Abstract
Background
Thoracoscopic pleural biopsy is often required for rapid and confirmative diagnosis in patients with suspected pleural tuberculosis (PL-TB). However, this method is more invasive and costly than its alternatives. Therefore, we evaluated the clinical utility of the chest computed tomography (CT)-based bronchial aspirate (BA) TB-polymerase chain reaction (PCR) test in such patients.
Methods
Bronchoscopic evaluation was performed in 54 patients with presumptive PL-TB through diagnostic thoracentesis but without a positive result of sputum acid-fast bacilli (AFB) smear, pleural fluid AFB smear, or pleural fluid TB-PCR test. Diagnostic yields of BA were evaluated according to the characteristics of parenchymal lesions on chest CT.
Results
Chest radiograph and CT revealed parenchymal lesions in 25 (46%) and 40 (74%) of 54 patients, respectively. In cases with an absence of parenchymal lesions on chest CT, the bronchoscopic approach had no diagnostic benefit. BA TB-PCR test was positive in 21 out of 22 (95%) patients with early-positive results. Among BA results from 20 (37%) patients with patchy consolidative CT findings, eight (40%) were AFB smear-positive, 18 (90%) were TB-PCR-positive, and 19 (95%) were culture-positive.
Pleural tuberculosis (PL-TB) is a common manifestation of extrapulmonary tuberculosis (TB) and a treatable cause of a lymphocytic pleural effusion1. Rapid diagnosis and prompt anti-TB treatment is necessary to reverse morbidity due to TB. However, confirmative diagnosis of PL-TB is a challenge due to the low sensitivity of acid-fast bacilli (AFB) smear, TB-polymerase chain reaction (PCR) test, and culture of pleural fluid1,2.
In resource-poor settings with a high incidence of TB, one can make a presumptive diagnosis of PL-TB and initiate anti-TB treatment if the pleural fluid reveals lymphocyte-predominant exudates and adenosine deaminase (ADA) levels of ≥40 U/L3,4. However, in regions with either a low burden of TB or high levels of drug resistance, blinded or thoracoscopic pleural biopsy is often required for rapid and confirmative diagnosis accompanied by subsequent drug-sensitivity determination4,5. In most large hospitals, thoracoscopic pleural biopsy has currently replaced blinded pleural biopsy due to the excellent diagnostic yields of this method6. However, the thoracoscopic approach is the most invasive and expensive diagnostic method available for PL-TB.
It has been recommended that sputum should be included as an additional sample for laboratory investigation in cases of suspected PL-TB3,4,7. Conde et al.8 demonstrated that induced sputum exhibited a 54% culture-positive rate in patients with PL-TB who do not have parenchymal pulmonary lesions on chest radiograph. In addition, chest computed tomography (CT) has revealed that 86% of patients with PL-TB have parenchymal pulmonary lesions9. Thus, a diagnostic approach that takes these associated parenchymal lesions into account may be useful for the rapid and confirmative diagnosis of PL-TB.
Meanwhile, other recent studies have demonstrated that the bronchial aspirate (BA) TB-PCR test is useful for the rapid diagnosis of smear-negative pulmonary TB10-12. By contrast, bronchoscopic evaluation has rarely been explored in patients with suspected PL-TB, primarily because bronchoscopy has played a limited role in the investigation of patients with undiagnosed pleural effusion13-15. However, these studies were all performed in patients with undiagnosed pleural effusion rather than in selected cases of suspected PL-TB; moreover, the studies were conducted in the era before the application of chest CT and TB-PCR tests. Given the modern state of the art, it would be desirable to take advantage of current knowledge regarding the high rate of associated pulmonary lesions on chest CT in patients with PL-TB and combine this with the rapid diagnostic accuracy of the BA TB-PCR test in smear-negative pulmonary TB. From that perspective, CT-based BA TB-PCR represents a promising potential modality for rapid confirmative diagnosis in patients with suspected PL-TB. Therefore, we evaluated the clinical utility of CT-based BA TB-PCR test in patients with suspected PL-TB.
We prospectively enrolled patients for this study between January, 2010 to May, 2012. To qualify for enrollment of broncoscopic evaluation, patients had to present with pleural effusion on chest radiography and be suspected of having PL-TB based on both lymphocyte-predominant (lymphocyte>50% of total white blood cell count) exudates and ADA levels≥40 U/L by pleural fluid analyses. Chest CT scans were performed in all subjects of whom the initial chest radiography had abnormal findings suspected of pleural effusion. Diagnostic thoracentesis was performed after chest CT scans were obtained. The pleural effusion was considered an exudates if the fluid met the criteria described by Light et al.16. In addition to cell counts and ADA levels, we also performed AFB smear, mycobacterial culture, TB-PCR test, Gram staining, bacterial culture, and cytologic examination on pleural fluid specimens. Next, at least two sputum samples from each patient with sputum available were collected in the morning and used for AFB smear and mycobacterial culture. Bronchoscopy was performed in patients who did not exhibit AFB smear-positive or TB-PCR-positive results from pleural fluid, or AFB smear-positive sputum. BA was also subjected to AFB smear, TB-PCR test, mycobacterial culture, and cytologic examination. Finally, thoracoscopic pleural biopsy and pathologic examination were performed for some patients who did not exhibit positive AFB smear or TB-PCR results from BA. The size of pleural effusion was estimated from the initial chest radiograph. An effusion was considered small if it occupied up to a third of the affected hemithorax; moderate if it occupied up to half of the hemithorax; and large when it affected more than half of the hemithorax8. PL-TB was diagnosed as follows: 1) positive culture for Mycobacterium tuberculosis (MTB) in pleural fluid, sputum, or BA; 2) pathologically chronic granulomatous inflammation in pleural biopsy tissue; and 3) clinical improvement upon anti-TB medication without other possible causes of pleural effusion, on the basis of lymphocyte-predominant exudates and ADA levels ≥40 U/L.
The diagnostic yields of BA were evaluated according to the assessment and characteristics of pulmonary parenchymal lesions on chest radiography and CT. Informed consent was obtained from each patient. The study protocols were reviewed and approved by our institutional review board.
The initial chest radiograph and CT prior to diagnostic thoracentesis were reviewed blindly by a board-certified radiologist and a pulmonologist, who evaluated the presence of the parenchymal pulmonary lesions. If any findings on chest CT were present, they were classified as patchy consolidative, nodular (<20 mm in size), linear-fibrotic, mass-like (≥20 mm in size), cavitary, or calcified9. In addition, the involvement of lung lesions on chest CT was categorized as either equal or less than one segment ('≤segmental') or more than one segment ('>segmental'). After reviewing the chest radiograph and CT findings, final decisions were reached by consensus.
After examination of tracheobronchial structure, normal saline was instilled into the orifices of the bronchopulmonary segments at which the lesion was likely to be located, and was then aspirated back. This bronchial procedure was repeated several times to get at least 12 mL of BA for cytology and microbial examination, including AFB staining, mycobacterial culture, and TB-PCR. For microscopic examination, the AFB smears were stained with auramine-fluorochrome and examined under a fluorescence microscope. MTB culture was performed by incubating the specimens in 3% Ogawa solid medium (Shin-yang Chemical, Seoul, Korea) and liquid medium (BACTEC MGIT 960 liquid medium; BD Biosciences, Sparks, MD, USA) for 8 and 6 weeks, respectively. Nucleic acid probes (Gen-Probe, San Diego, CA, USA) were used to identify MTB from samples that exhibited mycobacterial growth.
For real-time PCR testing of BA and pleural fluid, we used the Real-Q MTB & NTM PCR kit (Biosewoom Inc., Seoul, Korea) and the ABI 7500 Real-time PCR system (Applied Biosystems, Foster City, CA, USA), in accordance with the manufacturers' instructions.
Data are presented as number followed by percentage (number [%]) of patients with a positive result, unless otherwise specified. Statistical comparisons of diagnostic yields according to the presence or absence of pulmonary parenchymal lesions on chest radiography and CT were performed by χ2-test or Fisher's exact test. All tests of significance were two-sided, and a p<0.05 was considered statistically significant. Statistical analyses were performed using the PASW version 18.0 (SPSS Inc., Chicago, IL, USA).
We initially enrolled a total of 73 patients whose pleural fluid characteristics were compatible with PL-TB. Among these patients, 19 patients exhibiting other evidence of TB were excluded: AFB smear-positive pleural fluid (n=5), TB-PCR-positive pleural fluid (n=11), and AFB smear-positive sputum (n=6). Some patients showed positive results on more than one test. Bronchoscopy was performed in the remaining 54 patients, whose clinical characteristics are displayed in Table 1. The median age was 59 years (range, 19-94 years) and 33 (61%) were male. Eleven (20%) patients had a history of previous TB. A total of 32 (59%) patients received a diagnosis of PL-TB by bacteriology; culture of pleural fluid and BA was positive in 11 (20%) and 27 (50%) patients, respectively, and 16 (42%) out of 38 patients with sputum available resulted in positive culture. Four (7%) patients were diagnosed pathologically, and the other 18 (33%) patients were diagnosed clinically. None of the patients were seropositive for human immunodeficiency virus.
Pulmonary parenchymal lesions were observed on simple chest radiographs in 25 (46%) patients. In contrast, chest CT scans revealed parenchymal lesions in a total of 40 (74%) patients. Nodular (59%) and patchy (37%) infiltrations were the most common form of parenchymal lesion, and cavitary lesions were found in three (6%) patients (Table 1). The involvement of lung lesions on chest CT was ≤segmental in 34 (85%) patients and >segmental in 6 (15%). No patient exhibited more than lobar involvement.
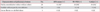
Table 2 displays the early (AFB smear- or TB-PCR-positive) and delayed (culture-positive) diagnostic yields of BA, compared between patients with present or absent pulmonary parenchymal lesions on chest radiograph or chest CT. According to the classification by chest radiograph, early-positive results (TB-PCR-positive, AFB smear-positive, or double-positive) were observed in 16 (64%) and six (21%) of the patients with and without pulmonary lesions, respectively (p=0.001). In the classification by chest CT, early-positive results were obtained in 21 (53%) and one (7%) of the patients with and without pulmonary lesions, respectively (p=0.003). The BA TB-PCR test was positive in 21 (95%) out of 22 patients, with early-positive results in both imaging modalities.
According to the classification by chest radiograph, delayed-culture results were positive in 18 (72%) out of 25 and 9 (31%) out of 29 patients with and without pulmonary lesions, respectively (p=0.003). In the classification by chest CT, culture results were positive in 26 (65%) of 40 and one (7%) of the 14 patients with and without pulmonary lesions, respectively (p<0.001). Some patients exhibited culture-positive results alone, without early-positive results; such cases were less frequent among patients without pulmonary lesions on chest CT scans than among patients without lesions on chest radiographs. A TB-PCR-positive but culture-negative BA result was obtained in one patient with and one patient without pulmonary lesions on chest radiograph and CT. These two patients had no previous TB history, and both cases were ultimately diagnosed by sputum culture and clinical decision, respectively.
Three of eleven patients with past TB history gave TB-PCR-positive BA results. They all exhibited pulmonary parenchymal lesions on both imaging modalities and also exhibited AFB smear-positive and culture-positive BA results, indicating that the TB-PCR results reflected true positives.
Among 20 patients with patchy consolidations on chest CT, other parenchymal lesions were accompanied in 17 patients. Those parenchymal lesions included nodular (n=16), linear-fibrotic (n=4), mass-like (n=3), cavitary (n=3), and/or calcified lesions (n=3). The remaining three patients had patchy consolidative lesions alone. These patchy consolidative lesions with or without other findings were associated with significantly higher positive rates for AFB smear (p=0.032), TB-PCR (p<0.001), and culture results (p<0.001), relative to other lesions, i.e., nodular lesions without patchy consolidative lesions (n=16) and linear-fibrotic or calcified lesions alone (n=4) (Table 3). Among BA results from 20 patients with patchy consolidative lesions, eight (40%) were AFB smear-positive, 18 (90%) were TB-PCR-positive, and 19 (95%) were culture-positive. One patient with patchy lesions who gave a culture-negative result was also negative for the AFB smear and TB-PCR tests but had subtle consolidation resembling ground-glass opacity on his chest CT. This patient was finally diagnosed by histological examination. Among sixteen patients who had nodular lesions without patchy infiltrations, only one (6%) was AFB smear-positive, two (13%) were TB-PCR-positive, and seven (44%) were culture-positive. Patients with linear or calcified lesions alone all gave negative results.
This study confirmed that over two-thirds of cases with PL-TB were associated with pulmonary parenchymal lesions on chest CT, and showed that the absence of parenchymal lesions on chest CT was a significant negative predictor for obtaining early and delayed diagnostic results by the bronchoscopic approach. In contrast, chest CT findings of patchy consolidation gave satisfactory early diagnostic yields (by BA TB-PCR) and confirmative diagnostic yields (by culture results) for PL-TB.
Analysis of pleural fluid through diagnostic thoracentesis provides useful information regarding the possible cause of pleural effusion. High ADA levels obtained in lymphocyte-predominant exudates strongly suggest a tuberculous origin3,4. However, some other diseases are also associated with similar high ADA levels in lymphocyte-predominant exudates7. Thus, clinicians often make efforts, such as pleural biopsy, to obtain further evidence indicating TB, especially in an area with a low incidence of TB. Diacon et al.17 reported a direct comparative study between thoracoscopic and closed-needle pleural biopsies in PL-TB; they found that the sensitivity of histology and culture was 100% and 76%, respectively, for thoracoscopy, and 66% and 48%, respectively, for closed-needle biopsy. However, thoracoscopy is more invasive and is of limited availability in many parts of the world, whereas closed-needle biopsy is less invasive but less sensitive and requires large pleural effusions for the blind use of the devices used6,17-19. Furthermore, although closed pleural biopsy may often be the procedure of first choice in resource-poor areas with a high incidence of TB, the fall in the incidence of TB in most of the developed world over the last 50 years has led to an equally significant reduction in operator experience among respiratory physicians1,6. Therefore, if possible, it is desirable to establish a diagnosis swiftly while minimizing unnecessary invasive investigations and facilitating treatment.
Sputum study is routinely recommended in patients suspected of having PL-TB. The diagnostic yields of respiratory specimens, such as sputum or BA, may be predicted to depend primarily on the parenchymal lesions. However, in the study of Conde et al.8, these parenchymal lesions (as assessed by chest radiograph) did not correlate with the culture yields of induced sputum for MTB. Even in this study, the culture yields of BA for MTB were 31% in patients without pulmonary lesions on chest radiograph. In contrast to chest radiograph, patients without parenchymal lesions on CT scan showed only a 7% positive culture rate. These findings indicate that the absence of parenchymal pulmonary lesions on chest CT is unlikely to confer a diagnostic benefit, even in conjunction with the bronchoscopic approach.
The mycobacterial burden of pulmonary TB is proportionally increased in cases of consolidative CT findings20, whereas the number of bacilli in solid nodular lesions ranges from 102-104, a lower bacillary burden21. These findings explain why patchy consolidative lesions gave the best results for the detection of MTB, compared to other CT findings in our study (Table 3). The significant differences in the diagnostic yields of bronchoscopic evaluation according to chest CT findings may suggest that this approach should be decided after considering the characteristics of parenchymal lesions on chest CT.
In the setting of presumptive PL-TB strongly suggested by high ADA levels and lymphocyte-predominant exudates, our study was conducted for rapidly obtaining additional evidence for PL-TB. The BA TB-PCR test was positive in 21 (95%) out of 22 patients with early-positive results (Table 2). In addition, these TB-PCR-positive results were mainly observed in patients with patchy consolidative CT findings (Table 3). Consequently, a BA TB-PCR test based solely on consolidative CT findings seems satisfactory for this purpose. The diagnostic value of the BA TB-PCR test is already well known in the smear-negative pulmonary TB field10-12. BA AFB smear is cheap but limited by low sensitivity, whereas BA culture is the most sensitive but takes the most time. In contrast, the BA TB-PCR test has good diagnostic accuracy, in terms of rapid detection of TB, in these patients. Thus, it is not surprising that the diagnostic yield in our study, specifically regarding the BA TB-PCR test on PL-TB patients with parenchymal lesions on chest CT, is in line with the results of previous studies regarding the BA TB-PCR test in subjects with smear-negative pulmonary TB. However, the BA TB-PCR test gave limited diagnostic yields in cases without patchy consolidation on CT scan.
In pleural fluid samples, TB-PCR-positive results cannot predict culture-positive results, as shown in several reports22-24. In BA, however, TB-PCR-positive results were reliably followed by culture-positive results, in contrast to the inconsistent bacteriologic relationship between these tests in pleural fluid. This relationship was apparent in our study as well as in previous smear-negative pulmonary TB studies10-12. This consistency of findings may represent an additional advantage of the parenchymal approach, which also enables subsequent drug-sensitivity tests in patients with PL-TB. Actually, two patients among 27 patients with drug-sensitivity tests available in this study showed resistance to one or more of anti-tuberculous drugs (one patient, resistance to isoniazid alone; the other, resistance to isoniazid and pyrazinamide), which required modification of treatment regimen and/or duration.
Our study has several limitations. Firstly, the sample size was small. However, we believe that study of a large population would not significantly alter the diagnostic yields obtained for cases accompanied by patchy consolidative lesions on chest CT. Secondly, we did not conduct induced sputum or sputum TB-PCR tests. These tests may be more useful in resource-poor settings, whereas the bronchoscopic approach may be preferable in developed countries. In addition, the sputum TB-PCR test cannot predict reliably culture results of a separate sputum sample because the sputum TB-PCR and culture tests are usually performed on different sputum samples22. Thirdly, other causes of pleural effusion cannot be fully excluded in some patients with clinically diagnosed PL-TB. However, all of them demonstrated clinical and radiographic improvement upon anti-TB medication without other possible causes of pleural effusion on the basis of lymphocyte-predominant exudates and ADA levels ≥40 U/L.
In conclusion, more than one-third of patients with suspected PL-TB had patchy consolidative parenchymal lesions on chest CT. Performing bronchoscopy with TB-PCR test in these patients may be useful for rapid diagnosis with a confirmative culture result, enabling a subsequent drug-sensitivity test. In the modern era, chest CT is frequently used for initial differential diagnosis. We have shown that characteristic chest CT findings predict the diagnostic yields of the bronchoscopic approach, which may be preferable to the thoracoscopic approach in patients with suspected PL-TB and associated patchy consolidative CT findings.
Figures and Tables
Table 2
Diagnostic yields of bronchial aspirate between patients with (+) and without (-) parenchymal pulmonary lesions on chest radiograph and CT

Values are presented as number (%) of patients with a positive result.
CT: computed tomography; Pul: pulmonary; AFB: acid-fast bacilli; TB-PCR: tuberculosis-polymerase chain reaction; MTB: Mycobacterium tuberculosis.
*p=0.001, †p=0.003, ‡p=0.003, and §p<0.001 compared with the absence of pulmonary lesions on the corresponding imaging modalities.
References
1. Hooper C, Lee YC, Maskell N. BTS Pleural Guideline Group. Investigation of a unilateral pleural effusion in adults: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010; 65:Suppl 2. ii4–ii17.
2. Moon JW, Chang YS, Kim SK, Kim YS, Lee HM, Kim SK, et al. The clinical utility of polymerase chain reaction for the diagnosis of pleural tuberculosis. Clin Infect Dis. 2005; 41:660–666.
3. Light RW. Update on tuberculous pleural effusion. Respirology. 2010; 15:451–458.
4. Porcel JM. Tuberculous pleural effusion. Lung. 2009; 187:263–270.
5. Laniado-Laborin R. Adenosine deaminase in the diagnosis of tuberculous pleural effusion: is it really an ideal test? A word of caution. Chest. 2005; 127:417–418.
6. Koegelenberg CF, Diacon AH. Pleural controversy: close needle pleural biopsy or thoracoscopy-which first? Respirology. 2011; 16:738–746.
7. Gopi A, Madhavan SM, Sharma SK, Sahn SA. Diagnosis and treatment of tuberculous pleural effusion in 2006. Chest. 2007; 131:880–889.
8. Conde MB, Loivos AC, Rezende VM, Soares SL, Mello FC, Reingold AL, et al. Yield of sputum induction in the diagnosis of pleural tuberculosis. Am J Respir Crit Care Med. 2003; 167:723–725.
9. Kim HJ, Lee HJ, Kwon SY, Yoon HI, Chung HS, Lee CT, et al. The prevalence of pulmonary parenchymal tuberculosis in patients with tuberculous pleuritis. Chest. 2006; 129:1253–1258.
10. Tueller C, Chhajed PN, Buitrago-Tellez C, Frei R, Frey M, Tamm M. Value of smear and PCR in bronchoalveolar lavage fluid in culture positive pulmonary tuberculosis. Eur Respir J. 2005; 26:767–772.
11. Lee JE, Lee BJ, Roh EY, Kim DK, Chung HS, Lee CH. The diagnostic accuracy of tuberculosis real-time polymerase chain reaction analysis of computed tomography-guided bronchial wash samples. Diagn Microbiol Infect Dis. 2011; 71:51–56.
12. Lee J, Lee SY, Yoo SS, Cha SI, Won DI, Park JY, et al. Clinical value of whole-blood interferon-gamma assay in patients with suspected pulmonary tuberculosis and AFB smear- and polymerase chain reaction-negative bronchial aspirates. Diagn Microbiol Infect Dis. 2012; 73:252–256.
13. Feinsilver SH, Barrows AA, Braman SS. Fiberoptic bronchoscopy and pleural effusion of unknown origin. Chest. 1986; 90:516–519.
14. Chang SC, Perng RP. The role of fiberoptic bronchoscopy in evaluating the causes of pleural effusions. Arch Intern Med. 1989; 149:855–857.
15. Heaton RW, Roberts CM. The role of fibreoptic bronchoscopy in the investigation of pleural effusion. Postgrad Med J. 1988; 64:581–582.
16. Light RW, Macgregor MI, Luchsinger PC, Ball WC Jr. Pleural effusions: the diagnostic separation of transudates and exudates. Ann Intern Med. 1972; 77:507–513.
17. Diacon AH, Van de Wal BW, Wyser C, Smedema JP, Bezuidenhout J, Bolliger CT, et al. Diagnostic tools in tuberculous pleurisy: a direct comparative study. Eur Respir J. 2003; 22:589–591.
18. Valdes L, Alvarez D, San Jose E, Penela P, Valle JM, Garcia-Pazos JM, et al. Tuberculous pleurisy: a study of 254 patients. Arch Intern Med. 1998; 158:2017–2021.
19. Ruan SY, Chuang YC, Wang JY, Lin JW, Chien JY, Huang CT, et al. Revisiting tuberculous pleurisy: pleural fluid characteristics and diagnostic yield of mycobacterial culture in an endemic area. Thorax. 2012; 67:822–827.
20. Matsuoka S, Uchiyama K, Shima H, Suzuki K, Shimura A, Sasaki Y, et al. Relationship between CT findings of pulmonary tuberculosis and the number of acid-fast bacilli on sputum smears. Clin Imaging. 2004; 28:119–123.
21. Canetti G. Present aspects of bacterial resistance in tuberculosis. Am Rev Respir Dis. 1965; 92:687–703.
22. Kumar P, Sen MK, Chauhan DS, Katoch VM, Singh S, Prasad HK. Assessment of the N-PCR assay in diagnosis of pleural tuberculosis: detection of M. tuberculosis in pleural fluid and sputum collected in tandem. PLoS One. 2010; 5:e10220.
23. Rosso F, Michelon CT, Sperhacke RD, Verza M, Olival L, Conde MB, et al. Evaluation of real-time PCR of patient pleural effusion for diagnosis of tuberculosis. BMC Res Notes. 2011; 4:279.
24. de Lassence A, Lecossier D, Pierre C, Cadranel J, Stern M, Hance AJ. Detection of mycobacterial DNA in pleural fluid from patients with tuberculous pleurisy by means of the polymerase chain reaction: comparison of two protocols. Thorax. 1992; 47:265–269.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download