Abstract
Background
This study aimed to evaluate the clinical and radiological outcomes of arthroscopic bioabsorbable screw fixation in osteochondritis dissecans (OCD) in adolescent patients with unstable lesions causing pain.
Methods
The study included 11 patients (10 males and 1 female) with OCD who underwent arthroscopic bioabsorbable screw fixation between July 2007 and February 2014 and were available for follow-up for more than 12 months. The mean age at diagnosis was 16.3 years (range, 11 to 19 years), and the average follow-up period was 51 months (range, 12 to 91 months). Clinical results were evaluated using the Knee Injury and Osteoarthritis Outcome Score (KOOS), Lysholm knee score, and International Knee Documentation Committee (IKDC) score measured before surgery and at follow-up. Functional evaluation was made using the Tegner activity scale. Magnetic resonance imaging (MRI) and second-look arthroscopy were performed at the 12-month follow-up.
Results
Between the preoperative assessment and follow-up, improvements were seen in the KOOS (range, 44.9 to 88.1), Lysholm knee score (range, 32.6 to 82.8), and IKDC score (range, 40.8 to 85.6). The Tegner activity scale also improved from 2.8 to 6.1. Based on postoperative MRI, there were eight Dipaola grade I cases and three grade II cases. No complications due to fixation failure developed in any case. Second-look arthroscopy at 12 months postoperatively revealed that the lesion was covered with cartilage in all cases.
Osteochondritis dissecans (OCD) is an increasingly common cause of knee pain and dysfunction among skeletally immature and young adult patients. Operative treatment is indicated for any detached or unstable lesions in which physeal closure is imminent or completed, and nonoperative management has failed. In the case of adult OCD, which will generally have a poor prognosis,1) surgical intervention is necessary. The treatment of symptomatic lesions in OCD of the knee is difficult, particularly in young patients who wish to maintain a high degree of sports activity.2345) Management of OCD in a young patient is multifaceted. Initial nonoperative management is indicated for stable lesions in skeletally immature patients.6)
The nonoperative management requires long periods of rest and the avoidance of sports.2345) Traditional OCD lesion fixation employed metal implants, including Herbert and other screws, various types of pins, and metal staples.678) Depending on the implant configuration and the method of application, compression may be achievable. However, such implants generally require removal after healing because of the potential for joint damage from prominent hardware, which may result in complications.8)
Current surgical treatments for OCD of the knee joint include arthroscopic multiple drilling, open or endoscopic fixation by screws, and autologous cartilage implantation. Recently treatments using biodegradable rods have been suggested.9)
The treatment method is determined by the patient's growth plate and the stability of the lesion itself.1011) This study attempted to evaluate clinical results, magnetic resonance imaging (MRI), and second-look arthroscopic findings of arthroscopic bioabsorbable screw fixation performed on painful, unstable OCD in adolescents.
This study was approved by the Ethics Committee of the Institutional Review Board (IRB No.: WKUHIRB 201505-HRE-031). Eleven patients, 10 males and 1 female, ranging in age from 11 to 19 years (average age of 16.3 years), who were diagnosed with OCD and underwent arthroscopic bioabsorbable screw fixation in our clinic from July 2007 to February 2014 were enrolled in this study. The preoperative MRI examinations showed that seven patients had lesions on the medial femoral condyle and four had lesions on the lateral femoral condyle. Lesion sizes ranged from 1.2 cm2 to 5.0 cm2 with an average of 3.19 cm2 (Table 1). The postoperative follow-up period on all patients ranged from 12 months to 91 months with an average of 51 months.
Symptoms with less than a few months duration were regarded as acute. The average period of symptom persistence was 13 months (range, 2 months to 3 years). Six of 11 cases were clearly related to trauma with three patients suffering from a fall, two from a motor vehicle accident, and one from a soccer accident. The remaining five patients had minor traumatic histories, but no specific causes could be identified.
In this study, surgery was performed on grade II, III OCD lesions if the patients who had symptoms were adolescents. Grade I, IV OCD lesions were excluded in this study because a different treatment method such as autogenous bone graft was considered preferable. Surgery was also excluded when multiple injuries such as ligament injury or epiphyseal plate closure was present.
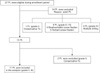
Fig. 1 provides a flow diagram for the patients evaluated for this study. The surgeons in this study performed a total of 27 arthroscopic screw fixations from July 2007 to February 2014. Fourteen patients were excluded because they were adult patients. One adult patient with grade I lesions among the 14 adult patients was treated conservatively. Of nine patients with grade II, III lesions, four of them underwent bioabsorbable screw fixation, and five underwent Herbert screw fixation. Multiple drilling was conducted for four patients with grade IV lesions. Two adolescent patients with grade I lesions among the 13 adolescent patients were treated conservatively. Eleven patients (40.7%) consented to participate (Fig. 1).
For clinical evaluation of the knee joint, the Knee injury and Osteoarthritis Outcome Score (KOOS), Lysholm knee score, and International Knee Documentation Committee (IKDC) score were measured before surgery and at the final follow-up, and the Tegner activity scale score was determined for functional evaluation. Preoperative and at postoperative 12 month follow-up, plain radiographs (anteroposterior view, lateral view, intercondylar notch view, skyline view) and MRI were performed, and the lesions were classified as described by Dipaola et al.12) Cases with articular cartilage thickening and no separation were classified as stage I; cases with articular cartilage separation with fiber attachment were classified as stage II; and cases with articular cartilage separation with synovial fluid behind the lesion were classified as stage III. Finally, vitreous body formation within the cartilage was classified as stage IV. At the follow-up MRI examination, comparison with the peripheral normal cartilage and conformity of the articular surface were assessed.
At initial operation and second-look arthroscopy, a probe was inserted through the arthroscopic portal to evaluate the instability of the lesion, and the lesion was classified according to the arthroscopic classification by Guhl.13) When irregular articular cartilage and softening were observed, the lesion was classified as stage I, and lesions separated without articular cartilage dislocation were classified as stage II. Lesions separated by accompanying articular cartilage dislocation were classified as stage III, and cases of vitreous body and articular cartilage loss were classified as stage IV.
A second arthroscopic examination was performed with patient consent 12 months after the initial surgery to check whether the OCD lesion was healed, if it matched the follow-up MRI, and to assess the condition of the articular surface in the area of the surgery and the continuity with the peripheral cartilage. Second-look arthroscopy was performed with the consent of the patient and the parent/guardian of adolescent patients with the epiphyseal plate still open.
According to the classification of Dipaola et al.,12) at preoperative MRI, four cases were grade II, and seven were grade III. Instability of lesions was evaluated with a probe intraoperatively with arthroscopy. Five cases had grade II lesions, and six cases had grade III lesions according to Guhl13)'s arthroscopic classification (Table 2).
Analysis of the results was done by using Wilcoxon signed-rank test of SPSS 13.0 ver. (SPSS Inc., Chicago, IL, USA). A p-value less than 0.05 was considered statistically significant.
After first performing arthroscopic examination in all cases, a probe was advanced to the lesion to determine its size and stability. The flexion angle of the knee joint was then adjusted manually, and bioabsorbable screws (Arthrex, Naples, FL, USA) composed of poly-L-lactic acid were used to perform the fixation. At least two bioabsorbable screws were used, and screw size was chosen between 2.5 mm × 18 mm and 3.0 mm × 18 mm depending on the size of the lesion. Here, the drill guide was located vertically on the lesion as much as possible, and the bioabsorbable screw was inserted vertically to provide axial pressure. Two or more bioabsorbable screws were used to provide roll stabilization. The bioabsorbable screws were inserted so as not to be exposed on the cartilage surface (Fig. 2). After the fixation, a probe was used to confirm solidity.
After surgery, patients were allowed to immediately flex the knee joint without limitations and do an isometric muscle strengthening exercise. No weight bearing was allowed for 6 weeks and crutches were used to permit partial-weight bearing for 6 additional weeks. Sports activities were permitted 1 year after the surgery.
With regard to the clinical and functional evaluation, the average KOOS was 44.9 points (range, 31.5 to 51.2 points) before surgery and 88.1 points (range, 83.3 to 91.1 points) at follow-up (p = 0.03). The Lysholm knee score improved from an average of 32.6 points (range, 27 to 41 points) before surgery to an average of 82.8 points (range, 78 to 88 points) at follow-up (p = 0.03). The IKDC score improved from an average of 40.8 points (range, 31 to 47 points) before surgery to an average of 85.6 points (range, 83 to 89 points) at follow-up (p = 0.03). With regard to recovery of the level of exercise ability, the Tegner activity scale score showed an improvement from an average of 2.8 points (range, 2 to 4 points) before surgery to an average of 6.1 points (range, 5 to 7 points) at follow-up (p = 0.03) (Table 3). There were no complications such as infection, intra-articular adhesion, or screw fixation failure in any of the cases.
MRI was performed in all 11 cases at the 12-month follow-up. These MRI scans showed that the articular surface coincided in overall, with similar signal intensity compared with the peripheral normal cartilage. One radiologist did the reading using T2 Fat suppression image.
At the second arthroscopic examination, the articular surface appearance generally agreed with the MRI findings and, in all cases, the articular surface of the lesion was observed to be covering the inner fixture. On palpation using a probe, the osteochondral plate appeared to be stable, and no abnormal findings of symmetrical bone articular surface on the bioabsorbable screw insertion site were observed. Based on the arthroscopic classification evaluation by Guhl,13) there were five grade II cases and six grade III cases. Before surgery, and seven grade I cases and four grade II cases at follow-up, indicating improvement (Table 2 and Fig. 4).
The treatment of OCD varies from conservative treatment to surgical treatment depending on patient age, lesion size, lesion site, and lesion stability. OCD of the knee joint in the adolescent period before the growth plate is closed has a high healing potential, and successful cures were reported with 6 weeks of conservative therapy such as nonweight-bearing and fixation, including natural healing.14) However, Twyman et al.15) reported that 32% of patients diagnosed with OCD before bone maturation developed moderate or severe arthritis, and if inflamed OCD persists until bone maturation is complete, degenerative arthritis develops at a high frequency. Therefore, as Kocher et al.10) reported, for unstable OCD in the adolescent period in which the growth plate is not fused, satisfactory results were obtained by attempting active fixation of the lesion rather than conservative treatment.
Multiple drilling is a typical surgical treatment, and many studies reported good results after performing it.16171819) For example, in the study of Kocher et al.,18) arthroscopic multiple drilling was performed for 23 patients ranging in age from 8.5 to 16.1 years. In the mean follow-up period of 3.9 years, all patients were clinically and radiologically cured without any complications. According to Kouzelis et al.,19) 90% of patients who had undergone Herbert screw fixation had a good clinical and radiological result. Also in a study of autologous osteochondral grafting and fixation, 70% to 95% of the patients were improved clinically and radiologically.202122) Gudas et al.23) reported that clinical and radiological improvement was obtained in 92% of the patients with autologous chondrocyte implantation.
Regarding the fixture methods employed to stabilize these unstable lesions, bioabsorbable pin or screw fixation can be applied and both are reported to be effective in improving symptoms.2425) Bioabsorbable fixtures do not need to be removed in contrast to metal fixtures. Furthermore there is an advantage of having the low image interference of the bioabsorbable fixture on MRI examination.26) Larsen et al.25) reported that internal fixation was performed using 2-3 bioabsorbable screws through arthrotomy for seven patients with an average age of 25.6 year (range, 17 to 46 years). At an average follow-up of 2.6 years, six patients out of seven (85.7%) showed satisfactory results clinically and radiologically, and one showed a nonunion requiring removal of the vitreous body from the joint. No other specific complications occurred. Din et al.24) reported that an average of 3.9 (range, 2 to 6) absorbable pins per patient, depending on the size of the lesion, were used to perform arthroscopic internal fixation on 12 patients with an average age of 14.8 years (range, 12 to 16 years). At an average of 32.4 months after surgery, union was observed in all 12 cases on the follow-up MRI. One case showed transient synovitis which improved with general treatment. However, there are reports of complications such as inflammation, osteolytic lesions, synovitis, and instrument rupture after internal fixation using these bioabsorbable pins or screws,26) Millington et al.27) performed surgery on patients having an average age of 19 years (range, 14 to 39 years) using various absorbable internal fixtures such as pins and screws. Among the 18 patients that were able to be followed for an average of 59 months, six patients (33.3%) showed union failures and complications such as a vitreous body within the joint. Surgical failures are reported with the use of smooth, non-threaded fixtures, such as pins, due to insufficient pressure. However, complications reported in other studies were not observed in our study which used bioabsorbable screw fixation. In all 11 of our cases, union was observed and clinically satisfactory results were obtained. These results were obtained by using an arthroscopy and inserting bioabsorbable screws with threads vertically into the lesion to provide maximum axial pressure, and two or more bioabsorbable screws to provide rotational stabilization. We also provided a sufficient rehabilitation period. However, because the follow-up period was relatively short, long-term follow-up observations and evaluation for complications are required.
In the study of Webb et al.28) healing of the treated lesion was assessed by the surgeon's examination of radiographs at final follow-up. In that study, MRI was used in nine cases to evaluate healing and lesion stability, whereas plain radiographs were obtained in 10 patients and a computed tomography scan in a single patient. At the final postoperative follow-up, osseous integration was evident in 15 of 20 knees (75%), with the 5 unhealed lesions all located on the lateral condyle.
In the present study, when MRI findings were classified according to Dipaola et al.,12) there were four grade II cases and seven grade III cases before surgery and eight grade I cases and three grade II cases at follow-up, indicating improvement in all cases after surgery.
There are several limitations to this study. The number of cases is small, and comparative analyses of the lesion size and site were not possible. In addition, there was no control group and only a short follow-up observation period. Finally, the second arthroscopic examination and MRI were conducted during follow-up observation to decide the postsurgical condition objectively, but a second arthroscopic examination is an invasive method, and MRI has the disadvantage of high cost.
In treating unstable OCD lesions causing pain in the adolescent patient, arthroscopic bioabsorbable screw fixation is considered to be an effective treatment method for reducing pain, and shows satisfactory results in recovering exercise ability.
Figures and Tables
Fig. 2
(A) The arthroscopic image from case no.2 shows an unstable lesion of the medial femoral condyle. (B) The drill guide is inserted in the vertical position into the lesion. (C) A bioabsorbable screw is inserted with vertical compression force. (D) The arthroscopic image shows three bioabsorbable screws in the osteochondritis dissecans lesion.
Fig. 3
(A, B) The preoperative magnetic resonance imaging (T2 fat suppression) scans from case no.2 show osteochondritis dissecans of the medial femoral condyle (arrow). (C, D) The magnetic resonance imaging scans taken at follow-up, 12 months after operation, show three bioabsorbable screws (arrows) fixed with nearly normal congruency of the articular surface overlying the fixation site.
Fig. 4
(A) The preoperative arthroscopic image shows bioabsorbable screw fixation of the osteochondritis dissecans lesion. (B) The second-look arthroscopy image at 12 months postoperatively revealed that the lesion is covered with cartilage.
Table 1
Case Analysis
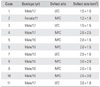
Table 2
Magnetic Resonance Imaging and Arthroscopy Stage
| Grade | Magnetic resonance imaging stage (by Dipaola et al.12)) | Arthroscopy stage (by Guhl13)) | ||
|---|---|---|---|---|
| Preoperative | Last follow-up | Preoperative | Last follow-up | |
| I | - | 8 | - | 7 |
| II | 4 | 3 | 5 | 4 |
| III | 7 | - | 6 | - |
| IV | - | - | - | - |
Table 3
Clinical Outcomes in Patients
References
1. Cahill BR. Osteochondritis dissecans of the knee: treatment of juvenile and adult forms. J Am Acad Orthop Surg. 1995; 3(4):237–247.

2. Sales de Gauzy J, Mansat C, Darodes PH, Cahuzac JP. Natural course of osteochondritis dissecans in children. J Pediatr Orthop B. 1999; 8(1):26–28.

3. Linden B. Osteochondritis dissecans of the femoral condyles: a long-term follow-up study. J Bone Joint Surg Am. 1977; 59(6):769–776.
4. Jakob RP, Franz T, Gautier E, Mainil-Varlet P. Autologous osteochondral grafting in the knee: indication, results, and reflections. Clin Orthop Relat Res. 2002; (401):170–184.

5. Prakash D, Learmonth D. Natural progression of osteo-chondral defect in the femoral condyle. Knee. 2002; 9(1):7–10.

6. Cain EL, Clancy WG. Treatment algorithm for osteochondral injuries of the knee. Clin Sports Med. 2001; 20(2):321–342.

7. Kivisto R, Pasanen L, Leppilahti J, Jalovaara P. Arthroscopic repair of osteochondritis dissecans of the femoral condyles with metal staple fixation: a report of 28 cases. Knee Surg Sports Traumatol Arthrosc. 2002; 10(5):305–309.

8. Lipscomb PR Jr, Lipscomb PR Sr, Bryan RS. Osteochondritis dissecans of the knee with loose fragments: treatment by replacement and fixation with readily removed pins. J Bone Joint Surg Am. 1978; 60(2):235–240.

9. Dervin GF, Keene GC, Chissell HR. Biodegradable rods in adult osteochondritis dissecans of the knee. Clin Orthop Relat Res. 1998; (356):213–221.

10. Kocher MS, Tucker R, Ganley TJ, Flynn JM. Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med. 2006; 34(7):1181–1191.

11. Murray JR, Chitnavis J, Dixon P, et al. Osteochondritis dissecans of the knee; long-term clinical outcome following arthroscopic debridement. Knee. 2007; 14(2):94–98.

12. Dipaola JD, Nelson DW, Colville MR. Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy. 1991; 7(1):101–104.

13. Guhl JF. Arthroscopic treatment of osteochondritis dissecans. Clin Orthop Relat Res. 1982; (167):65–74.

14. Hughston JC, Hergenroeder PT, Courtenay BG. Osteochondritis dissecans of the femoral condyles. J Bone Joint Surg Am. 1984; 66(9):1340–1348.

15. Twyman RS, Desai K, Aichroth PM. Osteochondritis dissecans of the knee: a long-term study. J Bone Joint Surg Br. 1991; 73(3):461–464.

16. Cepero S, Ullot R, Sastre S. Osteochondritis of the femoral condyles in children and adolescents: our experience over the last 28 years. J Pediatr Orthop B. 2005; 14(1):24–29.

17. Aglietti P, Buzzi R, Bassi PB, Fioriti M. Arthroscopic drilling in juvenile osteochondritis dissecans of the medial femoral condyle. Arthroscopy. 1994; 10(3):286–291.

18. Kocher MS, Micheli LJ, Yaniv M, Zurakowski D, Ames A, Adrignolo AA. Functional and radiographic outcome of juvenile osteochondritis dissecans of the knee treated with transarticular arthroscopic drilling. Am J Sports Med. 2001; 29(5):562–566.

19. Kouzelis A, Plessas S, Papadopoulos AX, Gliatis I, Lambiris E. Herbert screw fixation and reverse guided drillings, for treatment of types III and IV osteochondritis dissecans. Knee Surg Sports Traumatol Arthrosc. 2006; 14(1):70–75.

20. Fonseca F, Balaco I. Fixation with autogenous osteochondral grafts for the treatment of osteochondritis dissecans (stages III and IV). Int Orthop. 2009; 33(1):139–144.

21. Kobayashi T, Fujikawa K, Oohashi M. Surgical fixation of massive osteochondritis dissecans lesion using cylindrical osteochondral plugs. Arthroscopy. 2004; 20(9):981–986.

22. Miura K, Ishibashi Y, Tsuda E, Sato H, Toh S. Results of arthroscopic fixation of osteochondritis dissecans lesion of the knee with cylindrical autogenous osteochondral plugs. Am J Sports Med. 2007; 35(2):216–222.

23. Gudas R, Simonaityte R, Cekanauskas E, Tamosiunas R. A prospective, randomized clinical study of osteochondral autologous transplantation versus microfracture for the treatment of osteochondritis dissecans in the knee joint in children. J Pediatr Orthop. 2009; 29(7):741–748.

24. Din R, Annear P, Scaddan J. Internal fixation of undisplaced lesions of osteochondritis dissecans in the knee. J Bone Joint Surg Br. 2006; 88(7):900–904.

25. Larsen MW, Pietrzak WS, DeLee JC. Fixation of osteochondritis dissecans lesions using poly(l-lactic acid)/ poly(glycolic acid) copolymer bioabsorbable screws. Am J Sports Med. 2005; 33(1):68–76.

26. Scioscia TN, Giffin JR, Allen CR, Harner CD. Potential complication of bioabsorbable screw fixation for osteochondritis dissecans of the knee. Arthroscopy. 2001; 17(2):E7.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download