Abstract
Distribution of A118G single nucleotide polymorphism (SNP) in the mu-opioid receptor 1 gene (OPRM1) differs with ethnicity. We assessed the distribution of this SNP in Korean women with breast cancer and compared it with that in women of other ethnicities with breast cancer. Distribution of SNP genotypes was as follows: 49.8% for AG genotype, 40.6% for AA genotype, and 9.6% for GG genotype. Logistic regression analysis showed a negative association between the presence of the G allele at position 118 of OPRM1 and breast cancer in the studied population (odds ratios [OR], 0.635; p=0.002). However, the AG and GG genotypes were not associated with breast cancer in the studied population (OR, 0.719; p=0.130). The proportions of the AG and GG genotypes of the OPRM1 SNP were higher in Korean women with breast cancer than in those of other ethnicities.
Opioid receptors are involved in tumor growth and progression [123]. Active research is being performing on single nucleotide polymorphisms (SNPs) because genetic variation is associated with the occurrence and progression of different diseases. Recently, Cieślińska et al. [4] reported that presence of G allele in mu-opioid receptor 1 gene (OPRM1) A118G SNP increased the incidence of breast cancer in Caucasian women in northeastern Poland, of which 18% and 3% women had AG and GG genotypes, respectively, of the A118G SNP. Distribution of the OPRM1 A118G SNP differs according to ethnicity [45678]. Therefore, studies involving individuals of other ethnicities should be performed to confirm this. The present study was conducted to confirm the effects of the differential distribution of the OPRM1 A118G SNP on breast cancer in Korean women.
Study protocol was reviewed and approved by the Institutional Review Board of Konkuk University Medical Center, Seoul, South Korea (KUH1160085), and the study was registered at https://cris.nih.go.kr (KCT0001558). Medical records of Korean women who underwent breast surgery under general anesthesia at Konkuk University Medical Center from June 2012 to June 2014 were reviewed retrospectively. All the women were examined before the breast surgery to confirm that cancers primarily originated from the breast. None of the women received exogenous opioids. The women were classified into benign and cancer groups based on their pathological findings, which were confirmed by pathologists. Data on the genotyping of the OPRM1 A118G SNP were obtained from our previous study [5]. A118G SNP genotypes were determined by performing polymerase chain reaction (PCR)–restriction fragment length polymorphism. The PCR was performed using primers (5'-GGTCAACTTGTCCCACTTAGATCGC-3' and 5' AATCACATACATGACCAGGAAGTTT-3') specific to the A118G SNP (193 bp). The A118G SNP was analyzed using its restriction patterns, that is, SNP with a homozygous AA genotype provided a 193-bp fragment; SNP with a heterozygous AG genotype provided 193-, 169-, and 24-bp fragments; and SNP with a homozygous GG genotype provided 169- and 24-bp fragments. Results for each genotype were confirmed in randomly selected women by performing direct sequencing. In addition, our data were compared with those obtained for Caucasian women from northeastern Poland [4] and for European-American and African-American women [8]. Independent two-tailed t-test was used to compare the means of variables in continuous, normally distributed data, and chi-square test was used to compare genotypes between women in the benign and cancer groups. Allele frequencies were calculated from the results of two previous studies [48] by using the chi-square test. The risk of breast cancer was estimated using two methods, namely, (1) G allele versus A allele and (2) AG and GG genotypes versus AA genotype. Odds ratios (ORs) and 95% confidence intervals were calculated using logistic regression analysis. Normally distributed continuous data are presented as means±standard deviations, and the number of patients (n) and proportion (%) were calculated for categorical variables. All calculations were performed using SPSS version 18.0 (SPSS Inc., Chicago, USA), and p<0.05 was considered statistically significant.
In all, 444 women underwent breast surgery under general anesthesia at Konkuk Universtiy Medical Center. Data of three women with a history of cancer other than breast cancer, one woman with a history of previous radiotherapy to the upper body or chemotherapy, three women with recurrence after a previous breast surgery, and one woman with metastatic breast cancer from another organ were excluded. In addition, data of 28 women were excluded because of incomplete information on the OPRM1 A118G SNP. Thus, data of 408 women met the inclusion criteria and were analyzed in the present study. Of these 408 women, 157 were included in the benign group and 251 were included in the cancer group. The proportions of SNPs in the benign and cancer groups were AG>AA>GG. Distribution of the SNP genotypes in women in the cancer group was as follows: 49.8% for the AG genotype, 40.6% for the AA genotype, and 9.6% for the GG genotype (Figure 1). The proportions of the AG and GG genotypes the OPRM1 A118G SNP were higher in women included in the present study than in those of other ethnicities. Moreover, the percentage of the G allele was higher in women included in the present study than in those of other ethnicities. Stratification of the distribution of the OPRM1 A118G SNP according to cancer stage did not show significant inter-group differences (p=0.273) (Table 1). Logistic regression analysis showed a negative association between the presence of the G allele at position 118 of OPRM1 and breast cancer in women included in the present study (OR, 0.635; p=0.002). However, the AG and GG genotypes of the OPRM1 A118G SNP were not associated with breast cancer (OR, 0.719; p=0.130). Regression analysis of the results obtained by Cieślińska et al. [4] showed a strong association between the G allele of the OPRM1 A118G SNP and breast cancer in Caucasian women, which was consistent with that observed in their study (Table 2).
Distribution of the OPRM1 A118G SNP in Korean women with breast cancer was different from that in those of other ethnicities such as Caucasian, European-American, and African-American women with breast cancer. Particularly, the proportions of the AG and GG genotypes of the OPRM1 A118G SNP were relatively higher in women included in the present study than in those of other ethnicities. However, the AG and GG genotypes of the OPRM1 A118G SNP were not associated with breast cancer in women included in the present study. American women with breast cancer having one or more copies of the G allele show a low risk of mortality [8]. The study by Cieślińska et al. [4] is the only study to report a relationship between the OPRM1 A118G SNP and cancer progression. Moreover, this study showed a positive association between the AG and GG genotypes of the OPRM1 A118G SNP and breast cancer. However, this was not observed in the present study. These differences may be because of the following reasons. Initiation and progression of diseases are multifactorial, and genetic epidemiology alone does not completely account for the incidence of these diseases. Various genetic factors associated with cancer progression differ according to ethnicity [910]. The pattern of the G allele according to breast cancer stage also differed in a previous study. Bortsov et al. [8] showed that the frequency of the G allele decreased with an increase in the stage of breast cancer, which is not observed in the present study. In the present study, the frequency of the G allele did not change with an increase in the stage of breast cancer. These differences may also be attributed to differences in ethnicities or other effects. Although genetic epidemiology affects cancer progression, other factors such as environmental factors may exert higher effects on breast cancer progression in the Korean population. This should be clarified by performing further studies on the relationship between the G allele and breast cancer in the Korean population.
Our study has one consideration. Women with benign breast diseases were included in the control group in the present study. However, some benign breast diseases such as atypical ductal hyperplasia are associated with breast cancer [11]. However, less number of women with these pathological conditions were included in the present study (only 12 women, 7.6% of all women in the benign group), suggesting that these conditions did not exert a significant effect on the results of the present study.
In conclusion, distribution of the OPRM1 A118G SNP in Korean women with breast cancer examined in the present study differed from that in women of other ethnicities with breast cancer. The AG and GG genotypes of the OPRM1 A118G SNP were not associated with breast cancer. Thus, our results question the status of the G allele as a valid predictor of breast cancer. However, cancer survival may differ according to ethnicity. In addition, endogenous or exogenous opioids, which act through OPRM1, may exert different effects on breast cancer outcomes. Therefore, further studies involving larger populations from different ethnic backgrounds should be performed to determine any definite relationship between the OPRM1 A118G SNP and breast cancer.
Figures and Tables
Figure 1
Distributions of mu-opioid receptor 1 gene A118G single nucleotide polymorphism in benign and cancer groups. The proportions of single nucleotide polymorphisms (SNPs) in the benign and cancer groups were AG>AA>GG, and the distribution of the SNP was 49.8% AG, 40.6% AA, and 9.6% GG in the cancer group.
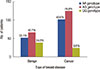
Table 1
Distribution and allele frequency of mu-opioid receptor 1 gene A118G single-nucleotide polymorphisms according to ethnicity in patients with breast cancer

| OPRM1 A118G genotype | p-value | Allele frequency | |||
|---|---|---|---|---|---|
| AA, No. (%) | AG+GG, No. (%) | A | G | ||
| Ethnicity | |||||
| Korean (n = 251) | 102 (40.6) | 149 (59.4) | 0.55 | 0.45 | |
| Caucasian (n = 151) [4] | 99 (65.6) | 52 (34.4) | 0.80 | 0.20 | |
| European-American (n = 1,263) [8] | 954 (75.5) | 309 (24.5) | 0.87 | 0.13 | |
| African-American (n = 764) [8] | 728 (95.3) | 36 (4.7) | 0.98 | 0.02 | |
| Cancer stage in Korean ethnicity | 0.273 | ||||
| Carcinoma in situ (n = 52) | 20 (38.5) | 32 (61.5) | 0.64 | 0.36 | |
| Stage I (n = 113) | 53 (46.9) | 60 (53.1) | 0.69 | 0.31 | |
| Stage II (n = 68) | 22 (32.4) | 46 (67.6) | 0.61 | 0.39 | |
| Stages III, IV (n = 18) | 7 (38.9) | 11 (61.1) | 0.64 | 0.36 | |
Table 2
Association between breast cancer and the G allele at position 118 of the mu-opioid receptor 1 gene

| OR | 95% CI | p-value | |
|---|---|---|---|
| Korean | |||
| G allele (vs. A allele) | 0.635 | 0.477–0.847 | 0.002 |
| AG+GG (vs. AA | 0.719 | 0.469–1.102 | 0.130 |
| Caucasian [4] | |||
| G allele (vs. A allele)* | 2.796 | 1.854–4.217 | <0.001 |
| AG+GG (vs. AA) | 3.3 | 2.2–5.0 | <0.001 |
Notes
References
1. Afsharimani B, Cabot P, Parat MO. Morphine and tumor growth and metastasis. Cancer Metastasis Rev. 2011; 30:225–238.

2. Gach K, Wyrębska A, Fichna J, Janecka A. The role of morphine in regulation of cancer cell growth. Naunyn Schmiedebergs Arch Pharmacol. 2011; 384:221–230.

3. Mathew B, Lennon FE, Siegler J, Mirzapoiazova T, Mambetsariev N, Sammani S, et al. The novel role of the mu opioid receptor in lung cancer progression: a laboratory investigation. Anesth Analg. 2011; 112:558–567.
4. Cieślińska A, Sienkiewicz-Szłapka E, Kostyra E, Fiedorowicz E, Snarska J, Wroński K, et al. Mu opioid receptor gene (OPRM1) polymorphism in patients with breast cancer. Tumour Biol. 2015; 36:4655–4660.
5. Lee SH, Kim JD, Park SA, Oh CS, Kim SH. Effects of micro-opioid receptor gene polymorphism on postoperative nausea and vomiting in patients undergoing general anesthesia with remifentanil: double blinded randomized trial. J Korean Med Sci. 2015; 30:651–657.

6. Zhang W, Yuan JJ, Kan QC, Zhang LR, Chang YZ, Wang ZY. Study of the OPRM1A118G genetic polymorphism associated with postoperative nausea and vomiting induced by fentanyl intravenous analgesia. Minerva Anestesiol. 2011; 77:33–39.
7. Sia AT, Lim Y, Lim EC, Goh RW, Law HY, Landau R, et al. A118G single nucleotide polymorphism of human mu-opioid receptor gene influences pain perception and patient-controlled intravenous morphine consumption after intrathecal morphine for postcesarean analgesia. Anesthesiology. 2008; 109:520–526.

8. Bortsov AV, Millikan RC, Belfer I, Boortz-Marx RL, Arora H, McLean SA. Mu-opioid receptor gene A118G polymorphism predicts survival in patients with breast cancer. Anesthesiology. 2012; 116:896–902.

9. Wang Q, Gu D, Wang M, Zhang Z, Tang J, Chen J. The E-cadherin (CDH1) -160C>A polymorphism associated with gastric cancer among Asians but not Europeans. DNA Cell Biol. 2011; 30:395–400.

10. He BS, Pan YQ, Zhang Y, Xu YQ, Wang SK. Effect of LEPR Gln223Arg polymorphism on breast cancer risk in different ethnic populations: a meta-analysis. Mol Biol Rep. 2012; 39:3117–3122.

11. Marshall LM, Hunter DJ, Connolly JL, Schnitt SJ, Byrne C, London SJ, et al. Risk of breast cancer associated with atypical hyperplasia of lobular and ductal types. Cancer Epidemiol Biomarkers Prev. 1997; 6:297–301.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download