Abstract
Background
This study evaluated which CT findings could be used to predict the negative results of a sputum smear in patients with active pulmonary tuberculosis and multiple cavities.
Methods
Thirty-eight patients with active pulmonary tuberculosis and multiple cavities on CT were classified into 2 groups: smear-positive (n = 30) and -negative (n = 8). The CT findings were reviewed retrospectively. The maximum internal diameter of the largest cavity, the number of the cavities and lobes with cavities, and the characteristics of the associated findings such as consolidation, ground glass opacity, micronodules and nodule were accessed. The number of cavities above 20 mm in the maximum internal diameter and a necrotizing pneumonia-like pattern were also evaluated.
Result
The maximum internal diameter and number of cavities was 32.23 ± 17.66 mm and 15.50 ± 11.12 mm (p = 0.0042), and 5.53 ± 3.17 and 2.43 ± 1.13 (p = 0.0002) in the smear-positive and -negative group, respectively. Three or more cavities were observed at 76.7% and 12.5% in the smear-positive and -negative group, respectively (p < 0.005). There were 2.00 ± 1.34 and 0.25 ± 0.46 (p = 0.001), and 1.5 ± 1.50 and 0.38 ± 0.52 (p = 0.0016) lobes with consolidation and ground glass opacity in the smear-positive and -negative group, respectively. A necrotizing pneumonia-like pattern was observed in 43.3% of the smear-positive group only. The other findings were similar in both two groups. The sensitivity, specificity, positive and negative predictive value for the presence of at least a finding of consolidation, more than 3 cavities or the largest cavity > 20 mm in the maximum internal diameter were 100%, 62.5%, 90.9%, and 100%, respectively.
Figures and Tables
Figure 1
CT images of a 65-year-old man among the sputum smear-negative group A. CT scan at the level of left upper lobe apex shows a cavity (7 mm in maximum internal diameter) (arrows). B. CT scan at the level of right upper lobe shows a cavity (6 mm in maximum internal diameter) (arrows). The rest CT scans of this patient showed no evidence of consolidation or another cavity.

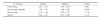
Table 2
Mean number of pulmonary lobes involving consolidation, ground-glass opacities, micronodules, and nodules in each group
References
1. Canetti G. Present aspects of bacterial resistance in tuberculosis. Am Rev Respir Dis. 1965. 92:687–703.
2. Kosaka N, Sakai T, Uematsu H, Kimura H, Hase M, Noguchi M, et al. Specific high-resolution computed tomography findings associated with sputum smear-positive pulmonary tuberculosis. J Comput Assist Tomogr. 2005. 29:801–804.
3. Shaw JB, Wynn-Williams N. Infectivity of pulmonary tuberculosis in relation to sputum status. Am Rev Tuberc. 1954. 69:724–732.
4. Liippo KK, Kulmala K, Tala EO. Focusing tuberculosis contact tracing by smear grading of index cases. Am Rev Respir Dis. 1993. 148:235–236.
5. Grzybowski S, Barnett GD, Styblo K. Contacts of cases of active pulmonary tuberculosis. Bull Int Union Tuberc. 1975. 50:90–106.
6. Van Geuns HA, Meijer J, Styblo K. Results of contact examination in Rotterdam, 1967-1969. Bull Int Union Tuberc. 1975. 50:107–121.
7. Telzak EE, Fazal BA, Pollard CL, Turett GS, Justman JE, Blum S. Factors influencing time to sputum conversion among patients with smear-positive pulmonary tuberculosis. Clin Infect Dis. 1997. 25:666–670.
8. American Thoracic Society. Diagnostic standards and classification of tuberculosis in adults and children. Am J Respir Crit Care Med. 2000. 161:1376–1395.
9. Matsuoka S, Uchiyama K, Shima H, Suzuki K, Shimura A, Sasaki Y, et al. Relationship between CT findings of pulmonary tuberculosis and the number of acid-fast bacilli on sputum smears. Clin Imaging. 2004. 28:119–123.
10. Lee KE, Lee YJ, Cho JH. Appropriate number of sputum specimens and optimal use of mycobacterial tests for the diagnosis of pulmonary tuberculosis. Korean J Clin Microbiol. 2005. 8:74–81.
11. Na MJ. Comparison of induced sputum and bronchoscopy in diagnosis of active pulmonary tuberculosis. Korean J Med. 1998. 55:75–82.
12. Baek SH, Lee JM, Kang MJ, Son JW, Lee SJ, Kim DG, et al. How reliable is sputum PCR test in the diagnosis of pulmonary tuberculosis when sputum smear is negative? Tuberc Respir Dis. 2001. 50:222–228.
13. Mo EK, Kyung TY, Kim DG, Park MJ, Lee MG, Hyun IG, et al. The clinical utility of polymerase chain reaction in the bronchoalveolar lavage fluid for the detection of mycobacteria. Tuberc Respir Dis. 1998. 45:519–528.
14. Poey C, Verhaegen F, Giron J, Lavayssiere J, Fajadet P, Duparc B. High resolution chest CT in tuberculosis: evolutive patterns and signs of activity. J Comput Assist Tomogr. 1997. 21:601–607.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download