Abstract
Broncholiths are defined as calcified materials that occur in a tracheobronchial tree or in a cavity communicating with that. Broncholith has variable clinical features. The therapeutic options to remove broncholiths are so variable that clinicians need to select the most safe and effective methods by mass size, mobility, and location. As yet, there is no consistent guideline removing a broncholith. We report 2 successful cases of removing a fixed broncholith by flexible bronchoscopy guided cryoadhesion. With repeated technique of thawing and freezing with ryoprobe, we could extract the fixed broncholith safely. This method is promising as a way to remove broncholith in the future.
Broncholith is calcified material within tracheobronchial tree. The therapeutic options are so variable that clinicians should choose the proper way to remove it considering by mass size, mobility, location, patient's symptoms. As yet, for removing broncholith, flexible bronchoscopy has been applied only in limited cases. We report here on 2 cases of successful removal of broncholith using cryotherapy-assisted flexible bronchoscopy.
A 32-year-old female was admitted on the chief complaint of blood-tinged sputum and fever for 3 weeks. The patient had an episode of hemoptysis 3 years ago at which she was treated with for pulmonary tuberculosis.
The patient complained of fever, myalgia and sweating for 3 weeks and physical examination revealed decreased lung sounds and crackles on right upper lung filed.
Chest radiographs showed multifocal ill defined patchy, nodular densities in the right upper lobe; therefore, a chest computed tomography (CT) scan was performed. Chest CT suggested a mass-like calcified endobronchial lesion and post-obstructive pneumopathy (Figure 1A).
Bronchoscopy was performed to examine the endobronchial lesion. On bronchoscopy, a fixed broncholith with sharp and speculated margins was seen (Figure 2A). At the opening of right upper lobe bronchus, it was difficult to approach the orifice due to nearly total obstruction with the impacted mass. Immediate cryotherapy was performed to extract the broncholith. Just 5 seconds freezing without thawing, we could fInd the cryoprobe stucked to the broncholith. We forced the probe which was attached to the mass backward. There was a small amount of bleeding. A bleeding control with argon plasma coagulation (APC) was successfully done without major complications. The extracted broncholith was 1.8 cm sized and attached bronchial mucosa with irregular margin (Figure 2B).
Tuberculosis study including both acid fast bacilli stain and tuberculosis polymerase chain reaction were negative and no pathogen was identified on cultures. Obstructive pneumonia improved (Figure 1B) and the patient was followed on out-patient department on routine basis without anti-tuberculosis medication.
A 32-year-old man visited for management of hemoptysis for 5-days. He has a history of 10 pack-year smoking and incomplete treatment of pulmonary tuberculosis 17 years ago. This was the second episode of massive hemoptysis.
At his first admission, the hemoptysis resolved with conservative management and thus he was discharged without any invasive management for removing the broncholith.
Chest CT on this admission showed ill defined patchy consolidation and ground glass opacities surrounding lingular segment and a calcified density within Lt. upper lobar bronchus suggesting broncholith with pulmonary hemorrhage (Figure 3A).
Bronchoscopy showed 1.5 cm sized yellowish mass (probably broncholith) at left upper lobe lingular division (Figure 4A).
Follow-up bronchoscopy and cryoadhesion were performed. We performed the freezing procedure about 5 seconds. The cryoprobe stucked to the mass, but we could not force the probe backward because the broncholith was tightly fastened to the bronchial wall. For thawing procedure, we waited for another 10 seconds, which made the linkage between the probe and the broncholith weakened. By repeating freezing-thawing techinique 5 times, the stucked mass became movable due to the damaged bronchial wall. So we could extract the total broncholith completely (Figure 4B) and additional APC was done for bleeding control. After 1 week, follow-up chest CT shows patent airway without broncholith and hemorrhage resorption (Figure 3B).
Broncholiths are endogenous calcified material within tracheobronchial tree. Its pathogenesis can be explained in three mechanisms. First, inhaled materials in the bronchus mixed up with calcium develop into broncholith. Second, bronchial cartilage is either calcified or ossified which then breaks apart in the endobronchial spaces. Third, the most common cause, lung parenchymal infection progresses and brings about calcium deposits in lymph nodes under alkalic environment1.
Major diseases that cause such symptoms as mentioned above include tuberculosis in Korea and Europe, while in US it is histoplasma. Occasionally they are also caused by fungal infection, lung abscess, pulmonary infarction, silicosis or inhalation of foreign materials2.
Depending on the location of the broncholith and the extent of bronchial erosion, clinical manifestations range from asymptomatic, mild coughing and sputum to hemoptysis, chest pain, fever, secondary pneumopathy, bronchiectasis and atelectasis. Whereas conservative care is adequate in patient with cough, hemoptysis and obstructive pneumopathy, surgical intervention such as lobectomy, segmentectomy or even pneumonectomy are rarely needed in some cases of refractory hemoptysis or obstructive pneumopathy suggestive of lung cancer1.
In clinical settings, broncholiths are often detected during evaluating symptoms of complications such as hemoptysis or recurrent pulmonary infections. If complications develop, both symptomatic care and the removal of broncholiths are often needed.
Even if a proper symptomatic care was done, recurrent symptoms would be often develop without the removal of broncholiths. But, some cases of these are studded tightly to bronchial mucosa granulation tissue and obstructed completely, it is not easy to remove the entire material by bronchoscopy without major complications. The therapeutic options to remove broncholiths are so variable, and it should be determined by mass size, mobility, location and patient's symptoms.
In general, a symptomatic, large and fixed broncholith were likely to be removed by a rigid bronchoscopy or if unsuccessful, thoracotomy. Success rates using flexible bronchoscopy for the removal of broncholiths reported to be approximately 30%3,4.
Rigid bronchoscopy is also employed for the removal of broncholiths with success rates ranging from 67 to 87%5. Olson et al.4 reported that 100% of their patients with loose (free in the airway) broncholiths were underwent flexible and rigid bronchoscopic extraction to attempts without severe complications. But, these results are only explained in easy cases resulting from loose broncholiths.
In many cases, a rigid bronchoscopy is preferred than a flexible bronchoscopy. Because, once the rigid bronchoscope was performed, jet ventilation is established that enabling the inspector more room to work through the end of the scope concomitantly while still oxygenating the patient6. But, rigid bronchoscopy needs general endotracheal anesthesia which sometimes induce respiratory depression or hemodynamic instability.
Therefore, many pulmonologist have been trying various ways to remove broncholiths by a flexible bronchoscopy. However as yet, there is no consistent guidelines for broncholithectomy or broncholithotomy using flexible bronchoscopy. As pulling with the forceps, or using a balloon catheters3, and YAG laser incision to broncholithotomy7, a variety of methods have been performed. Moreover, surgical treatment should be considered over bronchoscopic removal when patients present with hemoptysis, the broncholith is firmly attached to the bronchial wall, or bronchoscopic excision is not available or feasible6. Preferred operative procedures include segmentectomy, lobectomy, and pneumonectomy.
In both cases mentioned above, we used a flexible bronchoscopy guided cryoadhesion to remove the broncholiths which were firmly attached to the bronchial wall.
In the first case, the patient presented with obstructive pneumopathy caused by a fixed broncholith. Bronchoscopy was performed to identify the broncholith and the tip of cryoprobe was attached to the mass to freeze and it was removed with pull-out method. The procedure was successfully performed despite minor bleeding that was controlled by APC.
In the second case, the patient complained of massive recurrent hemoptysis that was revealed to be caused by a fixed broncholith. The same procedure was performed untill cryoprobe attached to the mass to freeze but then pulling out was risky as it may concur massive bleeding. This time, pulling out was retained until repeated freezing and thawing eased separation of broncholith and bronchial mucosa without any exertion. Bleeding was minimal.
Bronchoscopic cryotherapy is most often employed as a palliative therapy for airway obstruction due to a malignancy, usually in patients who cannot tolerate lung resection due to poor respiratory function or who are deemed inoperable due to the proximity of the tumor to the carina. Cryoadhesion can be used to extract foreign bodies, mucous plugs, or blood clots. During cryoadhesion, the cryoprobe freezes the target material, causing the material to adhere to the probe8-10. In 2007, there was a first attempt to remove the broncholith by using a cryoprobe with flexible bronchoscopy11.
A conventional method to remove broncholiths is to pull them out with a forcep. This method is applicable when the broncholith is not firmly attached to the bronchial wall. When dealing with the fixed masses however, which is the subject of this study, it is unlikely to remove them with forcep as it may tear the tissue surrounding which may result in major bleeding while pulling them out.
Another method applicable to remove broncholiths is to grind them with YAG laser7. Having to be performed in a very narrow space, it could also inflict damages on the surrounding tissue and entail subsequent bleeding. In particular, if the mass is adjacent to the vessel, it can trigger massive life-threatening hemoptysis secondary to fistula or rupture of aorta or pulmonary arteries and systemic air embolism12.
Meanwhile, cryoadhesion does not inflict any direct damages on the bronchial wall. While it freezes broncholith, the cold stimuli is gradually transmitted from the objective to the surrounding tissue. Tissue affected by cold stimuli will lose its density making it easier for the mass to fall apart13,14. All the procedures can take place without making the patient unconcious. Cryoadhesion obviously provides us with safer method to remove broncholith and foreign body in a limited space14.
There are two ways to perform the cryoadhesion depending on the conditions of the patients: pull-out method and repeated thawing-freezing method14,15.
Pull-out method means to forcep it out after rapid freezing of the broncholith. It has the merit of removing the broncholith with a single attempt but in such a case where surrounding tissue is not fully loosened, it could inflict damages on the tissue causing subsequent complications14. It is therefore applicable only to not firmly attached, movable endobronchial lesion or foreign body.
Repeated thawing-freezing method is suggested when the broncholith is deemed not easily removable by the pull-out method. The repeated thawing and freezing of the objective will reduce the resistance of the surrounding tissue ensuring safer removal of the fixed mass. Repeated thawing-freezing method obviously is more time consuming than pull-out method. Pull-out method as part of the cryoadhesion has greater risk of bleeding than repeated thawing-freezing method in which only a small amount of bleeding is noticed when removing the broncholith14. Repeated thawing-freezing method is recommendable to the patients with high risk of complications.
Our cases report successful removal of broncholith with cryoadhesion on patient of semi-sedative state. The procedure introduces safer method of repeated freezing and thawing that loosens the connection between the soft tissue and the broncholith unlike the classical way of attaching and pulling out. In this way, bleeding risk is notably reduced and manipulation much easier in small spaces and thus flexible bronchoscopy guided cryoadhesion can be considered as a primary therapy for removal of broncholith whether movable or fixed even though the patien's main symptom is hemoptysis.
Thus, introduction of bronchoscopic cryoadhesion method can spare unnecessary general anesthesia or lung surgery.
Figures and Tables
Figure 1
A 32-year-old woman's computed tomography (CT) scan image. (A) Chest CT scan image (mediastinal setting) showing calcifications present within the right upper lobe bronchus and resulting pneumonia. (B) Follow-up CT scan image (mediastinal setting) after bronchoscopic broncholith removal showing a patent airway and recovered pneumonic infiltrations.

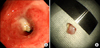
Figure 2
A 32-year-old woman's bronchoscopy image and extracted broncholiths. (A) The bronchoscopic view showing the sharp marginated broncholith which attached at the opening of the right upper lobe bronchus. (B) The extracted broncholith which was about 1.8 cm sized.
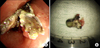
Figure 3
A 32-year-old man's computed tomography (CT) scan image. (A) Chest CT scan image (mediastinal setting) showing patchy opacities surrounding lingular segment and a calcified density within left upper lobe bronchus suggesting broncholith with pulmonary hemorrhage. (B) Follow-up CT scan image (mediastinal setting) after bronchoscopic broncholith removal showing no endobronchial mass.

References
1. Kwak SM, Ahn CM, Kim HJ, Lee JS, Oh SH. A case of middle lobe syndrome due to broncholithiasis. Korean J Intern Med. 1988. 34:834–840.
2. Lee HL, Kim SK, Chang J, Kim SK, Lee WY, Chung KY. A study on broncholithiasis. Korean J Med. 1995. 48:353–361.
3. Yi KY, Lee HK, Park SJ, Lee YC, Rhee YK, Lee HB. Two cases of broncholith removal under the guidance of flexible bronchoscopy. Korean J Intern Med. 2005. 20:90–91.
4. Olson EJ, Utz JP, Prakash UB. Therapeutic bronchoscopy in broncholithiasis. Am J Respir Crit Care Med. 1999. 160:766–770.
5. Ferguson JS, Rippentrop JM, Fallon B, Ross AF, McLennan G. Management of obstructing pulmonary broncholithiasis with three-dimensional imaging and holmium laser lithotripsy. Chest. 2006. 130:909–912.
6. Cerfolio RJ, Bryant AS, Maniscalco L. Rigid bronchoscopy and surgical resection for broncholithiasis and calcified mediastinal lymph nodes. J Thorac Cardiovasc Surg. 2008. 136:186–190.
7. Miks VM, Kvale PA, Riddle JM, Lewis JW Jr. Broncholith removal using the YAG laser. Chest. 1986. 90:295–297.
8. Bolliger CT, Mathur PN, Beamis JF, Becker HD, Cavaliere S, Colt H, et al. ERS/ATS statement on interventional pulmonology. European Respiratory Society/American Thoracic Society. Eur Respir J. 2002. 19:356–373.
9. Ernst A, Feller-Kopman D, Becker HD, Mehta AC. Central airway obstruction. Am J Respir Crit Care Med. 2004. 169:1278–1297.
10. Asimakopoulos G, Beeson J, Evans J, Maiwand MO. Cryosurgery for malignant endobronchial tumors: analysis of outcome. Chest. 2005. 127:2007–2014.
11. Reddy AJ, Govert JA, Sporn TA, Wahidi MM. Broncholith removal using cryotherapy during flexible bronchoscopy: a case report. Chest. 2007. 132:1661–1663.
12. Tellides G, Ugurlu BS, Kim RW, Hammond GL. Pathogenesis of systemic air embolism during bronchoscopic Nd:YAG laser operations. Ann Thorac Surg. 1998. 65:930–934.
13. Kim HO, Kim SJ, Lee SH, Lee EJ, Hur GY, Lee SY, et al. A case of atypical bronchial carcinoid treated by cryotherapy. Tuberc Respir Dis. 2011. 70:521–525.
14. Lyu J, Song JW, Hong SB, Oh YM, Shim TS, Lim CM, et al. Bronchoscopic cryotherapy in patients with central airway obstruction. Tuberc Respir Dis. 2010. 68:6–9.
15. Jung JY, Lee SY, Kim DH, Lee KJ, Lee EJ, Kang EH, et al. Clinical benefits and complications of cryotherapy in advanced lung cancer with central airway obstruction. Tuberc Respir Dis. 2008. 64:272–277.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download