Abstract
Purpose
This study was to assess the intention of undergoing Pap testing and to identify influencing factors of HPV knowledge and their attitude related to Pap test by sexual activity among unmarried nurses.
Methods
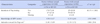
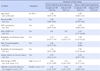
A cross sectional survey design was employed, utilizing a self-administered questionnaire amongst 343 unmarried nurses. Descriptive statistics was utilized to analyze data and inferential statistics used an independent-t test and χ2 test for the differences in measurement variables, and odds ratios for factors on intention of Pap testing by sexual activity.
Results
Nurses not sexually active were significantly higher in intention of Pap testing (χ2=40.15, p<.001) and influencing factors of HPV knowledge (t=3.93, p=.048) than did nurses who were sexually active. Factors influencing intention were regularity of the breast self-examination (Adjusted Odds Ratio [AOR]=4.20, 95% Confidence Interval [CI]=1.93~9.17), HPV knowledge (AOR=2.49, 95% CI=1.36~4.56), and attitudes toward the Pap test(AOR=2.33, 95% CI=1.25~4.34) amongst nurses who never had sexual experience.
Conclusion
It is necessary to minimize negative attitudes of Pap testing and to increase HPV knowledge in order to improve intention of Pap testing for women who were not sexually active. More focus would be given to sexually active women to get Pap tested as a preventive measure for cervical cancer.
Figures and Tables
Summary Statement
▪ What is already known about this topic?
Intention of Pap testing amongst unmarried women should be encouraged in order to prevent cervical cancer in Korea. Pap testing rates amongst Korean nurses who were married was not satisfactory.
▪ What this paper adds?
Intention of Pap testing and influencing factors of HPV knowledge were lower in the sexually active unmarried nurses than did for those who were not sexually active in Korea. Factors influencing intention of Pap testing were HPV knowledge and attitude toward Pap testing amongst nurses who were not sexually active.
▪ Implications for practice, education and/or policy
Focus should be given to sexually active unmarried women in order to enhance HPV knowledge and promotion of preventive practice of Pap test.
References
1. Ali SF, Ayub S, Manzoor NF, Azim S, Afif M, Akhtar N, et al. Knowledge and awareness about cervical cancer and its prevention amongst interns and nursing staff in tertiary care hospitals in Karachi, Pakistan. PLoS One. 2010; 5(6):e11059.

2. Urasa M, Darj E. Knowledge of cervical cancer and screening practices of nurses at a regional hospital in Tanzania. Afr Health Sci. 2011; 11(1):48–57.
3. Lee MH, Lim EJ, Yu YH, Jun MH. Clinical nurses's HPV-related knowledge and perception of cancer causes: HPV vaccinated vs. not vaccinated. Korean J Women Health Nurs. 2011; 17(1):1–9.
4. Kelaher M, Gillespie AG, Allotey P, Manderson L, Potts H, Sheldrake M, et al. The transtheoretical model and cervical screening: Its application among culturally diverse communities in Queensland, Australia. Ethn Health. 1999; 4(4):259–276.

5. Turkistanli EC, Sogukpınar N, Saydam BK, Aydemir G. Cervical cancer prevention and early detection-the role of nurses and midwives. Asian Pac J Cancer Prev. 2003; 4(1):15–21.
6. Makwe CC, Anorlu RI. Knowledge of and attitude toward human papillomavirus infection and vaccines among female nurses at a tertiary hospital in Nigeria. Int J Womens Health. 2011; 3:313–317.

7. Wamai RG, Ayissi CA, Oduwo GO, Perlman S, Welty E, Welty T, et al. Awareness, knowledge and beliefs about HPV, cervical cancer and HPV vaccines among nurses in Cameroon: An exploratory study. Int J Nurs Stud. 2013; 50(10):1399–1406.

8. Beydag KD. Knowledge and applications of the midwives and nurses at an educational hospital on the early diagnosis of cervix cancer. Asian Pac J Cancer Prev. 2011; 12(2):481–485.
9. Choe SA. Factors influencing continuous Pap smear participation in women employed in a general hospital [master's thesis]. 2002. Seoul: Yonsei University.
10. Ju HO, Kim JS, Cho YS, Park NH, Eo YS, Cho YR, et al. A survey on cancer screening among nurses at general hospital in Busan. Korean J Women Health Nurs. 2003; 9(1):18–27.

11. Kim HW, Jung YY. Relating factors in Pap smears by stage of change among married nurses. Korean J Women Health Nurs. 2010; 16(4):317–325.
12. Denny-Smith T, Bairan A, Page MC. A survey of female nursing students' knowledge, health beliefs, perceptions of risk, and risk behaviors regarding human papillomavirus and cervical cancer. J Am Acad Nurse Pract. 2006; 18(2):62–69.

13. Kim HW. Awareness of Pap testing and factors associated with intent to undergo Pap testing by level of sexual experience in unmarried university students in Korea: Results from an online survey. BMC Womens Health. 2014; 14:100.

14. Kim HW. Effects of prevention education on Human Papillomavirus linked to cervix cancer for unmarried female university students. J Korean Acad Nurs. 2009; 39(4):490–498.

15. Kim HW, Ko GY. Evaluation of Korean version of the beliefs about Papanicolau test and cervical cancer in unmarried university students. Korean J Women Health Nurs. 2013; 19(1):13–22.

16. Park SJ, Park WS. Identifying barriers to Papanicolaou smear screening in Korean women: Korean National Health and Nutrition Examination Survey 2005. J Gynecol Oncol. 2010; 21(2):81–86.

17. National Cancer Information Center. Cancer prevention and screening [Internet]. Seoul: National Cancer Center;2013. cited 2013 October 28. Available from: http://www.cancer.go.kr/mbs/cancer/subview.jsp?id=cancer_010202000000.
18. Kim HW, Ahn HY. Study on the knowledge of human papillomavirus in female university students. Korean J Women Health Nurs. 2007; 13(1):13–20.
19. Cho EJ, Chung BY. A descriptive study on women's embarrassability and embarrassment during cervical screening. J Korean Acad Nurs. 2002; 32(6):832–843.
20. Kim M, Park Y. Knowledge, attitude, and practice of obstetric nurses in relation to breast cancer and breast self examination. Korean J Women Health Nurs. 2011; 17(1):88–98.
21. The Korean Nurses. Comparisons of the nursing workforce in South Korea and United States [Internet]. Seoul: Korean Nurses Association;2003. cited 2013 October 25. Available from: http://webzine.koreanurse.or.kr/Webzine/read_article.php?webzine_id=2&sub_cat_id=24&is_sub_no=37&article_id=60.
22. Ministry of Health and Welfare. Ministry of Health and Welfare statistical yearbook 2013. Seoul: Gyemoonsa;2013. Volume 59:p. 162.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download