Abstract
Obstructive Fibrinous Tracheal Pseudomenbrane (OFTP) is a rarely known but potentially fatal complication of endotracheal intubation. Sudden respiratory failure shortly after extubation is not infrequent in the ICU. However, these cases are commonly diagnosed as laryngospasm, retention of secretion or laryngeal edema. A 68-year-old woman presented with a 6-day history of progressive dyspnea. She had undergone invasive ventilator care for 24 hours. The patient was discharged from the hospital with improvement after having an extubation. However, after 3 days she revisited the emergency department with progressive dyspnea. The patient was diagnosed with OFTP from the results of chest CT and bronchoscopy. This is the first case studied in detail using CT images, pulmonary function test, and bronchoscopy.
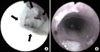
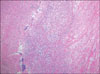
A 68-year-old woman with ischemic heart disease presented with a 6-day history of progressive dyspnea. Her symptoms had been progressively worsening for 6 days before the admission. On the first admission, her blood pressure was 130/70 mm Hg, and the pulse rate was 100/min. She was diagnosed with acute pulmonary edema, and she had undergone invasive ventilator care with a high volume-low pressure cuffed tube (Hi-Lo™; Mallinckrodt Medical, Athlone, Ireland) for 24 hours. While incubating, the intra-cuff pressure was monitored, and it was stable to maintain below 25 cm H2O. She improved, and the tube was removed immediately. She was discharged from the hospital on the 3rd day after extubation. After 3 days from being discharged, she revisited the emergency department with progressive dyspnea. On physical examination, breathing sound was coarse and stridor was ausculated on anterior neck. A chest CT scan was performed to search for an etiology of tracheal stenosis. The chest CT showed tubular structure mimicking stents at upper trachea (Figure 1). Pulmonary function test showed fixed airway obstruction (Figure 2). A bronchoscopy was performed under moderate sedation and showed a thick tubular, rubber-like, whitish pseudomembrane moulding, covering 2~3 cm of the tracheal wall at the level of the previously placed endotracheal tube cuff (Figure 2). It was completely ablated without secondary development of tracheal stenosis using a fiberoptic bronchoscope and forceps alone. After the mechanical removal of OFTP using a fiberoptic bronchoscope and forceps alone, following pulmonary function test showed no limitation of airway flow (Figure 3). A bronchoscopy was performed 1 month later, but showed no residual lesion. The biopsy specimen showed fibrinous material with acute inflammatory cells (Figure 4).
Obstructive fibrinous tracheal pseudomenbrane (OFTP) is a potentially fatal complication of tracheal intubation, consisted of fibrinous material with acute inflammatory cell infiltration and respiratory failure1,2 with unknown causes. OFTP typically appears as sudden upper airway obstruction occurring shortly after extubation. The clinical feature may be various from subclinical airway obstruction to acute respiratory failure. The delay from extubation to initial symptoms varies from several hours to several days1,2. So, it could be misled to the other causes of upper airway obstruction related to intubation such as acute retention of secretion, laryngospasm, glottic edema, and post-intubation tracheal stenosis. OFTP could sometimes be unrecognizable.
One possible cause of pathogenesis is a tracheal ischemic damage related to the cuff induced injury. According to the previous reports, the duration of intubation varies from 3 hours to 16 days. The delay from extubation to initial symptoms is anywhere between 3 hours to 9 days, and the delay from initial symptoms to diagnosis can be anywhere between <1 hour to 4 days1. Fiberoptic bronchoscopy is the key for diagnosis. The treatment choice is mechanical ablation with fiberoptic or rigid bronchoscopy1-4.
Unexplained respiratory failures with symptoms of upper airway obstruction, shortly after extubation, should lead to considering the diagnosis of OFTP. Learning points of this case are as following: 1) consider OFTP if unexplained respiratory failures occur shortly after extubation; 2) confirm the diagnosis of OFTP and ablate OFTP with bronchoscopy if OFTP is suspected.
Figures and Tables
Figure 1
Chest axial and coronal CT images are showing tubular structure with a good patency. It looks like a tracheal stents at upper trachea. CT: computed tomography.

Figure 2
(A) Fiberoptic bronchoscopy showing a thick tubular, rubber-like, whitish pseudomembrane moulding covering 2~3 cm of the tracheal wall at the level of the endotracheal cuff (the arrows indicate the pseudomembrane partially detached from trachea). (B) Fiberoptic bronchoscopy showing good patency after mechanical ablation with fiberoptic bronchoscopy.
References
1. Deslée G, Brichet A, Lebuffe G, Copin MC, Ramon P, Marquette CH. Obstructive fibrinous tracheal pseudomembrane. A potentially fatal complication of tracheal intubation. Am J Respir Crit Care Med. 2000. 162:1169–1171.
2. Lins M, Dobbeleir I, Germonpré P, Waelput W, Pauwels P, Jorens PG. Postextubation obstructive pseudomembranes: a case series and review of a rare complication after endotracheal intubation. Lung. 2011. 189:81–86.
3. Harbison J, Collins D, Lynch V, McNicholas WT. Acute stridor due to an upper tracheal membrane following endotracheal intubation. Eur Respir J. 1999. 14:1238.
4. Kang HH, Kim JW, Kang JY, Kim JS, Kim MS, Kim SS, et al. Obstructive fibrinous tracheal pseudomembrane after tracheal intubation: a case report. J Korean Med Sci. 2010. 25:1384–1386.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download