c: hemoglobin A1C, LMWH: low molecular weight heparin, RAAS: rennin angiotensin aldosterone system
Table 3
Comparison of coronary angiographic and procedural characteristics after propensity score matching in group A (HDL-C≥40 mg/dL and TG<150 mg/dL) and group B (HDL-C≥40 mg/dL and TG≥150 mg/dL)
Values are n (%) or mean±standard deviation. HDL-C: high density lipoprotein cholesterol, TG: triglyceride, TIMI: thromboysis in myocardial infarction, LM: left main, LAD: left anterior descending artery, LCX: left circumflex artery, RCA: right coronary artery, BMS: bare metal stent, DES: drug-eluting stent
Table 4
Comparison of angiographic and procedural characteristics after propensity score matching in group C (HDL-C<40 mg/dL and TG<150 mg/dL) and group D (HDL-C<40 mg/dL and TG≥150 mg/dL)
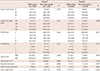
Table 5
The impact of statin therapy on primary end point after propensity score matching

The covariates in this multivariate analysis were age over 65 years, hypertension, diabetes mellitus, left ventricular ejection fraction, Killip classification, post-TIMI flow, and the use of aspirin, clopidogrel, beta-blocker, and renin-angiotensin system blocker. TIMI: thrombolysis in myocardial infaction, HR: hazard ratio, CI: confidence interval




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download