Abstract
Background and Purpose
We compared the motor-unit number estimation (MUNE) findings in patients who presented with signs and/or findings associated with carpal tunnel syndrome (CTS) and healthy controls, with the aim of determining if motor-unit loss occurs during the clinically silent period and if there is a correlation between clinical and MUNE findings in CTS patients.
Methods
The study investigated 60 hands of 35 patients with clinical CTS and 60 hands of 34 healthy controls. Routine median and ulnar nerve conduction studies and MUNE analysis according to the multipoint stimulation method were performed.
Results
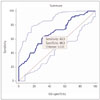
The most common electrophysiological abnormality was reduced conduction velocity in the median sensory nerve (100% of the hands). The MUNE value was significantly lower for the patient group than for the control group (p=0.0001). ROC analysis showed that a MUNE value of 121 was the optimal cutoff for differentiating between patients and controls, with a sensitivity of 63.3% and a specificity of 68.3%. MUNE values were lower in patients with complaints of numbness, pain, and weakness in the median nerve territory (p<0.05, for all comparisons), and lower in patients with hypoesthesia than in patients with normal neurological findings (p=0.023).
Conclusions
The MUNE technique is sensitive in detecting motor nerve involvement in CTS patients who present with sensorial findings, and it may be useful in detecting the loss of motor units during the early stages of CTS. Larger-scale prospective clinical trials assessing the effect of early intervention on the outcome of these patients would help in confirming the possible benefit of detecting subclinical motor-unit loss in CTS.
Carpal tunnel syndrome (CTS) is a group of symptoms that occur due to compression of the median nerve in the portion of the carpal tunnel between the wrist and palmar segment. CTS is the most frequent type of nerve entrapment and is most commonly diagnosed via electrophysiological examinations.12 Routine nerve conduction studies (NCS), including examination of median nerve sensory fibers, are very helpful for diagnosing CTS,34 but other methods such as motor-unit number estimation (MUNE) are also used.5678910 MUNE is a unique electrophysiological technique that can provide a numeric estimate of the number of axons innervating a muscle or group of muscles.11 The primary causes of motor disability in patients with CTS are atrophy and weakness, which occur in hand muscles as a result of the loss of motor units. The compound muscle action potentials (CMAPs) are decreased only in patients with advanced-stage CTS.12 An ideal electrophysiological examination should be capable of detecting motor-unit loss at an early stage of CTS or, more importantly, before clinical signs and symptoms associated with motor dysfunction appear.
In this study we compared MUNE findings between patients who presented with signs and/or findings associated with CTS and healthy controls, with the aim of determining if motor-unit loss occurs during the clinically silent period of CTS and if there is a correlation between clinical and MUNE findings in CTS patients.
During a 6-month period, 60 hands of 35 patients (3 male and 32 female) with clinical features indicative of CTS (i.e., presence of pain, paresthesia, and numbness/tingling in the distribution of the median nerve for at least 1 month) were enrolled. Prior to electrophysiological examinations, various characteristics of the patients were recorded, including age, sex, height and weight, symptom duration, dominant hand, symptomatic hand/s, presence of hypoesthesia and pain in digits 1-3, and complaints of weakness or clumsiness when using hands. Sensory and motor deficits in the median nerve distribution areas and the findings for Tinel's sign and Phalen's maneuver were also noted. Normative data were obtained from electrophysiological studies of 60 hands of 34 healthy controls (4 male and 30 female) without any risk factors for neuropathy and no neurological symptoms or signs of neuropathy.
The study protocol conformed to the Helsinki Declaration of Human Rights and was approved by the local Ethics Committee. All of the subjects provided written informed consent to participate in the study. Participants with cervical radiculopathy, diabetes mellitus, any disease that can cause loss of MUNE [e.g., amyotrophic lateral sclerosis (ALS), neurodegenerative disorders, and polyneuropathies], Martin-Gruber anastomosis, history of surgery for CTS, or any neurological disorder that can lead to degenerative, demyelinating, inflammatory, or traumatic effects in the central nervous system were excluded from the study.
Two experienced investigators (O.Y. and G.S.) performed all of the electrophysiological studies and one investigator (K.U.) reviewed all of the data offline; all three investigators were blinded to the patient and control groups.
NCS and MUNE were performed using a Medelec Synergy ENMG device (Oxford Instruments Medical Ltd., Old Working, UK). All of the participants underwent median and ulnar motor and sensory NCS of the bilateral upper extremities using superficial recording and stimulus electrodes, according to the methods described by Stålberg and Falck13 and Falck et al.14 The minimum F-wave latency was measured in all of the tested motor nerves.
Sensory NCS were performed using the antidromic method. For median sensory NCS, the recording electrodes were placed over the second digit and the nerves were stimulated at the wrist approximately 2 cm proximal to the distal crease of the forearm at a distance of 14 cm from the recording electrode. Ulnar sensory NCS were performed by placing the recording electrode on the palmar surface of the fifth digit and stimulating the nerve from the medial wrist (near the tendon of the flexor carpi ulnaris) at a distance of 14 cm from the recording electrode. The onset latency, amplitude, and velocity were measured in sensory NCS. The amplitude of the sensory nerve action potentials (SNAPs) was measured from baseline to the negative peak. The maximum SNAPs were obtained by applying a supramaximal stimulus intensity (i.e., at least threefold greater than the sensory threshold). The SNAP was accepted as being absent when there was no recognizable SNAP or when the SNAP was not repeatable and constant. The SNAP was recorded as the average of eight responses.
The distal latency, CMAP amplitude and velocity, and minimum F-wave latency were calculated for motor NCS. For median motor NCS, the recording electrodes were placed over the belly of the abductor pollicis brevis (APB) muscle, with the reference electrodes over the first metacarpophalangeal joint. The nerve was stimulated first on the wrist at 80 mm proximal to the recording electrode, and then at the elbow. The ulnar motor nerve was stimulated at the wrist, below the elbow, and above the elbow while recording at belly of the abductor digiti minimi muscle.
The median motor nerve recording electrode was placed on the volar field in the middle of the space between the wrist line and metacarpophalangeal joint, which is the most projecting part of the APB muscle. The stimulus was applied 80 mm from the recording electrode between the flexor carpi radialis and palmaris longus tendons from the medial antecubital space and lateral brachial artery at the level of the wrist.
The sensitivities of the measured median sensory nerve study parameters were calculated using the clinical criteria as a gold standard, as recommended by the American Academy of Electrodiagnostic Medicine Quality Assurance Committee, the American Academy of Neurology, and the American Academy of Physical Medicine and Rehabilitation.15
MUNE analysis was performed in all participants using the multipoint stimulation method.1617 By stimulating the nerve at several sites, this technique yields data from motor units with different morphologies. The recording electrode was placed on the most-projecting point of the APB muscle and a maximum CMAP was obtained by applying a supramaximal stimulus. The MUNE program recorded the maximum CMAP amplitude obtained. Next, at the stimulus point on the wrist, nine surface-detected motor-unit action potentials (SMUAPs) were measured at three time points from each of three different points separated by an interelectrode distance of 1 cm. Stimulation was applied at 1 Hz with 100-µs pulses, beginning with a site just proximal to the thenar motor point. The stimulus intensity was gradually increased to the level at which a single all-or-nothing SMUAP was obtained. When reproducible SMUAPs—free of any indication of alteration—could not be elicited, the stimulator was moved slightly to a new site. The mean value of the nine single SMUAPs was calculated and then divided by the maximum CMAP amplitude to obtain the MUNE value.
None of the participants of the study complained about discomfort or pain during the MUNE examination, which took approximately 15 minutes in each subject.
The NCS data were analyzed statistically using SAS Enterprise Guide (version 5.1). The chi-square test was used to compare demographic characteristics between two groups. The Shapiro-Wilk test was used to assess the normality of the distribution of quantitative data. Arithmetic mean±SD values were calculated for each electrophysiological parameter. The criterion for abnormality was determined as the arithmetic mean±2 SD, varying according to the data type; that is, a latency value of greater than the arithmetic mean plus 2 SD was accepted as abnormal, whereas velocity and amplitude values less than the arithmetic mean minus 2 SD were considered abnormal. The sensitivity of each parameter was calculated as a percentage: the number of hands with a positive electrodiagnostic test and clinical CTS divided by the number of hands with clinical CTS×100%. The t-test was used to compare mean electrophysiological parameter values between two groups. Pearson's correlation coefficients were used to analyze correlations. The cutoff for statistical significance was set at p<0.05.
In total, 60 symptomatic hands of 35 (3 male and 32 female) CTS patients and 60 hands of 34 (4 male and 30 female) healthy controls were analyzed. Data were collected prospectively. There were no significant differences in age, sex distribution, height, weight, or hand dominancy between the two groups (p>0.05 for all comparisons). The demographic features of the patients and controls are listed in Table 1.
The duration of CTS symptoms in the patient group ranged from 3 months to 60 months (mean: 16.9 months). Pain in the first three digits, numbness in the first three digits, and weakness were reported for 45 (75%), 53 (88.3%), and 6 (10%) of the patients' hands, respectively. Neurological examinations revealed hypoesthesia in the median nerve territory in 33 (55%) hands, but no motor weakness or atrophy was found in any of the patients. Tinel's sign and Phalen's maneuver were positive in 53 (88.3%) and 47 (78.3%) of the patients' hands, respectively.
Detailed electrophysiological findings are presented in Table 2. The Shapiro-Wilk normality test revealed that all of the NCS parameters had normal distributions. All of the evaluated electrophysiological parameters except latency values of the sensory and motor ulnar nerves differed significantly between patients and controls. All of the 60 clinically diagnosed CTS hands showed a lower than normal conduction velocity in the median sensory nerve [100% of the patients' hands (60/60 hands)]. Although the mean amplitude and velocity values for the ulnar sensory nerve differed significantly between the patient and control groups, individual abnormality rates of these parameters for the patients' hands were very low (rates of abnormal hands with respect to amplitude and velocity values for ulnar sensory nerve were 5% and 0%, respectively). Prolonged distal latency of the median motor nerve was the most common individual abnormality of motor nerve conduction (51.6%). Reduced median motor nerve conduction velocity was noted in only five (8.3%) patients' hands, and none of the patients had a reduced CMAP amplitude of the median motor nerve.
The MUNE value was significantly lower in the patient group (114.46±26.07) than in the control group (136.36±30.81, p=0.0001). ROC analysis showed that a MUNE value of 121 was the optimal cutoff for differentiating between patients and controls, with a sensitivity of 63.3% and a specificity of 68.3% (Fig. 1). None of the evaluated parameters for the median sensory nerve were correlated with hypoesthesia, whereas a significant correlation was found between hypoesthesia and MUNE value (p=0.001). There was a significant correlation between weakness symptom and MUNE value (p=0.035). Pain in the first three digits was significantly correlated with median motor velocity (p=0.045) and MUNE value (p=0.001). The MUNE value was also significantly correlated with numbness in the first three digits (p=0.023). None of the electrophysiological parameters was correlated with the MUNE value (p>0.05 for all of the analyzed electrophysiological parameters).
The present study compared MUNE findings between patients who presented with signs and/or findings associated with CTS and healthy controls, and monitored the loss of motor units in the CTS patients. In addition, correlations between the clinical manifestations of CTS and MUNE values were investigated. Based on the present findings, although none of the analyzed CTS patients presented with objective complaints of loss of strength, MUNE values were significantly lower in the patient group than in the control group. Moreover, among all of the tested electrophysiological parameters, the MUNE value showed the highest sensitivity for detecting individual abnormality in motor nerves. Analysis of the correlation between clinical and electrophysiological data showed that symptoms including pain, numbness, and weakness with hypoesthesia based on a clinical examination were significantly correlated with a low MUNE value.
The primary causes of motor disability in CTS patients are impaired hand functions, atrophy, and hand muscle fatigue, all of which result from the loss of motor units. An ideal electrophysiological method should be able to detect the electrophysiological correlation of these symptoms during the early stage, especially before clinical signs and symptoms of motor dysfunction appear. Although routine NCS are easy to perform, and are repeatable and reliable, their most important drawback is an inability to detect early-stage loss of motor units. During the slowly progressing clinical picture of CTS, the CMAP amplitude of the relevant median motor nerve is generally found to be within normal limits. Reinnervation of muscle fibers via collateral sprouting by the axons of the surviving motor units means that the CMAP amplitude does not change much until there is serious loss of axons.18 In contrast, MUNE seems to be an ideal method for evaluating motor fibers, since it provides data on motorunit dysfunction during the early stage of CTS.910
A motor unit is the structural unit that triggers the contraction of skeletal muscle. A motor unit is composed of an alpha motor neuron, the axonal terminal of the motor neuron, and muscle fibers innervated by that axon.18 There is no method for accurately determining the number of motor units, and so MUNE is the most reliable method at present even though it determines the number of motor units only indirectly.111819 Several MUNE methods have been described so far, all of which rely on the same principle of calculating the number of motor units by dividing the maximum CMAP by the average SMUAP, and established normative data sets and high reproducibility are available for all of them.1920 In the incremental stimulation method, since the stimulus intensity is increased progressively beyond the motor threshold, each successive increment in the CMAP is accepted to represent a single SMUAP, and then the average SMUAP size is found by dividing the CMAP amplitude by the number of component quantal steps. The MUNE value is obtained by calculating the ratio of the maximum CMAP divided by the average size of the SMUAPs. However, this method has the disadvantage of the motor axon stimulation thresholds overlapping at a given stimulus intensity, which is called the phenomenon of alternation. Therefore, the multiple point stimulation technique—in which the motor nerve is stimulated at various sites—is applied to collect a sample of SMUAPs that are free of alternation. The use of MUNE has been analyzed in various neuromuscular and neurodegenerative disorders, including anterior horn cell diseases such as ALS, spinal muscular atrophy, polio, and postpolio syndrome, and pathologies that affect motor fibers, such as polyneuropathy, radiculopathy, and entrapment neuropathies.111920
The use of MUNE was first described in 1973 in CTS patients, when it was reported that MUNE values decreased in some patients who did not exhibit clinical signs or symptoms of motor fiber involvement.6 Although that study included only 19 patients, the findings were important in indicating that subclinical motor fiber involvement can occur in CTS patients. Cuturic and Palliyath7 similarly reported that using a modified statistical MUNE method revealed a clinically silent period of loss of motor units before clinical signs and symptoms became evident in patients with mild-to-moderate CTS; however, that study did not examine correlations between clinical characteristics and MUNE. Koç et al.8 found that MUNE values were lower in 50 CTS patients than in controls. Significant correlations between MUNE, clinical, and electrophysiological findings have also been reported.910
None of the patients in the present study exhibited objective clinical motor abnormality, but their MUNE values were significantly lower than in the control group. Since it is clinically more useful to detect individual abnormality than to perform between-group comparisons of polyneuropathy or entrapment neuropathies, the sensitivity of MUNE for detecting individual abnormality was analyzed. Based on a MUNE cutoff of 121, individual abnormality was observed in 63% of the CTS patients' hands (38/60 of patients' hands), and the diagnostic sensitivity was higher when using this cutoff than when using any of the other conduction parameters of the motor nerve. Detecting the loss of motor units during the clinically silent period in CTS patients can be useful for determining the effect of the disease on motor axons (during the clinically silent period) and can aid in determining the progression of the disease and the treatment response during patient follow-up.
Similar to previous studies,910 we also found that some of the clinical signs and symptoms of CTS were correlated with MUNE findings. MUNE values were lower in patients with complaints of numbness, pain, and weakness in the median nerve territory. Also, patients with hypoesthesia showed significantly decreased MUNE values than patients with normal neurological findings. These parameters were accepted as substantially reflecting motor-unit involvement. Other findings obtained in the present study are similar to those reported previously. The sensitivity of routine motor NCS was not as high as that of sensory NCS. The most commonly observed nerve conduction abnormalities were decreased median sensory nerve conduction velocity, prolonged onset latency of the median sensory nerve, and prolonged distal latency of the median motor nerve. These findings are all highly suggestive of a demyelinating type of abnormality, but according to the MUNE findings we may also speculate that an axonal influence was present in at least some of the patients.
The most important limitations of the present study are the small number of patients' hands included and only obtaining baseline patient MUNE values. Additionally, because a squeeze dynamometer was not available in our center, we could not assess the muscle power quantitatively, and needle EMG was not performed since the findings of motor examinations were completely normal and those of motor NCS were within normal limits. However, it would have been better to also compare the MUNE results with other parameters related to the loss of motor axons.10
In conclusion, the present findings indicate that the MUNE technique is more sensitive than routine motor NCS in detecting motor nerve involvement in CTS patients who present with sensorial findings and the loss of motor units during the early stages of CTS. The demonstration of subclinical involvement of motor axons might alert the physician to take strict preventive measures in managing these patients and might avoid their progression to the overt clinical involvement of motor nerves with more severe symptoms. Larger-scale prospective clinical trials assessing the effect of early intervention on the outcome of these patients would help in confirming the possible benefit of detecting subclinical motor-unit loss in CTS.
Figures and Tables
Table 1
Clinical characteristics in the patient and control groups

Table 2
Electrophysiological findings in the patient and control groups

References
1. Katz JN, Simmons BP. Clinical practice. Carpal tunnel syndrome. N Engl J Med. 2002; 346:1807–1812.
3. Stevens JC. AAEM minimonograph #26: the electrodiagnosis of carpal tunnel syndrome. American Association of Electrodiagnostic Medicine. Muscle Nerve. 1997; 20:1477–1486.

4. Jablecki CK, Andary MT, Floeter MK, Miller RG, Quartly CA, Vennix MJ, et al. Practice parameter: electrodiagnostic studies in carpal tunnel syndrome. Report of the American Association of Electrodiagnostic Medicine, American Academy of Neurology, and the American Academy of Physical Medicine and Rehabilitation. Neurology. 2002; 58:1589–1592.

5. McComas AJ, Fawcett PR, Campbell MJ, Sica RE. Electrophysiological estimation of the number of motor units within a human muscle. J Neurol Neurosurg Psychiatry. 1971; 34:121–131.

6. Brown WF. Thenar motor unit count estimates in the carpal tunnel syndrome. J Neurol Neurosurg Psychiatry. 1973; 36:194–198.
7. Cuturic M, Palliyath S. Motor unit number estimate (MUNE) testing in male patients with mild to moderate carpal tunnel syndrome. Electromyogr Clin Neurophysiol. 2000; 40:67–72.
8. Koç F, Yerdelen D, Sarica Y, Sertdemir Y. Motor unit number estimation in cases with Carpal Tunnel Syndrome. Int J Neurosci. 2006; 116:1263–1270.

9. Bayrak IK, Bayrak AO, Tilki HE, Nural MS, Sunter T. Ultrasonography in carpal tunnel syndrome: comparison with electrophysiological stage and motor unit number estimate. Muscle Nerve. 2007; 35:344–348.

10. Sohn MK, Jee SJ, Hwang SL, Kim YJ, Shin HD. Motor unit number estimation and motor unit action potential analysis in carpal tunnel syndrome. Ann Rehabil Med. 2011; 35:816–825.

12. Padua L, LoMonaco M, Gregori B, Valente EM, Padua R, Tonali P. Neurophysiological classification and sensitivity in 500 carpal tunnel syndrome hands. Acta Neurol Scand. 1997; 96:211–217.

13. Stålberg E, Falck B. Clinical motor nerve conduction studies. Methods Clin Neurophysiol. 1993; 4:61–80.
14. Falck B, Stålberg E, Bischoff C. Sensory nerve conduction studies with surface electrodes. Methods Clin Neurophysiol. 1994; 5:1–20.
15. Jablecki CK, Andary MT, So YT, Wilkins DE, Williams FH. Literature review of the usefulness of nerve conduction studies and electromyography for the evaluation of patients with carpal tunnel syndrome. AAEM Quality Assurance Committee. Muscle Nerve. 1993; 16:1392–1414.

16. Kadrie HA, Yates SK, Milner-Brown HS, Brown WF. Multiple point electrical stimulation of ulnar and median nerves. J Neurol Neurosurg Psychiatry. 1976; 39:973–985.

17. Doherty TJ, Stashuk DW, Brown WF. Multiple point stimulation and F-response MUNE techniques. Suppl Clin Neurophysiol. 2003; 55:29–40.

19. Bromberg MB. Motor unit number estimation: new techniques and new uses. Suppl Clin Neurophysiol. 2004; 57:120–136.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download