Abstract
Purpose
The aim of this study was to determine the predictive factors for maternal role development for mothers of premature infants.
Methods
A descriptive correlational study was conducted. A total sample of 121 mothers of premature infants following discharge from the neonatal intensive care unit were recruited using two strategies; an internet-based survey and an in-person data collection in a tertiary university hospital in Korea. A self-report questionnaire was used to collect data regarding personal, birth variables, marital intimacy, maternal attachment, maternal identity and maternal role development.
Results
A hierarchical multiple regression analysis indicated that parity, maternal attachment, marital intimacy and maternal identity were predictors for maternal role development for mothers of premature infants, accounting for 70% of the variance. Among these variables, maternal attachment is the most powerful predictor for maternal role development.
Conclusion
Nursing interventions during hospitalization to post-discharge education that includes parents of premature babies with positive interaction between couples strengthening marital intimacy and promotes maternal attachment that leads to integrate maternal identity should be considered by priority. Community-based family services such as home visits should be focused on maximizing the predictive factors for maternal role development in transition to motherhood that can contribute to maternal health as well as optimal growth and development of premature infants.
Figures and Tables
Figure 1
Maternal role development model among NICU graduate mothers of premature infants based on Mercer's becoming a mother theory.

Table 1
Maternal Attachment, Maternal Identity, Marital Intimacy and Maternal Role Development according to Subjects' Characteristics (N=121)

Table 2
Relationships of Characteristics of Mothers and Premature Infants with Study Variables (N=121)
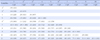
Table 3
Factors associated with Maternal Role Development in Mothers of Premature Infants Obtained by Hierarchical Multiple Analysis (N=121)

Summary Statement
▪ What is already known about this topic?
Although maternal role development has significant effects on infant's optimal growth and development, little understanding has been given to associated factors of maternal role development among mothers of premature infant in the transition from hospital to their own home environment.
▪ What this paper adds?
Maternal attachment, maternal identity and marital intimacy are correlated and found as predictors for maternal role development in neonatal intensive care unit graduate mothers of premature infants. Maternal attachment is the most powerful predictor of maternal role development.
▪ Implications for practice, education and/or policy
Sustainable community-based family nursing interventions for developmentally supportive care includes assessment of attachment between mother and infant dyads with marital relationship quality for mothers of premature infants need to be developed.
References
1. Statistics Korea. 2013 Birth certificate data [Internet]. Seoul: Statistics Korea;2014. cited 2014 December 1. Available from: http://kostat.go.kr/portal/korea/kor_nw/3/index.board?bmode=read&aSeq=329406&pageNo=&rowNum=10&amSeq=&sTarget=&sTxt=0.
2. Tooten A, Hoffenkamp HN, Hall RA, Braeken J, Vingerhoets AJ, van Bakel HJ. Parental perceptions and experiences after childbirth: A comparison between mothers and fathers of term and preterm infants. Birth. 2013; 40(3):164–171.

3. Altimier L, Phillips RM. The Neonatal Integrative Developmental Care Model: Seven neuroprotective core measures for family-centered developmental care. Newborn Infant Nurs Rev. 2013; 13(1):9–22.

4. Lopez GL, Anderson KH, Feutchinger J. Transition of premature infants from hospital to home life. Neonatal Netw. 2012; 31(4):207–214.

5. Hane AA, Myers MM, Hofer MA, Ludwig RJ, Halperin MS, Austin J, et al. Family nurture intervention improves the quality of maternal caregiving in the neonatal intensive care unit. J Dev Behav Pediatr. 2015; 36(3):188–196.

6. Bae CW, Shim KS, Hahn WH, Kim KS, Kim BI, Shin SM, et al. Rehospitalization rate and medical cost of infants in the first year after discharge from neonatal intensive care units. J Korean Soc Neonatol. 2010; 17(1):13–20.
7. Boykova M, Kenner C. Transition from hospital to home for parents of preterm infants. J Perinat Neonatal Nurs. 2012; 26(1):81–87.

8. Pisoni C, Garofoli F, Baiardini I, Tzialla C, Stronati M. The development of parents-infant relationship in high-risk pregnancies and preterm birth. J Pediatr and Neonatal Individual Med. 2014; 3(2):e030233.
9. Im M, Oh J. Integrative review on caring education papers for parents with a premature infant. Child Health Nurs Res. 2013; 19(2):120–129.

10. Miles MS, Holditch-Davis D, Burchinal MR, Brunssen S. Maternal role attainment with medically fragile infants: Part 1. Measurement and correlates during the first year of life. Res Nurs Health. 2011; 34(1):20–34.

11. Holditch-Davis D, Miles MS, Burchinal MR, Goldman BD. Maternal role attainment with medically fragile infants: Part 2. Relationship to the quality of parenting. Res Nurs Health. 2011; 34(1):35–48.

12. Pennestri MH, Gaudreau H, Bouvette-Turcot AA, Moss E, Lecompte V, Atkinson L, et al. Attachment disorganization among children in neonatal intensive care unit: Preliminary results. Early Hum Dev. 2015; 91(10):601–606.

13. Mercer RT. Becoming a mother versus maternal role attainment. J Nurs Scholarsh. 2004; 36(3):226–232.

14. Emmanuel EN, Creedy DK, St John W, Brown C. Maternal role development: The impact of maternal distress and social support following childbirth. Midwifery. 2011; 27(2):265–272.

15. Ngai FW, Wai-Chi Chan S, Ip WY. Predictors and correlates of maternal role competence and satisfaction. Nurs Res. 2010; 59(3):185–193.

16. Liu CC, Chen YC, Yeh YP, Hsieh YS. Effects of maternal confidence and competence on maternal parenting stress in newborn care. J Adv Nurs. 2012; 68(4):908–918.

17. Song JE, Ahn JA. Effect of intervention programs for improving maternal adaptation in Korea: Sytematic review. Korean J Women Health Nurs. 2013; 19(3):129–141.
18. Chon MY, Ji ES, Lee SH. Mothers' parenting experience of premature infants: Q methodological approach. J Korean Acad Nurs. 2013; 43(6):704–713.

19. Mercer RT. The process of maternal role attainment over the first year. Nurs Res. 1985; 34(4):198–204.

21. Lindblom J, Flykt M, Tolvanen A, Vänskä M, Tiitinen A, Tulppala M, et al. Dynamic family system trajectories from pregnancy to child's first year. J Marriage Fam. 2014; 76(4):796–807.

22. Jung YY, Kim HW. Factors associated with postpartum depression and its influence on maternal identity. Korean J Women Health Nurs. 2014; 20(1):29–37.

23. Kang H, Yeon K, Han ST. A Review on the use of effect size in nursing research. J Korean Acad Nurs. 2015; 45(5):641–649.

24. Pridham KF, Chang AS. What being the parent of a new baby is like: Revision of an instrument. Res Nurs Health. 1989; 12(5):323–329.

25. Choi HS, Shin YH. Effects on maternal attachment, parenting stress, and maternal confidence of systematic information for mothers of premature infants. Child Health Nurs Res. 2013; 19(3):207–215.

26. Walker LO. Investigating the semantic properties of two concepts. The University of Texas at Austin;1977. Unpublished manuscript paper.
27. Lee KH. A measure of marital intimacy. Fam Environ Res. 1995; 33(4):235–249.
28. Ha JY, Kim YJ. Factors influencing self-confidence in the maternal role among early postpartum mothers. Korean J Women Health Nurs. 2013; 19(1):48–56.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download