Abstract
Background
The delta reverse shoulder replacement system was developed for the treatment of rotator cuff arthropathy so that the deltoid can substitute for the deficient rotator cuff. To evaluate the results of delta reverse shoulder replacement for functional improvement and complications in a consecutive series by a single surgeon over a period of six years with a minimum follow-up of 2 years.
Methods
The data were collected retrospectively from electronic theatre records. Over a period of 6 years (2006-2012), 46 cases that fulfilled the inclusion criteria were identified. There were 34 females and 12 males. The average age of patients was 76.2 years (range, 58 to 87 years). A single surgeon performed all procedures using the anterosuperior approach. The mean follow-up time was 49 months (range, 24 to 91 months). All cases had preoperative and postoperative Constant scores. We collected the data on indications, hospital stay, and change in the Constant score, complications, and reoperation rates.
Results
The main indication for surgery was rotator cuff arthropathy (52.2%), followed by massive rotator cuff tear (28.3%), osteoarthritis (8.7%), fractures (6.5%), and rheumatoid arthritis (4.3%). Also, 65.2% of the cases were referred by general practitioners, 26% of the cases were referred by other consultants, and 8.8% of the cases were already under the care of a shoulder surgeon. The average preoperative Constant score was 23.5 (range, 8 to 59). The average Constant score at the final follow-up was 56 (range, 22 to 83). On average, there was an improvement of 33 points in the Constant score. The improvement in the Constant score was significant (p < 0.001). We observed complications in four patients (8.6%). Three of four patients (6.5%) needed reoperation. The first complication was pulmonary embolism in the early postoperative period. The other complications included dissociation of the glenosphere from the metaglene, deltoid detachment, and stitch abscess.
Massive rotator cuff tear is one of the challenging clinical conditions.1) Especially with a secondary degenerative process and proximal migration of the humeral head, the movements of the shoulder joint become severely restricted. This end stage arthritis is referred to as pseudoparalysis or rotator cuff arthropathy.23)
The treatment options in these cases are limited, and the aim of treatment is mainly to improve the pain. However, improvement in pain often results in functional improvement. Conservative management as well as arthroscopic debridement and biceps tenotomy can be attempted.45) These less aggressive measures are not as effective as joint replacement and patients should be briefed about the realistic outcomes. The major issues associated with total shoulder replacement in a rotator cuff-deficient shoulder are accelerated glenoid component loosening as well as limited joint movement.6)
The delta reverse shoulder replacement system was developed by Grammont and Baulot7) for the treatment of rotator cuff arthropathy. In these patients, due to an irreparable rotator cuff, arm elevation is not possible. The delta reverse shoulder system is designed to medialise the centre of rotation and also to advance the deltoid insertion at a more distal point.89) This increases the pretension in the deltoid muscle and enables this muscle to elevate the arm.10) Therefore, the rotator cuff function is substituted by the deltoid muscle.
The most common indication for reverse polarity shoulder replacement is rotator cuff arthropathy.1112) Recently, the indications have expanded to include fractures, salvage revision arthroplasty, osteoarthritis, and rheumatoid arthritis.13141516) The complication rate has been reported to range from 16% to 52% depending on the primary indication, and the most commonly reported complications are dislocation, nerve damage, loosening, and periprosthetic fractures.2101217) The reoperation rate has been reported to range from 8% to 18%.2101217)
We evaluated the clinical results of delta reverse shoulder replacement in a consecutive series by a single surgeon over a period of 6 years with a minimum follow-up of 2 years. The aim of study was to assess for the improvement in shoulder function and note any complications of the surgery.
The data were collected retrospectively. We identified our sample from electronic theatre records. All patients who had undergone delta reverse shoulder replacement were initially selected. We included only those patients who had a minimum two-year follow-up with the record of preoperative and postoperative constant scores. None of these patients had a history of previous arthroplasty although two patients had a history of previous rotator cuff repairs. The indications for reverse shoulder arthroplasty in our series were rotator cuff arthropathy, massive rotator cuff tear, osteoarthritis, failure of previous cuff repair, and rheumatoid arthritis.
The reverse shoulder arthroplasty procedures were performed between 2006 and 2012 by a single surgeon using the anterosuperior (Mackenzie) approach. Forty-six cases fulfilled our inclusion criteria. The inclusion criteria included; single surgeon, single approach, primary arthroplasty, a minimum 2-year follow-up, and the record of Constant scores. The mean follow-up time was 49 months (range, 24 to 91 months). All cases had pre- and postoperative Constant scores and then the subsequent Constant score at each follow-up appointment. We recorded the source of primary referral, indication for surgery, duration of hospital stay, and reasons for prolonged stay (> 6 days).
We collected the data on any complications from the time of surgery to discharge from follow-up. The rate and indication for revision surgery were also recorded. We used IBM SPSS ver. 22 (IBM Co., Armonk, NY, USA) to analyse the data and to calculate the p-value for change in the Constant score. The p-value was calculated using Wilcoxon signed-rank test and a value of less than 0.05 was assumed to be significant.
The demographic data are shown in Table 1. There were 34 females and 12 males. The average age of patients was 76.2 years (range, 58 to 87 years). The proportion of various indications is presented in Fig. 1. The main indication for surgery was rotator cuff arthropathy (52.2%), followed by massive rotator cuff tear (28.3%), osteoarthritis (8.7%), fractures (6.5%), and rheumatoid arthritis (4.3%). Also, 65.2% of the cases were referred by general practitioners, 26% of the cases were referred by other consultants, and 8.8% of the cases were already under the care of a shoulder surgeon. The average duration of hospital stay was 3 days (range, 2 to 7 days). The average preoperative Constant score was 23.5 (range, 8 to 59). The average Constant score at the final follow-up was 56 (range, 22 to 83). On average, there was an improvement of 33 points in the Constant score (Fig. 2). We used the Wilcoxon signed-rank test to assess the change in the Constant score. The improvement in the Constant score was significant (p < 0.001).
We observed complications in 4 patients (8.6%). Table 2 shows the nature and timing of complications. The first complication was pulmonary embolism in the early postoperative period. This patient was treated with warfarin. The second patient experienced pain and sound in his shoulder 6 months after the surgery. His radiographs raised the suspicion of dissociation between the glenosphere and the metaglene. Examination under anaesthesia using image intensifier confirmed the dissociation of the glenosphere from the metaglene (Fig. 3). This patient required revision surgery. Intraoperatively, it was noted that the screw on the medial surface of the glenosphere was broken. The movement of the glenosphere had caused damage of the polyethylene (Fig. 4). The metaglene, the glenosphere, and the polyethylene were revised. The next complication was a stitch abscess, which was observed at 5 weeks after surgery. The abscess was drained. However, 5 months after the initial surgery, the patient developed a sinus at the site of the stitch abscess. The sinus covered with the granulation tissue was excised. The patient did not require any further procedures. The final complication was detachment of the deltoid muscle. This patient had undergone previous open subacromial decompression and rotator cuff repair at another hospital. His preoperative X-rays showed fracture of the acromion. During arthroplasty, it was noted that he had fibrous non-union of the acromion, but the deltoid muscle was in good shape. Therefore, the acromion fracture was left alone and arthroplasty was performed. Postoperatively, he experienced pain and X-rays showed that the fracture fragment was pulled by the deltoid (Fig. 5). This patient required surgery for re-attaching the deltoid muscle. In total, we had three patients who needed reoperation for any reason. Among these patients, only one patient had prosthesis failure.
Arthroplasty in patients with a deficient rotator cuff has evolved over 40 years. The earlier authors noted the inability of prime movers to act properly after arthroplasty in the presence of a deficient rotator cuff.1819) Therefore, the outcome of arthroplasty in these patients was not satisfactory.320) Neer introduced the concept of constrained designs for patients with a deficient rotator cuff.820) However, Neer's three versions of constrained designs had higher complications in the form of dislocation, glenoid component loosening, and decreased excursion.21) This was probably due to increased stresses at bone-implant interface. Fenlin22) believed that by enlarging the glenohumeral construct, the range of motion could be improved. This would also increase the lever arm of the deltoid, enabling this muscle to elevate the arm.22) The long-term results showed higher rates of anterior instability, implant breakage, and loosening.23) Therefore, it was concluded that the failure was not primarily due to the prosthesis design.24) In fact, the failure was due to inability to avoid the subluxation effect of the deltoid because of a deficient rotator cuff.24) In the absence of rotator cuff, the stability and abduction could only be improved by utilizing the deltoid muscle.
Grammont et al.9) and Kalouche et al.25) proposed the idea of increasing the deltoid lever arm for arm elevation, and hence substituting for a deficient rotator cuff. The suggestion was to medialise the centre of rotation in order to increase the lever arm of the deltoid. In addition to this, to increase the tension in the middle part of the deltoid (responsible for abduction), the centre of rotation needs to be lowered from its anatomic position.925) For the patients with rotator cuff deficiency, Grammont proposed that the anatomic prostheses would not be functionally successful.24) In 1985, Grammont designed the reverse polarity shoulder replacement. The center of rotation for this system is medial and distal compared to the anatomical center of rotation. The weight-bearing component (glenoid) is convex, and the supporting component (humeral) is concave.9) Since then, there have been a few modifications to the current delta reverse shoulder replacement system, but the basic design concepts are the same.6)
The reverse polarity shoulder replacement gained popularity initially among patients with rotator cuff arthropathy. However, it is now being used for a variety of other indication including fractures, inflammatory arthropathy, and massive rotator cuff tears.26272829) With increase in in indications the complication and revision rate has also increased. The reported revision surgery rate is between 8% and 18%.2101217) The risks of complication and reoperation are higher in patients who need reverse polarity prosthesis as a result of failed previous arthroplasty.141517) The higher rate of complications in revision cases may be due to limited bone stock and poor soft tissue quality.
Werner et al.17) reported a complication rate of 50% and a revision rate of 33% at an average follow-up of 38 months. They reported a higher complication rate (51%) and reoperation (39%) rate in revision surgery. For primary procedures, the reported complication rate was 47% and the reported reoperation rate was 18%.17)
Grassi et al.2) reported the results of Delta III reverse shoulder prosthesis used in 23 patients for a variety of indications. The reported complication rate was 17.3% and the reported revision rate was 8.6% at a mean follow-up of 42 months.2) Naveed et al.10) reported the results of 50 patients who had undergone Delta III reverse shoulder replacement for rotator cuff arthropathy. At a mean followup of 39 months, the reported complication rate was 14% and the reported reoperation rate was 8%.
In our series, we observed complications in 4 patients (8.6%) and 3 of these patients (6.5%) needed reoperation (Table 3). Disengagement of the glenosphere from the metaglene was the only complication due to the failure of prosthesis and the patient needed revision of the glenoid component and polyethylene. This complication has been reported in the literature. The cause of disengagement has been considered to be inadequate reaming around the edge of the metaglene or soft tissue or bone interposition between the metaglene and glenosphere.30) We used the anterosuperior (Mackenzie) approach in all the patients. This approach has a potentially higher risk of axillary nerve injury but provides better glenoid exposure.17) The deltopectoral approach has been reported to be associated with a high dislocation rate due to subscapularis detachment, but it preserves the deltoid muscle. Based on the experience of the senior author, the anterosuperior approach allows for inferior placement of the metaglene, which is desirable to prevent glenoid notching.
The study shows short-term results of delta reverse shoulder arthroplasty. At this stage, the results are encouraging with no cases of loosening, deep infection, or dislocation. The complication and reoperation rates are better compared to those in previous studies. However, a long-term follow-up is required in order to comment on loosening and revision surgery.
Figures and Tables
Fig. 3
Disengagement of glenosphere. Radiograph (A) and fluoroscopic image (B) of the left shoulder obtained during manipulation under anesthesia. The arrows show dissociated glenosphere from the metaglene.

Fig. 4
Intraoperative photographs showing a broken screw (arrow) on the posterior part of the glenosphere (A) and damaged polyethylene (arrow) (B).

Table 1
Demographic Data
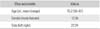
| Characteristic | Value |
|---|---|
| Age (yr), mean (range) | 76.2 (58-87) |
| Gender (male:female) | 12:34 |
| Side (left:right) | 22:24 |
Table 2
Complications
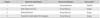
Table 3
Previous Studies Presenting Complications and Reoperation Rates
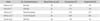
| Study | No. of joints/indication | Mean follow-up (mo) | Complication (%) | Reoperation (%) |
|---|---|---|---|---|
| Naveed et al.10) | 50/mixed | 39 | 14.0 | 8.0 |
| Grassi et al.2) | 23/mixed | 42 | 17.3 | 8.6 |
| Valenti et al.12) | 76/cuff arthropathy | 44 | 18.4 | 13.0 |
| Werner et al.17) | 17/cuff arthropathy | 38 | 50.0 | 33.0 |
| Present study | 46/mixed | 49 | 8.6 | 6.5 |
References
1. Vanhove B, Beugnies A. Grammont's reverse shoulder prosthesis for rotator cuff arthropathy: a retrospective study of 32 cases. Acta Orthop Belg. 2004; 70(3):219–225.
2. Grassi FA, Murena L, Valli F, Alberio R. Six-year experience with the Delta III reverse shoulder prosthesis. J Orthop Surg (Hong Kong). 2009; 17(2):151–156.

3. Neer CS 2nd, Craig EV, Fukuda H. Cuff-tear arthropathy. J Bone Joint Surg Am. 1983; 65(9):1232–1244.

4. Burkhart SS. Arthroscopic treatment of massive rotator cuff tears: clinical results and biomechanical rationale. Clin Orthop Relat Res. 1991; (267):45–56.
5. Walch G, Madonia G, Pozzi I, Riand N, Levigne C. Arthroscopic tenotomy of the long head of the biceps in rotator cuff ruptures. In : Gazielly DF, Gleyze P, Thomas T, editors. The cuff. Paris: Elsevier;1996. p. 350–355.
6. Pollock RG, Deliz ED, McIlveen SJ, Flatow EL, Bigliani LU. Prosthetic replacement in rotator cuff-deficient shoulders. J Shoulder Elbow Surg. 1992; 1(4):173–186.

7. Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993; 16(1):65–68.

8. Flatow EL, Harrison AK. A history of reverse total shoulder arthroplasty. Clin Orthop Relat Res. 2011; 469(9):2432–2439.

9. Grammont P, Trouilloud P, Laffay JP, Deries X. Concept study and realization of a new total shoulder prosthesis. Rhumatologie. 1987; 39:407–418.
10. Naveed MA, Kitson J, Bunker TD. The Delta III reverse shoulder replacement for cuff tear arthropathy: a single-centre study of 50 consecutive procedures. J Bone Joint Surg Br. 2011; 93(1):57–61.
11. Bohsali KI, Wirth MA, Rockwood CA Jr. Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006; 88(10):2279–2292.

12. Valenti P, Sauzieres P, Katz D, Kalouche I, Kilinc AS. Do less medialized reverse shoulder prostheses increase motion and reduce notching? Clin Orthop Relat Res. 2011; 469(9):2550–2557.

13. Cazeneuve JF, Cristofari DJ. Delta III reverse shoulder arthroplasty: radiological outcome for acute complex fractures of the proximal humerus in elderly patients. Orthop Traumatol Surg Res. 2009; 95(5):325–329.

14. Flury MP, Frey P, Goldhahn J, Schwyzer HK, Simmen BR. Reverse shoulder arthroplasty as a salvage procedure for failed conventional shoulder replacement due to cuff failure: midterm results. Int Orthop. 2011; 35(1):53–60.

15. Wall B, Nove-Josserand L, O'Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007; 89(7):1476–1485.
16. Zafra M, Uceda P, Flores M, Carpintero P. Reverse total shoulder replacement for nonunion of a fracture of the proximal humerus. Bone Joint J. 2014; 96(9):1239–1243.

17. Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005; 87(7):1476–1486.

18. Neer CS 2nd. Replacement arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 1974; 56(1):1–13.

19. Reeves B, Jobbins B, Flowers F, Dowson D, Wright V. Some problems in the development of a total shoulder endoprosthesis. Ann Rheum Dis. 1972; 31(5):425–426.

20. Neer CS 2nd, Watson KC, Stanton FJ. Recent experience in total shoulder replacement. J Bone Joint Surg Am. 1982; 64(3):319–337.

21. Katz D, O'Toole G, Cogswell L, Sauzieres P, Valenti P. A history of the reverse shoulder prosthesis. Int J Shoulder Surg. 2007; 1(4):108–113.

23. Fenlin JM. Semi-constrained prosthesis for the rotator cuff deficient patient. Orthop Trans. 1985; 9:55.
24. Baulot E, Sirveaux F, Boileau P. Grammont's idea: the story of Paul Grammont's functional surgery concept and the development of the reverse principle. Clin Orthop Relat Res. 2011; 469(9):2425–2431.

25. Kalouche I, Sevivas N, Wahegaonker A, Sauzieres P, Katz D, Valenti P. Reverse shoulder arthroplasty: does reduced medialisation improve radiological and clinical results? Acta Orthop Belg. 2009; 75(2):158–166.
26. Bufquin T, Hersan A, Hubert L, Massin P. Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg Br. 2007; 89(4):516–520.
27. Cuff DJ, Pupello DR. Comparison of hemiarthroplasty and reverse shoulder arthroplasty for the treatment of proximal humeral fractures in elderly patients. J Bone Joint Surg Am. 2013; 95(22):2050–2055.

28. Holcomb JO, Hebert DJ, Mighell MA, et al. Reverse shoulder arthroplasty in patients with rheumatoid arthritis. J Shoulder Elbow Surg. 2010; 19(7):1076–1084.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download