Abstract
Yellow nail syndrome (YNS) is a rare disorder of unknown cause associated with yellow nails, lymphedema and respiratory manifestations. It was first described by Samman and White in 1964, and to date, approximately 150 cases have been reported. The diagnosis of YNS is essentially a clinical one and based on the presence of characteristic findings. We report a case of YNS of a 62-year-old female who presented with a 4-month history of dyspnea and recurrent pleural effusion. The patient had a 5-year history of leg swelling and dyspnea. She had been managed with medications for congestive heart failure (CHF) for two years and she was referred to our hospital for further evaluation and management.
Yellow nail syndrome (YNS) is a rare disorder characterized by yellow discoloration of nails, lymphedema and respiratory disorders1-3. It was first described by Samman and White in 1964, and to date, approximately 150 cases have been reported1. Three cases have been reported in Korea. The underlying pathophysiology, clinical presentation, and natural history remain obscure. According to available data, anatomic or functional lymphatic abnormalities have been proposed as the predominant underlying mechanism1,4,5. Recent studies have suggested microvasculopathy with protein leakage as a more likely explanation for various manifestations of YNS6,7. Many cases are sporadic with clinical manifestations and occur relatively late. Overall, lymphatic dysfunction observed in YNS is an acquired disorder rather than a hereditary one8. Our case, which have been managed with the medication for CHF, was diagnosed as YNS.
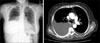
We report a case of a 62-year-old female who presented with a 4-month history of dyspnea and recurrent pleural effusion. The patient also had a 5-year history of leg swelling and dyspnea. She had been treated with medications for CHF two years ago. But her symptoms had been waxing and waning. Four months prior to presentation, she had been hospitalized and undergone thoracentesis for dyspnea. Echocardiography at that time was unremarkable. She had been managed with digoxin, carvedilol, diuretics (furosemide, spironolactone) but continued to experience dyspnea, generalized edema. She was referred to our hospital for further evaluation and management. On admission, the blood pressure was 136/65 mm Hg, heart rate 84/min, respiratory rate 20/min, and body temperature 36.0℃. On physical examination, breathing sound and vocal fremitus were decreased and on percussion, dullness was felt on right lung field. Thickened yellowish nails with onycholysis features were evident (Figure 1). Complete cell count test, liver function test and urine analysis were normal. Erythrocyte sedimentation rate was 57 mm/h and NT-pro BNP was 108.8 pg/mL. Chest radiograph and Computed tomography revealed right pleural effusion without parenchymal disorder (Figure 2). Pleural fluid analysis showed lymphocyte-predominant exudate (66%). Adenosine deaminase (ADA) was 33.4 IU/L, cytology showed no malignant cells, and Tb polymerase chain reaction (PCR) was negative. Bronchoscopic findings included external compression of RLL and RML due to massive pleural effusion. An obstructive pattern was observed on pulmonary function test. On echocardiography, the ventricular function was normal, except for a small amount of pericardial effusion. Video-assisted thoracic surgery (VATS) biopsy exhibited inflamed pleura with focal myxoid degeneration. Lymphoscintigraphy was performed to confirm the diagnosis of YNS, and delayed main lymphatic flow of both lower extremities, highly suggestive of lymphedema, was seen. There were no associated conditions, such as malignancies, immunodeficiency states, and connective tissue diseases. The triad of YNS, which are thickened yellow nails, lymphedema and chronic respiratory manifestation, were met in this case. The patient is currently being treated with supportive measures including repeated therapeutic thoracentesis and chemical pleurodesis for pleural effusion, as well as elastic stockings for lower extremity edema. Presently, she has been doing well for one year after diagnosis.
Yellow nail syndrome (YNS) was a rare disorder characterized by yellow nails, lymphedema and respiratory manifestations1-3. The characteristics of the nails include yellow discoloration, slow growth, abnormal thickening, transverse ridging, excessive curvature, and onycholysis. Lymphedema is slow progressive, nonpitting and typically involves the lower extremities in a symmetric fashion. Respiratory manifestations are diverse, and includes cough, shortness of breath, pleural effusion, bronchiectasis, chronic sinusitis, and recurrent pneumonia. Pericardial effusions may also occur8.
Although the pathophysiology, clinical presentation, and natural history remain obscure, anatomic or functional lymphatic abnormalities have been proposed as the predominant underlying mechanism1,4,5. Recent studies have suggested microvasculopathy with protein leakage as a more likely explanation for various manifestations of YNS6,7. Many cases are sporadic with clinical manifestations and occur relatively late. Overall, lymphatic dysfunction observed in YNS is an acquired disorder rather than a hereditary one8.
Multiple clinical conditions have been associated with YNS, which include malignancies, immunodeficiency states, connective tissue diseases, diabetes mellitus, thyroid dysfunction, hemochromatosis, obstructive sleep apnea, Guillain-Barré syndrome, xanthogranulomatous pyelonephritis, tuberculosis, myocardial infarction, nephrotic syndrome, exudative enteropathy, hypoalbuminemia, drugs9.
The diagnosis of YNS is essentially a clinical one and based on the presence of characteristic findings including thickened yellow nails, lymphedema and chronic respiratory manifestation. All three criteria may not simultaneously be present, and the presence of two of them has been considered sufficient for diagnosis2.
Most clinical manifestations of YNS are generally manageable with supportive measures. Bronchiectasis can be controlled with combination of bronchopulmonary hygiene measures, postural drainage and prompt treatment of complicating respiratory infections. The management strategies for recurrent symptomatic pleural effusion include therapeutic thoracenteses, pleurodesis and pleurectomy. Lymphedema can be managed with a combination of gradient pressure garments, exercise, bandage wraps, manual lymphedema drainage, and external pneumatic compression. Nail manifestations eventually improve in the majority of patients, often without intervention. Although the efficacy of local steroid injection or vitamin E remains unclear, it seems reasonable to contemplate the option10. Lymphedema and pleural effusions are persistent and spontaneous recovery has not been reported. Improvement of lymphedema and nail manifestations has been observed with better control of respiratory manifestations. The long-term prognosis appears favorable. The previous three cases in Korean journals showed that nail change was a mainly diagnostic clue. In this case report, we present a patient who had been initially managed for CHF was confirmed to have YNS.
Figures and Tables
References
1. Samman PD, White WF. The "yellow nail" syndrome. Br J Dermatol. 1964. 76:153–157.
2. Hiller E, Rosenow EC 3rd, Olsen AM. Pulmonary manifestations of the yellow nail syndrome. Chest. 1972. 61:452–458.
3. Emerson PA. Yellow nails, lymphoedema, and pleural effusions. Thorax. 1966. 21:247–253.
4. Beer DJ, Pereira W Jr, Snider GL. Pleural effusion associated with primary lymphedema: a perspective on the yellow nail syndrome. Am Rev Respir Dis. 1978. 117:595–599.
5. Bull RH, Fenton DA, Mortimer PS. Lymphatic function in the yellow nail syndrome. Br J Dermatol. 1996. 134:307–312.
6. Battaglia A, di Ricco G, Mariani G, Giuntini C. Pleural effusion and recurrent broncho-pneumonia with lymphedema, yellow nails and protein-losing enteropathy. Eur J Respir Dis. 1985. 66:65–69.
7. D'Alessandro A, Muzi G, Monaco A, Filiberto S, Barboni A, Abbritti G. Yellow nail syndrome: does protein leakage play a role? Eur Respir J. 2001. 17:149–152.
8. Maldonado F, Ryu JH. Yellow nail syndrome. Curr Opin Pulm Med. 2009. 15:371–375.
9. Maldonado F, Tazelaar HD, Wang CW, Ryu JH. Yellow nail syndrome: analysis of 41 consecutive patients. Chest. 2008. 134:375–381.
10. Szolnoky G, Lakatos B, Husz S, Dobozy A. Improvement in lymphatic function and partial resolution of nails after complex decongestive physiotherapy in yellow nail syndrome. Int J Dermatol. 2005. 44:501–503.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download