Abstract
Background
The prevalence rate of pulmonary tuberculosis (PTB) is steadily decreasing in South Korea. However, PTB is a disease with relatively high mortality and morbidity rates throughout Korea. Although there are many studies and statistics about the risk factors of PTB mortality in many countries, there are only a limited number of domestic papers on this topic. The aim of this study is to determine predictive factors for mortality among in-hospital patients associated with PTB.
Methods
From December 2006 to January 2011, we reviewed medical records of 2,122 adult patients diagnosed with tuberculosis at a single tertiary hospital in a suburban area. In this study period, 960 patients were diagnosed with PTB by positive Acid fast bacilli smear and/or mycobacterial culture of the respiratory specimen. We compared the groups of patients deceased and patients discharged alive with PTB. The number of dead patients was 82 (47 males, 35 females).
Results
Mortality was significantly associated with increased values of white blood cells (WBC), blood urine nitrogen (BUN), creatinine, C-reactive protein (CRP), numbers of involved lung field, and length of hospitalization. Also, it was associated with the decreased values of hemoglobin, lymphocyte, sodium, albumin, and cholesterol. Furthermore, admission through the emergency department, initial intensive care unit admission, and drug resistant PTB affected mortality in PTB patients. Independent predictors associated with PTB mortality are BUN, initial intensive care unit care, and admission during treatment of tuberculosis.
According to World Health Organization (WHO), incidence of tuberculosis (TB) in 2009 was 9.4 million worldwide, and number of TB patients and deaths was 14 million and 1.3 million, respectively1. In Korea, incidence of TB has steadily decreased; statistics of Korean government shows that TB death rate ranks outside top 10 in Korea2. Despite, pulmonary tuberculosis (PTB) still shows high morbidity and infection rates among infectious diseases.
PTB does not usually require hospital admission for treatments, but if symptoms such as shortness of breath, and deterioration in systemic condition are present, hospital admission may be necessary. Despite of appropriate TB treatments, death rate of TB reaches 5 to a population of 100,0003. Many patients die prior to or in the middle of treatments4. Causes of death include TB itself and underlying diseases and diseases in organs other than the lung5. In cases of respiratory infection diseases including pneumonia, indexes such as Pneumonia Patient Outcomes Research Team (PORT)6 and confusion, uremia, respiratory rate, blood pressure (CURB)7 help calculate a death rate using conditions of patients at admission and blood test findings. However, studies and data on prognosis factors of PTB have not been sufficient enough in Korea. Therefore, it may be meaningful to confirm death-related factors for treatments and deciding prognosis.
In this study, patient records of the university hospital inpatients accompanied by PTB were investigated to find out characteristics of the patients and factors affecting death.
We reviewed medical records of 2,340 patients who visited tertiary teaching university hospital, Yonsei University Wonju Christian Hospital, between December 2006 and January 2011, and were diagnosed with TB by International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10). Patients with younger than 20 years of age, negative sputum examination results, extra PTB only, nontuberculous mycobacteria and who did not receive TB tests were excluded from the present study. Among 1,021 patients who were diagnosed with PTB, those who were diagnosed through biopsy only were excluded from the present study, and the remaining 960 inpatients diagnosed with PTB through acid fast bacillus (AFB) smear test and mycobacterium culture test were finally selected. Among patients who were admitted to hospital during treatments, or diagnosed with PTB after admission, a total of 82 patients died; 67 died during hospital stay while 15 died during drug treatment after they were discharged (Figure 1). Control group was selected 187 patients by matching age and gender among who were diagnosed with PTB through sputum examination, and were discharged alive from the hospital.
Through retrospective investigations on patient records, major symptoms at admission, comorbidity, cause of death, and results of blood test, radiologic findings and tests related with TB were confirmed.
Through patient records, major symptoms, comorbidity, use of emergency room or intensive care unit (ICU) at admission, and hospital stay were reviewed.
Test results including white blood cell (WBC) count, hemoglobin, lymphocyte count, sodium, potassium, blood urea nitrogen, creatinine, albumin, total cholesterol, blood glucose, aspartate transaminase (AST), alanine transaminase, bilirubin, C-reactive protein (CRP) and arterial blood gas were reviewed.
In sputum samples, results of AFB smear test, culture test and drug susceptibility test were reviewed. Patients showing at least one positive result of either smear test or culture test were enrolled in the present study. Cases identified with nontuberculous mycobacteria in culture test were excluded.
Regarding classification of severity according to the extent of lesion in the lung, standards of National Tuberculosis Association, US8, and method of dividing both lungs into 6 random parts were used based on the chest X-ray images at admission. According to the standard of National Tuberculosis Association, US, mild level is the case of lesions localized in small area at one lung or both lungs without cavity, while intermediate level is the case of slightly scattered lesions not exceeding one lung, dense lesions taking less than 1/3 of one lung, or the sum of cavity diameter which is less than 4 cm. Severe level is the case of lesions whose severity is exceeding intermediate level. According to the method of dividing both lungs into 6 random parts, both lungs were divided into upper, middle and lower parts on chest X-ray prior to counting numbers of involved part.
Patients who died during hospital stay, or died within 2 weeks after being discharged were included as the case of death during hospital stay.
Criteria of direct cause of death by TB include: central nervous system invasion with positive culture test result, deterioration of PTB accompanied by findings of negative nitrogen balance without respiratory failure, identification of drug-resistant strains without other cause of death, large amount of hemoptysis on the brink of death, and respiratory failure without any other etiology of respiratory failure2. Cause of death was divided two groups into TB-related and non-TB-related cases.
Drug-resistant strains include: strains resistant to isoniazid or rifampin, multidrug-resistant TB strains resistant to both isoniazid and rifampin, and extensive drug-resistant TB strains resistant to isoniazid and rifampin, and to at least one quinolones and one of 3 injections.
SPSS version 18 (IBM Corp., Armonk, NY, USA) was used for statistical analysis. Values of continuous variables were shown as mean±SD, and discrete random variables were shown as frequency or percentage. For comparison of continuous variables between death group and control group, t-test was used. For discrete random variables, chi-square test was used. In case of small number of comparison groups, Fisher's exact test was used. Multiple logistic regression test was conducted for statistically significant or influential items. Statistical significance was set with p-value at less than 0.05.
Decedent group consisted of 82 subjects with a mean age of 68.8±15.3. Number of male was 47 (57.3%). Significant difference between the groups was observed in terms of admission via emergency room and ICU, long hospital stay, present TB treatments at the time of admission, and history of interrupting treatments (p <0.05) (Table 1).
Major symptoms of subjects at the time of admission included coughing, dyspnea, sputum, fever, hemoptysis and general weakness. In decedent group, dyspnea (43.9%) was most common symptom followed by general weakness (18.3%). In survivor group, coughing (49.7%) was most common symptom followed by dyspnea (35.3%) and sputum (34.8%). Among major symptoms, significant difference in general weakness, poor oral intake and mental deterioration was observed between the groups (p<0.05) (Table 2). One hundred ninety-four patients were admitted due to the respiratory symptoms such as coughing, sputum, fever, dyspnea and hemoptysis, and 9 patients were admitted due to side effects developed during TB treatments, and 6 patients were admitted for evaluation of TB. Reasons of the remaining subjects included systemic deterioration, digestive symptoms such as bloody stool and nausea, cardiovascular symptoms such as chest pain and palpitation, and neurologic symptoms such as mental deterioration.
Number of patients having comorbidity was 60 (73.2%) in decedent group, and 118 (63.1%) in survivor group showing no significant difference between the groups. In both group, most common comorbidity was hypertension, followed by diabetes, history of PTB, respiratory diseases, cerebrovascular diseases, malignant tumor, cardiovascular diseases, chronic hepatitis, and kidney diseases. Except kidney diseases and malignant tumor, no difference of comorbidity showed between the groups (p<0.05) (Table 3).
According to microbiological comparison, positive AFB smear test results were observed in 69 (84.1%) subjects in decedent group, and 69.5% in survivor group showing a significant difference (p=0.012). Presence of drug-resistant strains was reported in 16 (19.5%) subjects in decedent group, and 11.8% in survivor group showing a significant difference (p=0.046). However, when drug-resistant strains against each agent were compared, no statistical significance was observed between the groups. According to radiologic findings, number of invaded lung part was 3.3±1.6 in decedent group, and 2.1±1.0 in survivor group showing a significant difference (p<0.05). Based on chest X-ray, severe level showed the most statistical significance than other milder levels. However, presence of cavity was not statistically significant (Table 4).
According to the results of blood test at admission, levels of WBC, blood urea nitrogen, creatinine and CRP were significantly high in decedent group, while levels of hemoglobin, lymphocyte count, sodium, albumin and total cholesterol were significantly low (p<0.05) (Table 5).
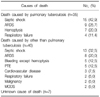
In all subjects, septic shock was the most common cause of death with 28 (34.1%) subjects followed by acute respiratory distress syndrome (ARDS) with 17 (20.7%) subjects. PTB was the direct cause of death with 35 (42.7%) subjects and among these patients, septic shock with 15 (42.9%) subjects, ARDS with 9 (25.7%) subjects, hemoptysis with 7 (20.0%) subjects, and respiratory failure with 4 (11.4%) subjects. In the group whose direct cause of death was not PTB, septic shock (13 subjects, 32.5%) was the most common cause, and the reason was mainly due to pneumonia (12 subjects, 92.3%). Other causes of death included bleeding other than hemoptysis (12.5%) and pulmonary embolism (12.5%). Deaths due to hemoptysis were observed only in the patients whose direct cause of death was TB (Table 6).
As a result of multiple logistic regression test for the items showing a significant difference through univariate analysis, factors such as blood urea nitrogen, initial treatments in ICU, admission during TB treatments were confirmed as the factors independently affecting death (Table 7).
According to the statistics of Korean National Tuberculosis Association, incidence of TB in 2010 was 36,305 in every 100,000 population3. Out of the 36,305 patients, 28,176 were PTB patients, and we estimate additional patients who may have not been diagnosed or reported. Death rate in every 100,000 population was 4.8 showing a reduction from 7.2 in 2000. Accordingly, the death rate of PTB ranks outside top 10 in Korea for the last 4 years. Out of the 1,021 TB inpatietns in the present study, 960 subjects were diagnosed with PTB based on microbiological tests. Among them, 67 patients died during hospital stay, and death rate was about 6.9%. This result is very higher than the result of Korean National Tuberculosis Association in 2010, which was 4.8 in a population of 100,000. This study was conducted in inpatients of tertiary hospital with a high ratio of severe cases resulting in a higher death rate than that of Korean National Tuberculosis Association.
In the study conducted in North Carolina, US, Nguyen et al.9 reported 721 (13.5%) death cases out of 5,311 TB patients over the period of 10 years (1993~2003). According to the study, risk factors of TB death included old age, miliary or meningeal diseases and human immunodeficiency virus (HIV). In the study conducted in San Francisco, California, US, Nahid et al.10, reported 37 (6.6%) death cases out of 565 patients between 1990 and 2001, and factors of death such as HIV infection, old age, positive sputum exam result, and poor TB treatments. According to the study by Low et al.11 conducted in 7,433 patients in Singapore between 2000 and 2006, 884 (11.9%) patients died. Risk factors included old age, male, Malayan, microbiological definite diagnosis, history of using long-term care facilities, and strains having resistance against at least isoniazid. Lefebvre and Falzon12 reported 3,085 (7.8%) cases of death out of 39,566 patients in 15 EU countries between 2002 and 2004. Risk factors of death included old age and resistance against isoniazid and rifampin in addition to male and history of TB treatments. In Africa, more studies on HIV have been reported than studies on risk factors associated with TB13,14. Few studies have been reported on risk factors of TB death in Korea. Shin et al.15 reported 27 death cases with 54 control group patients in 2006. In the study, significant difference was confirmed in comorbidity, admission via emergency room, initial ICU treatments, dyspnea at admission, general weakness, miliary TB, hemoglobin, blood urea nitrogen, albumin, cholesterol, AST and CRP. Among these, initial ICU treatments and albumin were confirmed as independent factors. In the areas other than Africa, old age, HIV, gender and isoniazid drug-resistant strains were risk factors. Since age and gender were analyzed in pair in Korean studies including the present study, age and gender were excluded from risk factors. But, number of death patients showed an increase in elderly patients in the age of 60 or older (Figure 2) evidencing an old age as a factor associated with death. Presence of drug-resistant strains had a statistical significance between two groups, but when drug-resistant strains were compared according to each agent, no significant finding was observed. Due to small numbers of drug-resistant strains, it was not easy to confirm significance. Tests on HIV were not conducted and accordingly, its possibility as a risk factor was not confirmed. However, considering increasing number of HIV patients, studies on HIV will be necessary as Shin et al.15 suggested.
As a result of comparing risk factors of the present study with those of Korean studies, many factors stated in the studies are common. Factors such as admission via emergency room, initial ICU treatments, general weakness, blood urea nitrogen, CRP, hemoglobin, albumin and total cholesterol were significant in two studies. However, in multivariate analysis, initial ICU treatment was the only common independent factor associated with death. Only one factor was common as an independent factor, but through univariate analysis, factors such as systemic condition of patients at admission, nutritional state and intensive care were confirmed to affect prognosis. This result corresponds to that of Rao et al.16, which reported that death factors were decided not only by severity and chronic condition of TB but systemic health state of patients.
In this study, patients complained coughing and dyspnea as most common symptoms, but decedent group did significantly not cough, and patients with general weakness, poor oral intake and mental deterioration showed a statistically significant difference between the groups. As comorbidity, respiratory diseases such as history of PTB or chronic obstructive pulmonary disease, diffuse interstitial lung disease and asthma did not show significant difference between the groups. Only kidney diseases including end stage renal disease showed a significant difference but the number of sample was too small to confirm.
In microbiological statistics, Low et al.11 and Lefebvre and Falzon12 reported that presence of drug-resistant strains was significant, particularly in multidrug-resistant strains. In the present study, positive result of smear test, and presence of drug-resistant strains were significant between the groups, but when each type of drug-resistant strains was compared, no statistical significance was observed. In addition, due to the small number of samples, statistical significance on drug-resistant strains was not confirmed.
Through radiologic image divided 6 parts, number of involved parts in decedent group were significantly more than control group, and the statistical significance was also confirmed in 3 sub-divided severity levels according to the standards of National Tuberculosis Association, US. However, severity level in multivariate test was not recognized as an independent factor by chest X-ray.
Increase in WBC count and CRP at admission showed a significant difference between the groups, this is implying an influence of inflammatory responses at admission on death. Recently Rasmussen et al.17 reported that procalcitonin could help anticipate severity and death in TB patients. Therefore, correlation with inflammation markers such as procalcitonin may be necessary to study in future.
Plasma protein which helps assess nutritional status includes albumin, prealbumin, transferrin and ferritin18. According to Goldwasser and Feldman19, the lower the level of albumin was, the higher the death rate was. In the present study, the albumin level of death group was significantly lower than that of survivor group, but it was not confirmed as an independent factor. For detailed investigation on nutritional status, body mass index should be checked together.
Out of the 82 death patients, causes of death of 7 patients were not confirmed due to loss of contact with their family in some cases of moribund discharge, while 35 (42.7%) patients were confirmed that their PTB was directly associated with death. The most common factor was septic shock, but hemoptysis (7 subjects, 20.0%) showed a significant difference from decedent group which did not die of PTB. According to Davis et al.5, only 20 (49%) out of 41 death patients died of TB, and number of deaths due to hemoptysis was 4 (20%) showing a similar result to the present study.
According to the present study and Shin et al.15, the only common independent factor in multivariate analysis was initial ICU treatment. Zahar et al.20 reported that cases with delay in diagnosis and treatments of TB, and active PTB in severe level which requires mechanical ventilation show high death rate. In addition, delay in TB treatments for patients in ICU with respiratory failure results in a high death rate. In Korea, Kang et al.21 reported 12 death cases out of 43 PTB patients admitted in ICU. In univariate analysis, significant items were major symptoms such as coughing, number of invaded parts of the lung, lymphocyte count, albumin, cholesterol and CRP. In multiple regression analysis, respiratory failure was the independent factor affecting death. In the present study, 47 patients were admitted via ICU, and 31 died. In future, study on causes of death in ICU will be necessary.
In the present study, among patients accompanied TB, we can find factors which correlated with death, but there are limitations. First, age and gender were paired in selecting subjects of survivor group, but number of elderly patients may be too small for analysis. In addition, results on factors such as drug-resistant strains may be distorted due to the small sample size. Second, there is a limitation using past patient records. Third, cases of PT which were accidentally found during hospital stay could be so mild that it might not be directly associated with death. Fourth, in some cases of moribund discharge, patient records and contact information were not sufficient for confirming cause of death.
In treatments of PTB, delayed treatments may increase risk of death. So, stabilization of systemic condition, early diagnosis and appropriate treatments may contribute to lowering TB death rate. Data of the present study may contribute to making prognosis of TB patients, and may be used for future TB studies.
Figures and Tables
References
1. World Health Organization. Report: global tuberculosis control. 2010. Geneva: World Health Organization.
2. Statistics Korea [Internet]. c1996. cited 2011 Nov 17. Daejeon: Statistics Korea;Available from: http://kostat.go.kr/.
3. Korean National Tuberculosis Association [Internet]. cited 2011 Nov 17. Seoul: Korean National Tuberculosis Association;Available from: http://www.knta.or.kr/.
4. Harries AD, Hargreaves NJ, Gausi F, Kwanjana JH, Salaniponi FM. High early death rate in tuberculosis patients in Malawi. Int J Tuberc Lung Dis. 2001. 5:1000–1005.
5. Davis CE Jr, Carpenter JL, McAllister CK, Matthews J, Bush BA, Ognibene AJ. Tuberculosis. Cause of death in antibiotic era. Chest. 1985. 88:726–729.
6. Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997. 336:243–250.
7. Lim WS, Macfarlane JT, Boswell TC, Harrison TG, Rose D, Leinonen M, et al. Study of community acquired pneumonia aetiology (SCAPA) in adults admitted to hospital: implications for management guidelines. Thorax. 2001. 56:296–301.
8. Hong YP. Hong YP, Kim SJ, editors. Chapter 13. Clinical diagnostic classification. Tuberculosis. 1993. 4th ed. Seoul: The Korean Academy of Tuberculosis and Respiratory Diseases;142–143.
9. Nguyen LT, Hamilton CD, Xia Q, Stout JE. Mortality before or during treatment among tuberculosis patients in North Carolina, 1993-2003. Int J Tuberc Lung Dis. 2011. 15:257–262.
10. Nahid P, Jarlsberg LG, Rudoy I, de Jong BC, Unger A, Kawamura LM, et al. Factors associated with mortality in patients with drug-susceptible pulmonary tuberculosis. BMC Infect Dis. 2011. 11:1.
11. Low S, Ang LW, Cutter J, James L, Chee CB, Wang YT, et al. Mortality among tuberculosis patients on treatment in Singapore. Int J Tuberc Lung Dis. 2009. 13:328–334.
12. Lefebvre N, Falzon D. Risk factors for death among tuberculosis cases: analysis of European surveillance data. Eur Respir J. 2008. 31:1256–1260.
13. Meintjes G, Schoeman H, Morroni C, Wilson D, Maartens G. Patient and provider delay in tuberculosis suspects from communities with a high HIV prevalence in South Africa: a cross-sectional study. BMC Infect Dis. 2008. 8:72.
14. Mukadi YD, Maher D, Harries A. Tuberculosis case fatality rates in high HIV prevalence populations in sub-Saharan Africa. AIDS. 2001. 15:143–152.
15. Shin SR, Kim CH, Kim SE, Park YB, Lee JY, Mo EK, et al. Predictors on in-hospital mortality following in-hospital diagnosis of tuberculosis. Tuberc Respir Dis. 2006. 61:233–238.
16. Rao VK, Iademarco EP, Fraser VJ, Kollef MH. The impact of comorbidity on mortality following in-hospital diagnosis of tuberculosis. Chest. 1998. 114:1244–1252.
17. Rasmussen TA, Søgaard OS, Camara C, Andersen PL, Wejse C. Serum procalcitonin in pulmonary tuberculosis. Int J Tuberc Lung Dis. 2011. 15:251–256.
18. DeLegge MH, Drake LM. Nutritional assessment. Gastroenterol Clin North Am. 2007. 36:1–22.
19. Goldwasser P, Feldman J. Association of serum albumin and mortality risk. J Clin Epidemiol. 1997. 50:693–703.
20. Zahar JR, Azoulay E, Klement E, De Lassence A, Lucet JC, Regnier B, et al. Delayed treatment contributes to mortality in ICU patients with severe active pulmonary tuberculosis and acute respiratory failure. Intensive Care Med. 2001. 27:513–520.
21. Kang JY, Kim MS, Kim JS, Kang HH, Kim SS, Kim YH, et al. Clinical characteristics and prognostic factors in patients with pulmonary tuberculosis admitted to intensive care units. Tuberc Respir Dis. 2010. 68:259–266.




 PDF
PDF ePub
ePub Citation
Citation Print
Print










 XML Download
XML Download