This article has been
cited by other articles in ScienceCentral.
Abstract
We report a case involving a young female patient with severe mandibular retrognathism accompanied by mandibular condylar deformity that was effectively treated with Le Fort I osteotomy and two genioplasty procedures. At 9 years and 9 months of age, she was diagnosed with Angle Class III malocclusion, a skeletal Class II jaw relationship, an anterior crossbite, congenital absence of some teeth, and a left-sided cleft lip and palate. Although the anterior crossbite and narrow maxillary arch were corrected by interceptive orthodontic treatment, severe mandibular hypogrowth resulted in unexpectedly severe mandibular retrognathism after growth completion. Moreover, bilateral condylar deformities were observed, and we suspected progressive condylar resorption (PCR). There was a high risk of further condylar resorption with mandibular advancement surgery; therefore, Le Fort I osteotomy with two genioplasty procedures was performed to achieve counterclockwise rotation of the mandible and avoid ingravescence of the condylar deformities. The total duration of active treatment was 42 months. The maxilla was impacted by 7.0 mm and 5.0 mm in the incisor and molar regions, respectively, while the pogonion was advanced by 18.0 mm. This significantly resolved both skeletal disharmony and malocclusion. Furthermore, the hyoid bone was advanced, the pharyngeal airway space was increased, and the morphology of the mandibular condyle was maintained. At the 30-month follow-up examination, the patient exhibited a satisfactory facial profile. The findings from our case suggest that severe mandibular retrognathism with condylar deformities can be effectively treated without surgical mandibular advancement, thus decreasing the risk of PCR.
Keywords: Severe mandibular retrognathism, Condylar deformity, Orthognathic surgery, Genioplasty
INTRODUCTION
In patients with mandibular retrognathism, it is difficult to establish a satisfactory esthetic profile,
12 improve the respiratory function,
34 and achieve stable treatment outcomes
25 with orthodontic treatment alone. Surgical mandibular advancement with bilateral sagittal split osteotomy (BSSO) or distraction osteogenesis (DO) is generally required for effective treatment,
6 and both osteotomy techniques have exhibited equal effectiveness and good outcomes.
7
However, progressive condylar resorption (PCR) sometimes occurs as a serious complication of surgical mandibular advancement.
8 Although the precise underlying mechanism remains unclear, overloading of the condyle during or after surgery is considered one of the main etiologies for PCR.
910 Moreover, Kobayashi et al.
11 reported that clicking in the temporomandibular joint (TMJ) and malformation of the condyles can be risk factors for PCR.
Here we report a case involving a young female patient with severe mandibular retrognathism and bilateral condylar deformities caused by severe mandibular hypogrowth after the first phase of orthodontic treatment. Bilateral PCR was suspected, and surgical mandibular advancement was associated with a high risk of further condylar resorption. Accordingly, we performed Le Fort I osteotomy with two genioplasty procedures, avoiding surgical mandibular advancement to prevent excessive loading of the condyles. Good esthetic and functional outcomes were achieved, with maintenance of a satisfactory facial profile at 30 months after treatment completion.
DIAGNOSIS AND ETIOLOGY
A girl aged 9 years and 9 months was referred to the outpatient clinic of our university hospital from the plastic surgery unit at another hospital. She had been diagnosed with left-sided unilateral cleft lip and palate (UCLP) and had undergone cheiloplasty at 4 months of age. Compared with the average height of Japanese girls of the same age (133.5 ± 6.2 cm), she was small in stature (113.1 cm). Her medical history revealed epileptic seizures at 9 years of age and a congenital ventricular septal defect. Her facial profile was convex with a retrognathic mandible (
Figure 1). An increased lower facial height, facial asymmetry, and circumoral muscle strain on lip closure were observed. She was in the mixed dentition stage and exhibited an anterior crossbite, with an overjet of −1.5 mm and an Angle Class III molar relationship on both sides (
Figure 2). Surgical scars were present on the distal side of the maxillary left central incisor, which was mesially rotated by 90°. The maxillary and mandibular arches were narrow, with moderate crowding in the mandibular incisor region. Clinical examination and a panoramic radiograph revealed the congenital absence of the maxillary left lateral incisor and all second premolars (
Figure 3). An alveolar bone defect was observed between the maxillary left lateral incisor and the deciduous canine. Lateral and posteroanterior cephalograms showed digitate impressions on the surface of the skull and a deviated nasal septum. Cephalometric analysis (
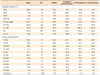
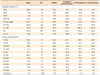
Table 1) showed a skeletal Class II relationship (A point-nasion-B point angle, ANB; 9.0°) with mandibular retrusion (sellanasion-B point angle, SNB; 67.0°). In addition, the mandibular body was short compared with the Japanese norms.
12 The mandibular plane (Mp) angle was steep and the ramus plane (Rp) was rotated clockwise (Mp–Frankfort [FH] plane, 39.0°; Rp–FH, 90.5°). The maxillary and mandibular incisors were lingually inclined and extruded (upper incisor axis to FH, U1–FH, 99.0; angle between axial inclination of mandibular central incisor and Mp, L1–Mp, 85.5°; perpendicular distance of U1 to nasal floor, U1/NF, 32.5 mm; perpendicular distance of L1 to MP, L1/MP, 44.5 mm).
On the basis of her small stature and medical history of seizures, a ventricular septal defect, and UCLP, we suspected a syndrome. However, a plastic surgeon ruled out any syndrome. Therefore, we diagnosed the patient with Angle Class III malocclusion, a skeletal Class II jaw relationship, an anterior crossbite, moderate mandibular incisor crowding, and left-sided UCLP. The treatment objectives were as follows: correction of the anterior crossbite, expansion of the maxillary alveolar cleft before bone grafting, and achievement of dental alignment and leveling for adequate intercuspation. Orthognathic surgery was planned as the second phase of treatment if the maxilla and/or mandible failed to show ideal growth after permanent tooth eruption and growth completion.
First, the narrow maxillary arch was expanded using a quadhelix device before bone grafting at 10 years of age. Alveolar bone grafting was performed at 10 years and 3 months of age to close the left-sided UCLP and ensure continuity of the alveolar bone. After successful bone grafting, the maxillary crossbite and maxillary incisor angulation were corrected using a lingual arch at 11 years and 3 months of age. Patients with CLP usually exhibit skeletal Class III malocclusion with maxillary deficiency because of the cleft itself and fibrous scar tissue formation caused by reconstructive surgery. However, in our patient, at the completion of maxillary and mandibular growth, we recognized downward and backward rotation of the mandible caused by the lack of forward growth and excessive vertical growth of the maxilla from the cephalometric superimposition (
Figure 4). Furthermore, the mandibular notch had become significantly deeper relative to the initial position (
Figure 4C). As a result, the facial profile appeared significantly retrognathic compared with the initial profile (
Figure 5). Moreover, an excessive overjet and an anterior open bite were observed (
Figure 6). The SNB angle had decreased by 6.5° and the ANB and Mp-FH angles had increased by 5.5° and 10.0°, respectively (
Table 1). The L1/Mp had increased by 8.0 mm. In addition, bilateral finger-shaped condyles with anterior bone surface resorption were observed (
Figures 7 and
8).
We reassessed the patient at the beginning of the second phase of treatment and diagnosed suspected bilateral PCR on the basis of the growth pattern and imaging findings.
TREATMENT OBJECTIVES
The treatment objectives in the second phase were as follows: correction of the retrognathic facial profile from esthetic and functional perspectives, correction of the anterior open bite and excessive overjet, and achievement of an acceptable occlusion.
TREATMENT ALTERNATIVES
To achieve the abovementioned treatment objectives, surgical orthodontic treatment with double-jaw surgery (Le Fort I intrusion osteotomy and mandibular ramus osteotomy) was considered necessary to advance the mandible. BSSO and DO are the most common procedures for surgical mandibular advancement and generally result in good treatment outcomes. However, we suspected bilateral PCR in our patient and preferred to avoid mandibular advancement osteotomy to prevent any further condylar resorption. Therefore, we planned Le Fort I osteotomy with genioplasty to avoid ingravescence of PCR and achieve counterclockwise rotation of the mandible. We planned two genioplasty procedures to achieve an esthetic facial profile through advancement and vertical reduction of the chin.
The maxilla must be positioned posteriorly in cases of maxillary impaction to achieve autorotation of the mandible. To eliminate the risk of forward repositioning of the maxilla by posterior interference, we reluctantly decided to extract the impacted second molar to create enough space for setback osteotomy.
TREATMENT PROGRESS
In the second phase of treatment, at 15 years and 6 months of age, preadjusted edgewise appliances with 0.018-inch slots were placed in the maxilla and mandible and leveling of both arches was initiated. The patient also had to wear a high-pull headgear appliance at least 10 hours per day for intrusion of the maxillary molars and prevention of clockwise mandibular rotation caused by molar extrusion. After 18 months of presurgical orthodontic treatment, we observed discontinuation of mandibular growth and active condylar erosion by superimposition of serial cephalometric tomograms obtained in the last 6 months. Therefore, Le Fort I intrusion osteotomy was performed with advancement genioplasty and extraction of the maxillary second molar. The maxilla was impacted by 7.0 mm in the incisor region and 5.0 mm in the first molar region, and the chin was advanced by 11.0 mm because of counterclockwise rotation of the mandible led by maxillary impaction and advancement genioplasty. During postsurgical orthodontic treatment, a second genioplasty procedure was performed with 8.0-mm advancement and 6.0-mm vertical reduction of the chin, along with rhinocheiloplasty. The preadjusted edgewise appliances were removed at 24 months after orthognathic surgery. Subsequently, a vacuum-formed retainer for the maxillary arch and a vacuum-formed retainer and a lingually bonded retainer for the mandibular arch were provided for retention. The total duration of active treatment was 42 months.
RESULTS
The patient’s post-treatment records showed significant resolution of both skeletal disharmony and malocclusion (
Figures 9,
10,
11). The strain observed in the circumoral musculature during mouth closure also disappeared. An ideal overjet and overbite were achieved with acceptable interdigitation. The dental midlines coincided with the facial midline. Cephalometric evaluation showed an increased SNB angle (64.0°) and a decreased Mp-FH angle (34.0°), although the skeletal jaw relationship was still Class II (ANB, 11.0°;
Table 1). The maxilla was impacted by 7.0 mm in the incisor region and 5.0 mm in the first molar region, while the pogonion was advanced by 18.0 mm through mandibular counter-clockwise rotation and the two advancement genioplasty procedures (
Figure 12). The mandible showed desirable counterclockwise rotation. The maxillary molars were tipped backward and the mandibular molar was upright. The maxillary incisors were lingually inclined. Morphological changes in the bilateral condyles were not observed on computed tomography (
Figure 13). In addition, hyoid bone advancement and an increased pharyngeal airway volume were observed (
Figure 14).
At the 30-month follow-up examination, we observed a satisfactory facial profile and a slightly decreased overbite (
Figure 15). Cephalometric superimposition showed that the maxilla and chin were stable. There were minimal changes in the dentition and negligible clockwise rotation of the mandible (
Figure 12).
DISCUSSION
We described the effective treatment of severe mandibular retrognathism with suspected PCR using Le Fort osteotomy and two genioplasty procedures, thus eliminating the need for surgical mandibular advancement. The treatment was mainly aimed toward achieving satisfactory esthetics and respiratory function and long-term stability.
To achieve improved esthetics and simultaneously avoid condylar overloading, Le Fort I osteotomy for superior repositioning of the maxilla and advancement genioplasty for counterclockwise rotation of the mandible and anterior projection of the chin were performed. DO and BSSO are two commonly used procedures for the treatment of mandibular retrognathism from esthetic and functional perspectives.
67 However, these procedures occasionally result in PCR, particularly in patients who undergo long-span mandibular advancement with continuous overloading in the TMJ region.
81113 Although the precise etiology of PCR remains unclear, TMJ stress or overloading is considered one of the main causes.
91014 Unfortunately, despite the presence of severe mandibular retrognathism, our patient developed finger-shaped condyles on both sides after the first phase of orthodontic treatment, probably because of bone surface absorption. Condylar malformation is also suggested as a risk factor for PCR.
11 Because our patient had suspected PCR and was at a high risk of further resorption with surgical mandibular advancement, we decided to perform Le Fort I osteotomy with two advancement genioplasty procedures and avoided mandibular surgery, which would improve the facial profile without stressing the TMJ at the end of mandibular growth. Some studies have reported a relationship between Le Fort I osteotomy with superior repositioning and condylar resorption. Hoppenreijs et al.
15 reported that the incidence of condylar resorption was 9% with Le Fort I intrusion osteotomy only, and this was lower than the incidence with bimaxillary osteotomies in patients with an anterior open bite. They suggested that intermaxillary fixation (IMF) with rigid internal fixation should be avoided to minimize condylar changes. Therefore, we used compression bandages around the head and neck as an alternative to IMF after Le Fort I osteotomy. Consequently, no significant changes in the condylar morphology were observed at 24 months after surgery.
To assess the respiratory function, we evaluated the pharyngeal area by superimposition of pre-treatment and post-treatment cephalograms (
Figure 14A) and the airway volume using the Dolphin 3D software (Dolphin Imaging and Management Solutions, Chatsworth, CA, USA) for airway analysis (
Figure 14B). The results showed hyoid bone advancement and an increased pharyngeal airway space and volume. Severe mandibular retrognathism is often accompanied by pharyngeal airway obstruction,
3 probably because of downward displacement of the tongue. Therefore, advancement genioplasty can achieve extensive anterior retraction of the suprahyoid musculature and decrease the signs and symptoms of obstructive sleep apnea syndrome, including the apnea–hypopnea index.
1617 Moreover, the posterior airway space significantly increases after advancement genioplasty.
1819 Our patient also snored during her sleep before treatment, and we believe that her treatment has minimized any future risks of obstructive sleep apnea.
With regard to long-term stability, the maxillary, chin, and jaw positions appeared stable at the 30-month follow-up examination in our patient. Le Fort I osteotomy with superior repositioning of the maxilla and advancement genioplasty are considered more stable than other procedures.
20 In fact, these procedures have been successfully used for effective correction of juvenile idiopathic/rheumatoid patients.
21 We suggest that maxillary impaction surgery with advancement genioplasty offers a good prognosis without ingravescence of PCR.
At the 30-month follow-up examination for our patient, we observed a slight decrease in the overbite caused by a moderate relapse in the mandibular dentition. We will continue careful follow-ups for her, considering that surgically treated patients are generally at a high risk of relapse because of condylar remodeling or other skeletal changes.
2
CONCLUSION
In the present report, we showed that Le Fort I osteotomy with two advancement genioplasty procedures was effective for the treatment of severe mandibular retrognathism with suspected PCR and eliminated the need for surgical mandibular advancement using BSSO or DO, which increases the risk of PCR in some patients. The findings from our case suggest that this surgical treatment is effective for the correction of occlusion and esthetics in patients with severe mandibular retrognathism and condylar deformities, thus decreasing the risk of PCR observed with surgical mandibular advancement.
Figures and Tables
Figure 1
Initial facial and intraoral photographs of our patient who was diagnosed with Angle Class III malocclusion, a skeletal Class II jaw relationship, an anterior crossbite, congenital absence of some teeth, and a left-sided cleft lip and palate at 9 years and 9 months of age.

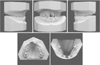
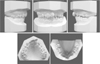
Figure 2
Initial dental casts.
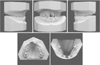
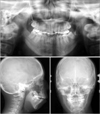
Figure 3
Initial panoramic and cephalometric radiographs.

Figure 4
Superimposition of cephalometric tracings obtained before, during, and after the first phase of interceptive orthodontic treatment. A, Superimposition on the sella– nasion plane at the sella. B, Superimposition on the palatal plane at the anterior nasal spine (ANS) and the mandibular plane at the menton. C, Superimposition on the ramus plane at the articulare.

Figure 5
Facial and intraoral photographs obtained before the second phase of treatment for our patient who exhibited severe mandibular retrognathism with bilateral condylar deformities after growth completion.

Figure 6
Dental casts fabricated before the second phase of treatment.
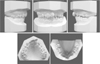
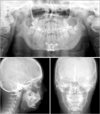
Figure 7
Panoramic and cephalometric radiographs obtained before the second phase of treatment.
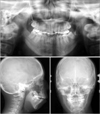
Figure 8
Computed tomography images of the bilateral condyles for our patient with bilateral condylar deformities after growth completion. The arrowheads show bone surface absorption.

Figure 9
Facial and intraoral photographs obtained after Le Fort I osteotomy with two advancement genioplasty procedures followed by fixed orthodontic treatment.

Figure 10
Dental casts fabricated after treatment.

Figure 11
Panoramic and cephalometric radiographs obtained after treatment.
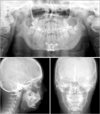
Figure 12
Superimposition of cephalometric tracings obtained before the second phase of treatment and after Le Fort I osteotomy with two advancement genioplasty procedures followed by fixed orthodontic treatment and after retention. A, Superimposition on the sellanasion plane at the sella. B, Super impo s i t ion on the palatal plane at the posterior nasal spine (PNS). C, Superimposition at the gonion.

Figure 13
Computed tomography reconstructions obtained before (A–D) and after (E–F) Le Fort I osteotomy with two advancement genioplasty procedures followed by fixed orthodontic treatment and retention for our patient who exhibited severe mandibular retrognathism with bilateral condylar deformities after growth completion.

Figure 14
Assessment of the airway space after treatment. A, Superimposition of cephalometric tracings with the pharyngeal area (black, before treatment; red, after treatment). B, Airway volume measurements obtained using the Dolphin 3D software (Dolphin Imaging and Management Solutions, Chatsworth, CA, USA) for airway analysis.

Figure 15
Facial and intraoral photographs obtained at 30 months after treatment.

Table 1
Cephalometric measurements obtained at different time points during the two phases of treatment and after retention












 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download