Abstract
Background
For surgical treatment of lumbar and lumbosacral tuberculosis, the anterior approach has been the most popular approach because it allows direct access to the infected tissue, thereby providing good decompression. However, anterior fixation is not strong, and graft failure and loss of correction are frequent complications. The posterior approach allows circumferential decompression of neural elements along with three-column fixation attained via pedicle screws by the same approach. The purpose of this study was to evaluate the outcome (functional, neurological, and radiological) in patients with lumbar and lumbosacral tuberculosis operated through the posterior approach.
Methods
Twenty-eight patients were diagnosed with tuberculosis of the lumbar and lumbosacral region from August 2012 to August 2013. Of these, 13 patients had progressive neurological deterioration or increasing back pain despite conservative measures and underwent posterior decompression and pedicle screw fixation with posterolateral fusion. Antitubercular therapy was given till signs of radiological healing were evident (9 to 16 months). Functional outcome (visual analogue scale [VAS] score for back pain), neurological recovery (Frankel grading), and radiological improvement were evaluated preoperatively, immediately postoperatively and 3 months, 6 months, and 1 year postoperatively.
Results
The mean VAS score for back pain improved from 7.89 (range, 9 to 7) preoperatively to 2.2 (range, 3 to 1) at 1-year follow-up. Frankel grading was grade B in 3, grade C in 7, and grade D in 3 patients preoperatively, which improved to grade D in 7 and grade E in 6 patients at the last follow-up. Radiological healing was evident in the form of reappearance of trabeculae formation, resolution of pus, fatty marrow replacement, and bony fusion in all patients. The mean correction of segmental kyphosis was 9.85° postoperatively. The mean loss of correction at final follow-up was 3.15°.
According to the World Health Organization's Global tuberculosis report 2015, tuberculosis now ranks alongside human immunodeficiency virus (HIV) as a leading cause of death worldwide with 1.4 million deaths in 2014.1) Spine is the most common site for osseous involvement of tuberculosis accounting for around 50% of musculoskeletal tuberculosis cases.2) Thoracic spine is most commonly affected and involvement of lumbar and lumbosacral region is less common.34) With advent of magnetic resonance imaging (MRI), early detection of disease is possible and effective antitubercular therapy has allowed disease cure in majority of patients with conservative management lone.5) However, surgery is indicated in patients having disabling back pain and or progressive neurological deficit despite conservative management.56)
Traditionally, surgical management of lumbar and lumbosacral tuberculosis has always been through anterior route because the anterior approach allows direct access to infected tissue, thereby providing good decompression.5) However, anterior fixation is not strong, and graft failure and loss of correction are frequent complications.6) In addition, it is a difficult approach in lumbar or lumbosacral spine due to the presence of iliac vessels anterolaterally.6) Posterior approach allows circumferential decompression of neural elements along with three-column fixation attained via pedicle screws by the same approach.56) The present study aims to evaluate the results (functional, neurological, and radiological) of the posterior approach in patients operated for lumbar and lumbosacral tuberculosis.
A total of 31 patients were diagnosed with lumbar and lumbosacral tuberculosis from August 2012 to August 2013 based upon radiological findings (MRI) and histopathology reports (sample obtained by computed tomography [CT] guided biopsy). All were started on antitubercular therapy. Of these, 13 patients developed progressive neurological deterioration or increasing back pain despite conservative measures and underwent posterior decompression and pedicle screw fixation and posterolateral fusion. Our analysis was centred upon these 13 patients managed surgically. There were 8 males and 5 females and their mean age at the time of surgery was 35.2 years (range, 22 to 55 years). The mean duration of symptoms was 4 months (range, 2 to 7 months). Indication of surgical procedure was intolerable back pain and/or progressive neurological deficit despite ongoing conservative management.
A complete blood count, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), Mantoux test, plain radiography of the lumbosacral spine (anteroposterior and lateral views), and MRI were carried out in all patients.
Under general anaesthesia, the midline posterior approach was used with the patient placed in prone position in all cases. Laminectomy or laminotomy was done at the affected levels and pedicle screw fixation was done cephalad and caudad including healthy pedicles of the affected vertebrae (Table 1). Decompression involved only removal of tissue compressing neural structures. Extensive anterior debridement was avoided. Posterolateral fusion was done in all cases. Infected material was sent for histopathological examination and culture sensitivity.
Log roll, side turning, and pelvic lift exercises were started on postoperative day one and mobilization with the support of lumbosacral belt was started as early as possible. Antitubercular chemotherapy was continued till radiological healing of the lesion was evident.
Mean hospital stay was 9 days (range, 7 to 14 days) and suture removal was done on postoperative day 13 in all except 1 case with superficial infection (postoperative day 17).
Functional outcome (visual analogue scale [VAS] for back pain),7) neurological recovery (Frankel grading),8) and segmental kyphosis (on plain radiographs) were assessed preoperatively and at 3, 6, and 12 months following surgery. In all patients, MRI was done every 4 months postoperatively till signs of radiological healing were evident. Segmental kyphotic angle was measured as the angle between caudal and cephalad end plates nearest to the lesion.
Preoperatively, the ESR was elevated in 8 cases (61.5%) and the CRP level in 10 cases (76.90%). The ESR returned to normal in 6 cases by 3 months postoperatively. Normal values of ESR were attained in all 8 patients at final follow-up. The CRP level had fallen to normal values in all the 10 cases at the end of 3 months after surgery. The Mantoux test was positive in 6 cases (46.15%) and histopathology reports demonstrated tubercular osteomyelitis in all 13 cases with presence of typical caseating granulomas. However, culture was positive only in 5 cases (38.46%).
The mean VAS score for back pain improved from 7.89 (range, 9 to 7) preoperatively to 2.2 (range, 3 to 1) at final follow-up (Table 2). Frankel grading was grade B in 3, grade C in 7, and grade D in 3 patients preoperatively, which improved to grade D in 7 and grade E in 6 patients at last follow-up (Table 3). Radiological healing was evident in the form of reappearance of trabeculae formation, resolution of pus, fatty marrow replacement, and bony fusion on sequential follow-ups in all cases (Figs. 1 and 2). All except 1 patient healed at 1-year follow-up. One patient had a pocket of pus in the psoas muscle and healed at the end of 17 months postoperatively. The mean correction of segmental kyphosis was 9.85° (range, 9° to 14°) postoperatively. The mean loss of correction at final follow-up was 3.15° (range, 1° to 8°) (Table 4).
Based on current evidence, spinal tuberculosis can be considered a medical condition that requires operative treatment only in the presence of neurological deficits caused by spinal cord compression, disabling back pain, and spinal deformity in spite of ongoing antitubercular therapy.2569) The surgical approach in spinal tuberculosis has evolved from anterior to posterior. The anterior approach, popularised by Hodgson et al.10) in 1960, was advocated traditionally in view of the predilection of the pathology of tuberculosis for the vertebral bodies and disc spaces. The anterior approach concedes direct access to the infected focus and is convenient for debriding infection and reconstructing the defect.1112) In the lumbar region, attainment of bony stability through anterior instrumentation may be insubstantial due to presence of the concomitant osteoporosis associated with infection of tuberculosis that renders the vertebrae structurally weak and thereby preventing adequate fixation.1314) Also, anterior fixation is not feasible in the lumbar and lumbosacral spine due to the presence of the common iliac vessels anterolaterally.15)
A combined anterior plus posterior approach helps to overcome stability-related drawbacks of the anterior approach alone.13141516) However, it involves 2 surgeries (it can be a single event or performed as a staged procedure), and when performed as a single event, it is associated with increased operative time and blood loss along with exposure of vital structures such as peritoneum in already immunocompromised tuberculosis patients, leading them susceptible to further infection and thus contributing to further additional morbidity.6) Campbell et al.17) have reported higher rates of complications with isolated anterior fixation and combined anterior and posterior spinal fusion in comparison to isolated posterior fusion.
Recently, the posterior approach has gained popularity because it is less invasive, allows circumferential cord decompression, can be extended proximally and distally from the involved segment, and provides a stronger three-column fixation through uninvolved posterior elements via pedicle screws.161819) In 2005, Bezer et al.20) reported transpedicular drainage and posterior instrumentation as a less demanding single-stage procedure in patients with lumbosacral tuberculosis.
Functional recovery evaluated in terms of VAS in our study was comparable to that of Sahoo et al.21) with a mean value of 1.9 at the end of 1-year follow-up. The majority of the patients were pain-free at final follow-up. Significant improvement in neurological grading was evident with an improvement of two grades in more than 50% of the cases. Evaluation of radiological healing in cases of spinal tuberculosis has been described by Jain et al.22) as the remineralization and reappearance of bony trabeculae, sharpening of the articular and cortical margin, sclerosis of the vertebral body and end plates, fusion of vertebral bodies on plain X-rays, resolution of enhanced vertebral body on MRI, and paravertebral collection and fatty replacement of marrow seen as enhanced intensity on sequential T1 and T2 images. These findings were evident in our study on radiological scans performed at regular intervals. In the present study, the loss of correction at final follow-up was 3.15°, which was not statistically significant (p > 0.05). This was consistent with the findings of Zhang et al.23) Recently, percutaneous posterior fixation with or without anterior debridement has been published.2425) Only posterior fixation was done for patients with back pain only. Patients with neurological involvement underwent anterior debridement in addition, thus having complications associated with anterior approach. In our study, decompression was required in all patients thus ruling out the option of percutaneous fixation.
In conclusion, single-stage posterior decompression and instrumented fusion is an effective and safe procedure for surgical treatment of lumbar and lumbosacral tuberculosis in adults. Further studies with a large number of patients and a longer follow-up will be necessary.
Figures and Tables
Fig. 1
(A) Preoperative sagittal T2-weighted magnetic resonance imaging scan showing L4–L5 spondylodiscitis with epidural soft tissue compressing the cauda equina. (B) Follow-up sagittal T2-weighted magnetic resonance imaging scan obtained at 1-year after surgery showing radiological healing (disappearance of soft tissue and fatty marrow conversion).
Fig. 2
(A) Preoperative plain radiograph showing destruction of L4 body and end plate with reduction of L3–L4 disc space and segmental kyphosis of 23°. (B) Follow-up radiograph at 1-year after surgery showing sclerosis at the affected level and pedicle screws with segmental kyphosis of 14°.

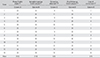
Table 1
Number of Vertebrae Affected and Number of Levels Fixed
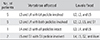
Table 2
Mean Visual Analogue Scale Scores of 13 Patients at Serial Follow-ups
| Follow-up duration | Visual analogue scale score |
|---|---|
| Preoperative | 7.9 |
| Immediate postoperative | 3.2 |
| Postoperative (mo) | |
| 3 | 2.8 |
| 6 | 2.3 |
| 12 | 1.9 |
| 18 | 1.6 |
| 24 | 1.5 |
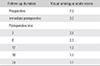
Table 3
Frankel Grading
| Frankel grading | Preoperative | Final follow-up |
|---|---|---|
| Grade A | 0 | 0 |
| Grade B | 3 (23.08) | 0 |
| Grade C | 7 (53.84) | 0 |
| Grade D | 3 (23.08) | 7 (53.84) |
| Grade E | 0 | 6 (46.16) |
| Total | 13 (100) | 13 (100) |
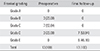
Table 4
Segmental Kyphotic Angles at Serial Follow-ups
References
1. World Health Organization. Global tuberculosis report 2015. 20th ed. Geneva: World Health Organization;2015.
2. Trecarichi EM, Di Meco E, Mazzotta V, Fantoni M. Tuberculous spondylodiscitis: epidemiology, clinical features, treatment, and outcome. Eur Rev Med Pharmacol Sci. 2012; 16:Suppl 2. 58–72.
3. Turgut M. Spinal tuberculosis (Pott's disease): its clinical presentation, surgical management, and outcome. A survey study on 694 patients. Neurosurg Rev. 2001; 24(1):8–13.

4. Nussbaum ES, Rockswold GL, Bergman TA, Erickson DL, Seljeskog EL. Spinal tuberculosis: a diagnostic and management challenge. J Neurosurg. 1995; 83(2):243–247.

5. Lee TC, Lu K, Yang LC, Huang HY, Liang CL. Transpedicular instrumentation as an adjunct in the treatment of thoracolumbar and lumbar spine tuberculosis with early stage bone destruction. J Neurosurg. 1999; 91:2 Suppl. 163–169.

6. Zaveri G. The role of posterior surgery in spinal tuberculosis. ArgoSpine News J. 2011; 23(3):112–119.

8. Frankel HL, Hancock DO, Hyslop G, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia: I. Paraplegia. 1969; 7(3):179–192.

9. Khoo LT, Mikawa K, Fessler RG. A surgical revisitation of Pott distemper of the spine. Spine J. 2003; 3(2):130–145.

10. Hodgson AR, Stock FE, Fang HS, Ong GB. Anterior spinal fusion: the operative approach and pathological findings in 412 patients with Pott's disease of the spine. Br J Surg. 1960; 48(208):172–178.

11. Benli IT, Kaya A, Acaroglu E. Anterior instrumentation in tuberculous spondylitis: is it effective and safe? Clin Orthop Relat Res. 2007; 460:108–116.
12. Jain AK, Dhammi IK, Prashad B, Sinha S, Mishra P. Simultaneous anterior decompression and posterior instrumentation of the tuberculous spine using an anterolateral extrapleural approach. J Bone Joint Surg Br. 2008; 90(11):1477–1481.

13. Hee HT, Majd ME, Holt RT, Pienkowski D. Better treatment of vertebral osteomyelitis using posterior stabilization and titanium mesh cages. J Spinal Disord Tech. 2002; 15(2):149–156.

14. Krodel A, Kruger A, Lohscheidt K, Pfahler M, Refior HJ. Anterior debridement, fusion, and extrafocal stabilization in the treatment of osteomyelitis of the spine. J Spinal Disord. 1999; 12(1):17–26.
15. Fukuta S, Miyamoto K, Masuda T, et al. Two-stage (posterior and anterior) surgical treatment using posterior spinal instrumentation for pyogenic and tuberculotic spondylitis. Spine (Phila Pa 1976). 2003; 28(15):E302–E308.

16. Moon MS, Woo YK, Lee KS, Ha KY, Kim SS, Sun DH. Posterior instrumentation and anterior interbody fusion for tuberculous kyphosis of dorsal and lumbar spines. Spine (Phila Pa 1976). 1995; 20(17):1910–1916.

17. Campbell PG, Malone J, Yadla S, et al. Early complications related to approach in thoracic and lumbar spine surgery: a single center prospective study. World Neurosurg. 2010; 73(4):395–401.

18. Moon MS. Combined posterior instrumentation and anterior interbody fusion for active tuberculous kyphosis of the thoraco-lumbar spine. Orthop Trauma. 1991; 5(3):177–179.

19. Sundararaj GD, Behera S, Ravi V, Venkatesh K, Cherian VM, Lee V. Role of posterior stabilisation in the management of tuberculosis of the dorsal and lumbar spine. J Bone Joint Surg Br. 2003; 85(1):100–106.

20. Bezer M, Kucukdurmaz F, Aydin N, Kocaoglu B, Guven O. Tuberculous spondylitis of the lumbosacral region: long-term follow-up of patients treated by chemotherapy, transpedicular drainage, posterior instrumentation, and fusion. J Spinal Disord Tech. 2005; 18(5):425–429.
21. Sahoo MM, Mahapatra SK, Sethi GC, Dash SK. Posterior-only approach surgery for fixation and decompression of thoracolumbar spinal tuberculosis: a retrospective study. J Spinal Disord Tech. 2012; 25(7):E217–E223.
22. Jain AK, Srivastava A, Saini NS, Dhammi IK, Sreenivasan R, Kumar S. Efficacy of extended DOTS category I chemotherapy in spinal tuberculosis based on MRI-based healed status. Indian J Orthop. 2012; 46(6):633–639.

23. Zhang H, Sheng B, Tang M, et al. One-stage surgical treatment for upper thoracic spinal tuberculosis by internal fixation, debridement, and combined interbody and posterior fusion via posterior-only approach. Eur Spine J. 2013; 22(3):616–623.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download