Abstract
Background
Notified tuberculosis (TB) cases in Korea have not decreased over the last decade (2001-2010).
Methods
To clarify the reasons, we analyzed an annual report on notified tuberculosis patients and age-specific population drift in Korea.
Results
Compared to the age-specific notified TB cases between 2001 and 2010, distinctive features in notified TB cases and new cases increased markedly in people aged 45-54 years and in patients over 65 years old, whereas those between 15-34 years in 2010 decreased drastically. In particular, notified TB individuals over 65 years old occupied 29.6% of the cases in 2010, which was 1.5 times higher than that in 2001. The main reason not to decrease in notified TB patients for the last decade (2001-2010) was due to the increasing elderly population as well as the aging of baby boomers, which have a higher risk of TB development.
Tuberculosis (TB) is still a global epidemic that needs to be controlled. Globally, 8.7 million new cases of TB were estimated in 2011 and over half (60%) were allocated in Asia1. Globally, 125 incident cases per 100,000 people were estimated, which included 100 in the Republic of Korea in 20111.
The prevalence of TB in Korea has decreased from 1965 to 1995 (radiologically active cases and the active case rate aged over 5 years have decreased from 5,168 to 767 per 100,000 population)2.
Healthcare facilities should report clinical information on TB patients and suspected TB patients to the Korea Tuberculosis Information Management System (TBnet) according to the Korean Tuberculosis Preventive Law. The TBnet, established in 2000, is an online tuberculosis surveillance system in both public and private sectors that substituted the national TB actual condition surveillance every 5 years from 1965 to 199514.
This analysis was based on an annual report that is composed of notified TB patients through the TBnet in Korea3-13.
Notified TB cases were counted from the 1st of January to the 31st of December every year. All notified TB cases were used in statistical analysis after filtering out double-notified patients by full name, social security number, and date of treatment etc.
The data regarding the Korean population was derived from Korean Statistics.
Notified TB cases were the total of TB patients and suspected TB patients that were notified through TBnet. A TB patient was defined as an individual who was smear-positive or culture-positive for Mycobacterium tuberculosis from a patient specimen (sputum, blood, urine, cerebrospinal fluid, tissues, etc.)3-13. A suspected TB patient was defined as an individual having all clinical, radiological, and histological results indicating TB infection although not confirmed by a positive M. tuberculosis bacilli on the smear and culture examination3-13.
This study had a limitation which notified TB cases were fewer than TB cases from the Nationwide Medical Records Survey of Patients with TB or Health Insurance Review and Assessment service15,16. In addition, notified TB cases might include a few of non-tuberculous mycobacteria (NTM) cases among suspected TB cases, because the proportion of NTM is recently increasing in Korea17,18.
The case notification rate was calculated as the total number of notified TB cases divided by a midterm (1st of July) population of the year received from Statistics Korea, and then multiplied by 100,000. The notified new TB rates per 100,000 was obtained by using the same formula as the case notification rate except it was counted as new TB patients among the notified cases in the year. This study has the limitation of the notified TB system, which should be affected by the notification rate. This means that the data was not based on precise prevalence or an incidence survey.
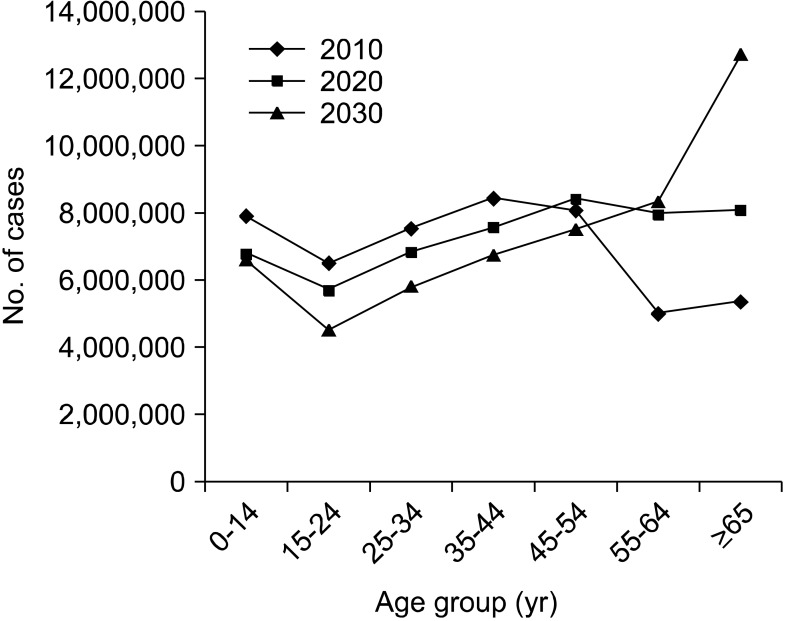
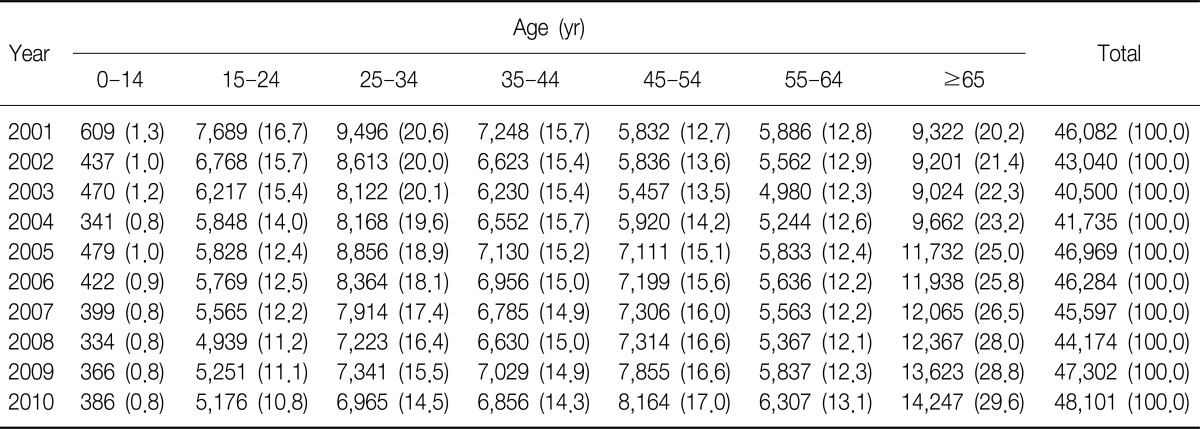
Total notified TB cases have not decreased during the last decade (Table 1). Compared to the age-specific notified TB cases between 2001 and 2010, distinctive features regarding TB cases markedly increased in 45-54 year olds and in people over 65 year olds, but decreased dramatically among the 15-34 year olds in 2010 (Table 1, Figure 1). These features were also identical in the new pulmonary TB cases confirmed by only culture examination (Table 2) or the suspected new TB cases (data not shown).
In the identical period, the age-specific notified TB rates per 100,000 for all age groups have decreased slightly (Figure 2). In particular, a reduction of notified TB rates per 100,000 in 15-34 year olds and 55-64 year olds is conspicuous. A high TB rate in younger age is usually a typical pattern in high TB-burdened countries, and a declining TB rate for this age means that TB control is improving.
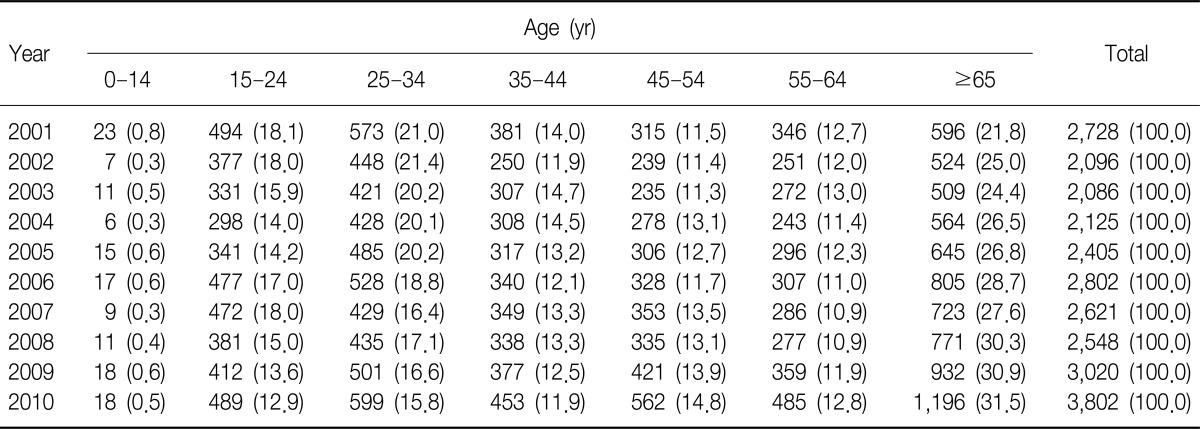
New TB cases also increased in the over 45 year olds, especially, the over 65 year olds TB patients who occupy 29.6% of the total new cases in 2010 (Table 3, Figure 3). However, the notified new TB rates per 100,000 have decreased in all age groups under the age of 65 (Table 3).
Smear-positive pulmonary TB patients are regarded as a source of new TB infection. Fortunately, total smear-positive numbers have not increased for the last decade (2001-2010), however, the proportion of over 45 year olds occupied 65.3% of the total smear-positive, new pulmonary TB patients in 2010 (Table 3).
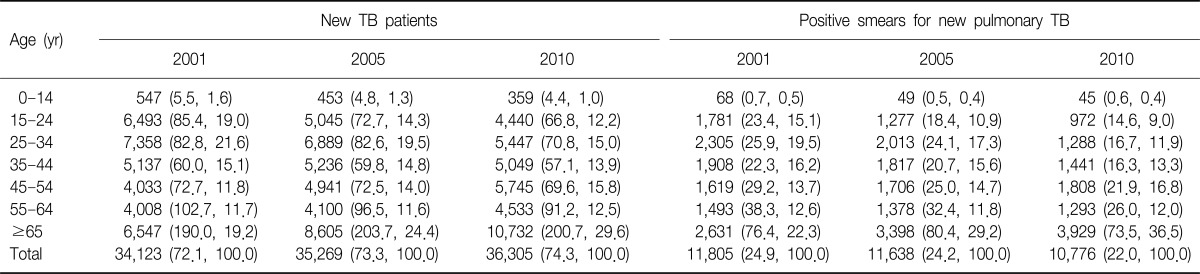
We found demographic change that older age groups have increased steadily while younger age groups have decreased from 1980 to 2010 (Figure 4). The population of individuals over 45 year olds has steadily increased every 10 years. The rapid increase in the older aged population might result from the development of medical technology as well as a favorable socioeconomic situation in Korea.
Conspicuous age shift was found in the 25-34 year olds in 1990, 35-44 year olds in 2000 and 45-54 year olds in 2010 (Figure 4). This big population shift includes the baby boomer generation (born 1955-1963 in Korea). Therefore, aging of this generation contributed to increased TB cases notwithstanding the declining TB rate on the population constitution. The change of population constitution was the main cause of slowing the improved control of TB in Korea.
To make matters worse in terms of TB control, Statistics Korea projected that the older aged population will increase for a few more decades in the future (Figure 5).
The age-specific incidence rate of TB is usually higher in younger individuals in high burdened TB countries, but in the older populations in lower burdened TB countries20. TB prevalence in Korea has been declining from 1965 to 1995 according to the TB survey2. However, notified TB patients have not decreased recently according to the notified TB system since 2000. Through this study, we found that Korea has been a rapidly aging society since 2000, and the demographic transition seems to be a hindrance to national TB control.
Moreover, the baby boomer generation (born 1955-1963), which occupies a large portion (about 15%) of the Korean population has approached the advanced age groups. Those people have lived during a high TB-exposed period after the Korean War (1950-1953) and should have high rates of latent TB infection.
Furthermore, the Republic of Korea has had a greater longevity and lower fertility for the last decade (2001-2010). This situation tends to increase the prevalence of TB infection; because the higher the proportion of old aged people within the population constitution, the higher the proportion of latent TB infected individuals, which results in higher opportunity to develop active TB by reactivation21.
Similarly, according to a retrospective study in Hong Kong, the incidence rate of TB in over 45 year olds did not decrease as was predicted, especially in people over 65 year olds, which remained static for two decades22.
In the mice model, CD4+ T cell responses in old age during infection with M. tuberculosis are declined when compared young mice23. This defect may also be responsible for the increased susceptibility of M. tuberculosis in elderly individuals. In addition, age-associated diseases such as malignancy and diabetes mellitus may increase the risk of TB in the elderly population24.
Also, the improvement of the survival rate through the enhancement of TB treatment should result in the accumulation of TB patients in old age and an increased prevalence of TB.
TB symptoms in old age have some unique characteristics, and it necessary to perform detailed examinations in order to detect TB in patients. Further, TB in old age has higher primary anti-tuberculous drug resistance and side effects than the younger population, making it more difficult to treat the elderly with TB25-27. Therefore, TB in old age is difficult to control even in the low TB-burdened countries28-30. The notified new TB rate per 100,000 for each age group in Korea was still higher than Taiwan in the younger age groups or Japan in all age groups30,31.
The Korean Center for Disease Control and Prevention (KCDC) launched the "New 2020 Plan for the Elimination of Tuberculosis in Korea" in 2010. The major goals of the 2020 plan are the reduction of the incidence of smear-positive TB and TB mortality from 20 to 10, and from 4.3 to 2.3 per 100,000, respectively, and an increase in TB treatment success rates of new smear-positive TB patients from 85% to 95%.
The KCDC struggles to achieve these goals with various action plans such as the expansion of private-public mix, directly observed treatment and short-course drug therapy, prophylactic medicine to latent tuberculosis infection, the establishment of a TB management system for TB vulnerable groups including the homeless, and the improvement of the diagnostic system for early TB detection, among others.
We need to give special consideration towards an action plan regarding the elderly population in order to successfully achieve the 2020 goals through effective TB control.
References
1. World Health Organization. Global tuberculosis report 2012. WHO/HTM/TB/2012.6. 2012. Geneva: World Health Organization.
2. Hong YP, Kim SJ, Lew WJ, Lee EK, Han YC. The seventh nationwide tuberculosis prevalence survey in Korea, 1995. Int J Tuberc Lung Dis. 1998; 2:27–36. PMID: 9562108.
3. Korean Center for Disease Control and Prevention. Annual report on the notified tuberculosis patients in Korea, 2001. 2002. Seoul: Korean Center for Disease Control and Prevention.
4. Korean Center for Disease Control and Prevention. Annual report on the notified tuberculosis patients in Korea, 2002. 2003. Seoul: Korean Center for Disease Control and Prevention.
5. Korean Center for Disease Control and Prevention. Annual report on the notified tuberculosis patients in Korea, 2003. 2004. Seoul: Korean Center for Disease Control and Prevention.
6. Korean Center for Disease Control and Prevention. Annual report on the notified tuberculosis patients in Korea, 2004. 2005. Seoul: Korean Center for Disease Control and Prevention.
7. Korean Center for Disease Control and Prevention. Annual report on the notified tuberculosis patients in Korea, 2005. 2006. Seoul: Korean Center for Disease Control and Prevention.
8. Korean Center for Disease Control and Prevention. Annual report on the notified tuberculosis patients in Korea, 2006. 2007. Seoul: Korean Center for Disease Control and Prevention.
9. Korean Center for Disease Control and Prevention. Annual report on the notified tuberculosis patients in Korea, 2007. 2008. Seoul: Korean Center for Disease Control and Prevention.
10. Korean Center for Disease Control and Prevention. Annual report on the notified tuberculosis patients in Korea, 2008. 2009. Seoul: Korean Center for Disease Control and Prevention.
11. Korean Center for Disease Control and Prevention. Annual report on the notified tuberculosis patients in Korea, 2009. 2010. Cheonwon: Korean Center for Disease Control and Prevention.
12. Korean Center for Disease Control and Prevention. Annual report on the notified tuberculosis patients in Korea, 2010. 2011. Cheonwon: Korean Center for Disease Control and Prevention.
13. Korean Center for Disease Control and Prevention. Annual report on the notified tuberculosis patients in Korea, 2011. 2012. Cheonwon: Korean Center for Disease Control and Prevention.
14. Lew WJ, Lee EG, Bai JY, Kim HJ, Bai GH, Ahn DI, et al. An Internet-based surveillance system for tuberculosis in Korea. Int J Tuberc Lung Dis. 2006; 10:1241–1247. PMID: 17131783.
15. Park YS, Hong SJ, Boo YK, Hwang ES, Kim HJ, Cho SH, et al. The national status of tuberculosis using nationwide medical records survey of patients with tuberculosis in Korea. Tuberc Respir Dis. 2012; 73:48–55.

16. Hong SJ, Park YS, An H, Kang SM, Cho EH, Shin SS. Factors leading to under-reporting of tuberculosis in the private sector in Korea. Int J Tuberc Lung Dis. 2012; 16:1221–1227. PMID: 22794136.

17. Yoo JW, Jo KW, Kim MN, Lee SD, Kim WS, Kim DS, et al. Increasing trend of isolation of non-tuberculous mycobacteria in a tertiary university hospital in South Korea. Tuberc Respir Dis. 2012; 72:409–415.

18. Lee SK, Lee EJ, Kim SK, Chang J, Jeong SH, Kang YA. Changing epidemiology of nontuberculous mycobacterial lung disease in South Korea. Scand J Infect Dis. 2012; 44:733–738. PMID: 22720876.

19. Statistics Korea [Internet]. cited 2012 Oct 30. Daejeon: Statistics Korea;Available from: http://kostat.go.kr/.
20. Mori T, Leung CC. Tuberculosis in the global aging population. Infect Dis Clin North Am. 2010; 24:751–768. PMID: 20674802.

21. Dye C, Williams BG. The population dynamics and control of tuberculosis. Science. 2010; 328:856–861. PMID: 20466923.

22. Vynnycky E, Borgdorff MW, Leung CC, Tam CM, Fine PE. Limited impact of tuberculosis control in Hong Kong: attributable to high risks of reactivation disease. Epidemiol Infect. 2008; 136:943–952. PMID: 17678555.

23. Vesosky B, Turner J. The influence of age on immunity to infection with Mycobacterium tuberculosis. Immunol Rev. 2005; 205:229–243. PMID: 15882357.
24. Rajagopalan S. Tuberculosis and aging: a global health problem. Clin Infect Dis. 2001; 33:1034–1039. PMID: 11528577.

25. Rajagopalan S, Yoshikawa TT. Tuberculosis in the elderly. Z Gerontol Geriatr. 2000; 33:374–380. PMID: 11130191.

26. Lee JH, Han DH, Song JW, Chung HS. Diagnostic and therapeutic problems of pulmonary tuberculosis in elderly patients. J Korean Med Sci. 2005; 20:784–789. PMID: 16224152.

27. Thrupp L, Bradley S, Smith P, Simor A, Gantz N, Crossley K, et al. Tuberculosis prevention and control in long-term-care facilities for older adults. Infect Control Hosp Epidemiol. 2004; 25:1097–1108. PMID: 15636299.

28. Hauer B, Brodhun B, Altmann D, Fiebig L, Loddenkemper R, Haas W. Tuberculosis in the elderly in Germany. Eur Respir J. 2011; 38:467–470. PMID: 21804163.

29. Yamagishi F. Tuberculosis in the elderly. Kekkaku. 2004; 79:481–486. PMID: 15484832.
30. Lo HY, Chou P, Yang SL, Lee CY, Kuo HS. Trends in tuberculosis in Taiwan, 2002-2008. J Formos Med Assoc. 2011; 110:501–510. PMID: 21783019.

31. Research Institute of Tuberculosis. JATA. Tuberculosis annual report 2009. Series 4. Elderly TB. Kekkaku. 2011; 86:737–741. PMID: 21922784.
Figure 1
Comparison of age-specific notified tuberculosis (TB) cases between 2001 and 2010. Distinctive features of TB cases markedly increased in 45-54 year olds and those over 65 year olds in 2010.
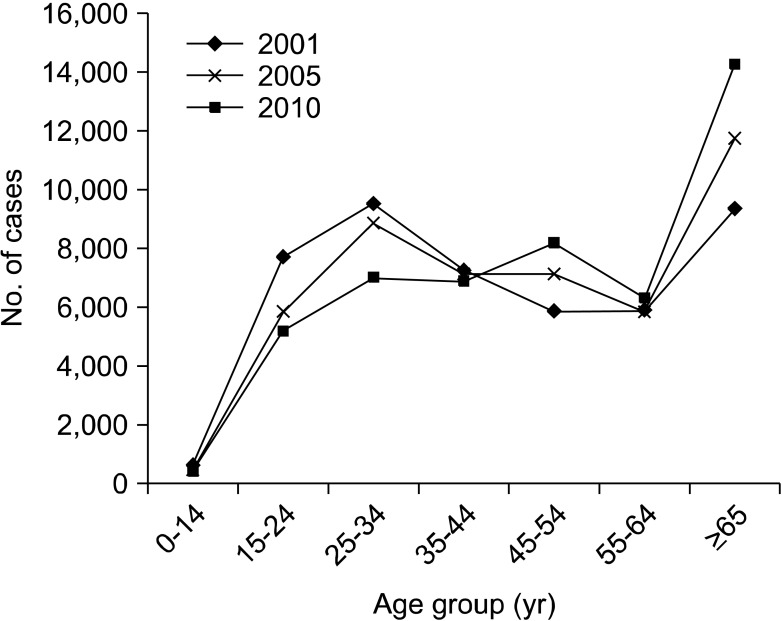
Figure 2
Comparison of notified age-specific tuberculosis (TB) rates per 100,000 people between 2001 and 2010. The TB rates in 2010 were reduced in all age groups compared to 2001.
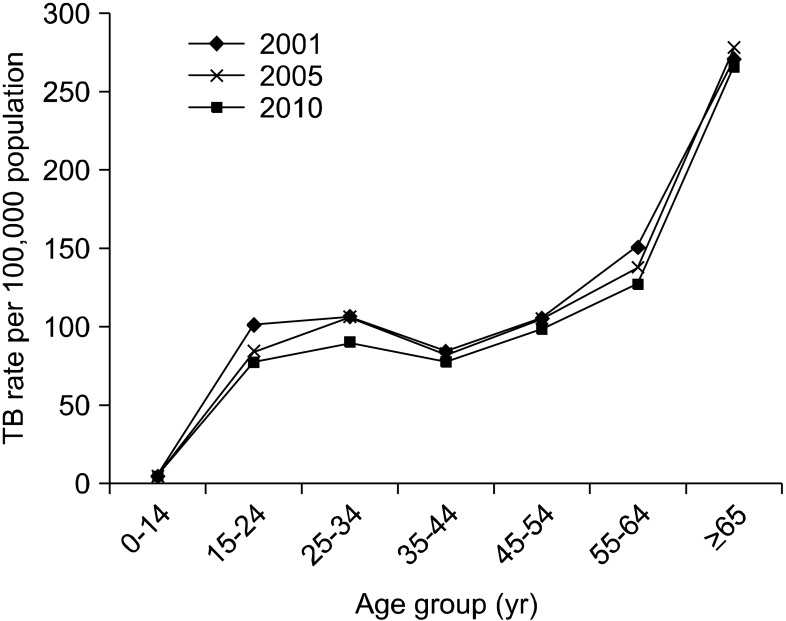
Figure 3
Trend of age-specific notified new tuberculosis (TB) cases for the last decade (2001-2010). New TB cases increased in those over 45 year olds, particularly in individuals aged 65 or over compared to 2001 TB patients in 2010.
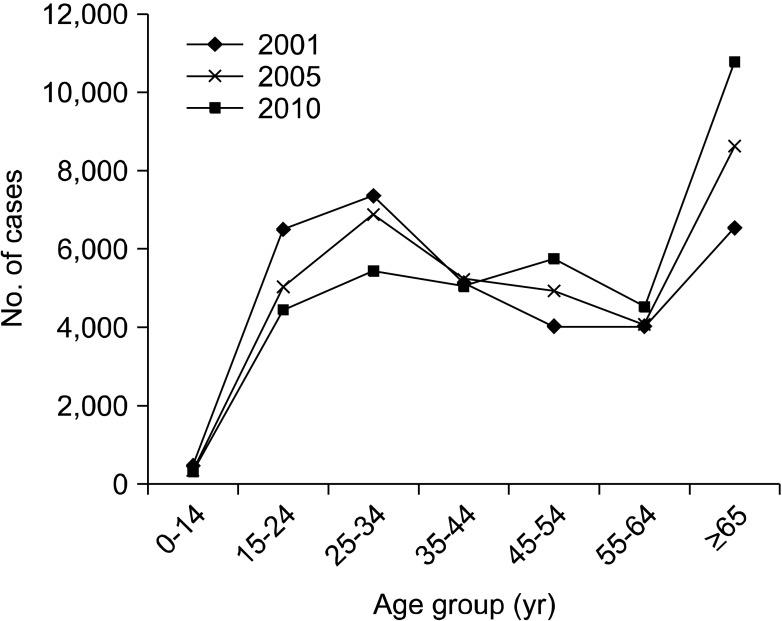
Figure 4
Demographic change of age specific population from 1980 to 2010. The old age group has increased steadily while the younger age group has decreased.
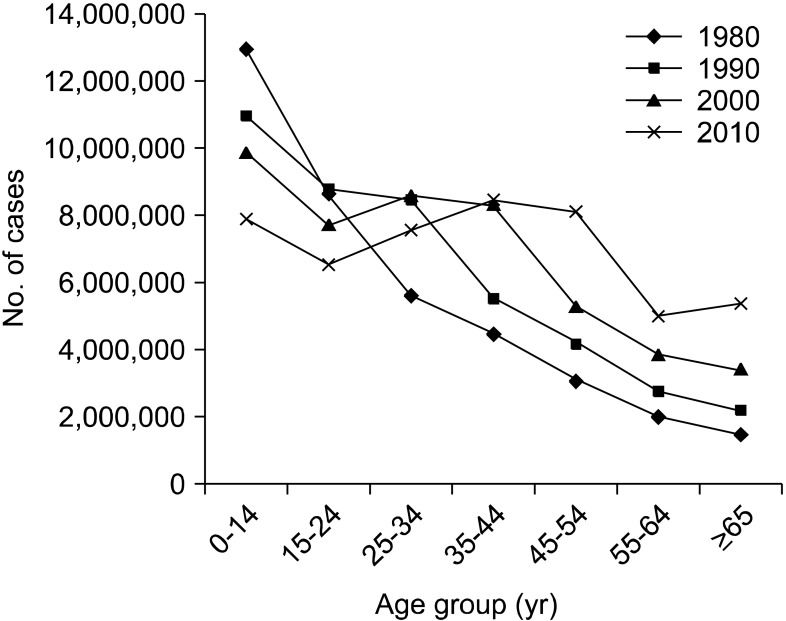
Figure 5
Prospective age-specific populations in the future (data from Statistics Korea)19. Baby boomers would be the main cause for the increasing old age group.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download