Abstract
Background and purpose
Zonisamide (ZNS) is a useful antiepileptic drug with a broad therapeutic spectrum. However, there is limited information on the long-term use of ZNS as a monotherapy. This study investigated the long-term effects of ZNS as a monotherapy for the treatment of epilepsy.
Methods
We retrospectively analyzed the records of epilepsy patients treated with ZNS monotherapy at our clinic. We identified outcomes for patients treated with ZNS monotherapy for a minimum of 6 months. Efficacy was quantified as the percentage change in seizure frequency, and safety was assessed by the frequency and types of adverse events.
Results
Sixty patients who received ZNS for a minimum of 6 months were included. The mean duration of treatment was 19.8 months (range, 6-37 months), and the mean ZNS dosage was 255 mg/day (range, 100-500 mg/day). Twenty-seven patients (45%) were seizure-free, and an additional 20 patients (33%) had above 50% seizure frequency reduction at the last follow-up visit. Partial seizures with or without secondary generalization and generalized seizures were well controlled by ZNS, whereas complex partial seizures were not. Forty-eight patients (80%) reported mild-to-moderate adverse events, including memory loss (35%), attention deficit (27%), and weight loss (20%).
Zonisamide (ZNS, Exegran®) has been shown to be a useful antiepileptic drug (AED) with a broad therapeutic spectrum.1-3 It has been used in Japan since 1989, and is effective against simple and complex partial seizures, generalized tonic-clonic seizures (GTCS), myoclonic epilepsies, Lennox-Gastaut syndrome, and infantile spasms.4 ZNS was introduced into the South Korean market in June 1992, and subsequently approved as a monotherapy. Recently, ZNS mono- or add-on therapy (100-1100 mg/day) was shown to be a safe, effective, and well-tolerated long-term treatment option in pediatric and adult epilepsy patients.5-12 Among them, 26-61% of patients reported mild-to-moderate adverse events, and the severity of these events tended to decrease over time, suggesting that patients develop a tolerance to them.10
During the period of introduction of ZNS into the Korean market, several studies evaluated its efficacy and safety in epilepsy patients.13-17 Patients received ZNS dosages ranging from 100 to 600 mg/day for periods from 2 to 15 months. Seizure freedom occurred in 0-30% of patients, and a seizure frequency reduction of ≥ 50% was demonstrated in 55-83% of patients. Mild-to-moderate adverse events such as gastrointestinal troubles, dizziness, somnolence, weight loss, and headache were detected in 35-69% of patients. Although these studies have provided information about the usefulness of ZNS in epilepsy patients, they did not provide any information about the effectiveness of long-term ZNS monotherapy in newly diagnosed epilepsy, because the majority of studies considered only the short-term (≤ 6 months) effectiveness of ZNS as an add-on therapy for intractable epilepsy. More recently, a double-blind, randomized, comparative study of ZNS and carbamazepine (CBZ) as a monotherapy in newly diagnosed epilepsy was conducted by the Korean ZNS Group.18 The 24-week remission rate of seizures with 302 mg/day ZNS was 69.9%, which was similar to that of 611 mg/day CBZ. The mean time to the first seizure recurrence in the ZNS group was 41 days, which was also similar to that of CBZ group. Although the profiles of adverse events differed between ZNS and CBZ, the incidence of these events did not differ significantly between the two groups (67.1% and 53.7%, respectively). Although that study concluded that ZNS was as effective and safe as CBZ as a 6-month therapy, it did not elucidate the long-term effectiveness of ZNS monotherapy.
In the current study, we evaluated the efficacy and safety of long-term treatment with ZNS as a monotherapy (6-37 months) by reviewing charts of 60 patients treated at our epilepsy clinic.
A retrospective chart review was conducted to identify outcomes for patients with epilepsy who had received long-term ZNS monotherapy (≥ 6 months) in our epilepsy clinic between January 2000 and June 2007. ZNS monotherapy was applied to patients with either newly diagnosed epilepsy or formerly diagnosed epilepsy who were not treated at clinic visits.
The efficacy of ZNS was quantified using the baseline seizure frequency for 3 months before therapy and compared with seizure frequency for the same period at the end of treatment, defined as: seizure freedom, ≥ 75% reduction, ≥ 50% reduction, < 50% reduction, or no effect. The response rate of ZNS on seizure was calculated by the frequency of patients with ≥ 50% seizure frequency reduction among all patients. Patients who discontinued ZNS treatment before 6 months or whose seizure response data were unavailable were not included in the efficacy analyses. The frequencies and types of adverse events were recorded to assess the safety of ZNS. In order to assess changes in adverse events over time, we compared the frequency of adverse events before 6 months (a short-term treatment) with that after 6 months of medication (a long-term treatment). The seizure frequency and side effects, as reported by the patients, were recorded by a physician at follow-up clinic visits.
The chart review revealed that 100 patients had been treated with ZNS monotherapy, of which 40 (40%) were excluded from the study due to their ZNS intake lasting less than 6 months. The reasons for incomplete medication were adverse events in 12 patients (12%), inefficacy in 10 patients (10%), spontaneous off-medication without specific reasons in 3 patients (3%), follow-up loss in 2 patients (2%), and a ZNS intake lasting less than 6 months at the time of chart review in 13 patients (13%). The discontinuation of treatment was due to cognitive dysfunction in four patients (4%). Therefore, 60 patients were included in the study.
The characteristics of epilepsy patients who received ZNS for a minimum of 6 months are listed in Table 1. Their mean age was 29.8 years (range, 16-65 years).
Similar proportions of patients experienced partial seizures and generalized seizures. Among 26 patients (43%) with generalized seizures, 20 patients were diagnosed as GTCS only and 6 patients as juvenile myoclonic epilepsy (JME). The proportion of patients with newly diagnosed epilepsy was 87%. The mean daily ZNS dosage at the last visit was 255 mg (range, 100-500 mg), and the mean duration of therapy was 19.8 months (range, 6-37 months).
The efficacy of ZNS monotherapy ranged from seizure freedom to no effect, as shown in Figure 1. Among the 60 patients, 27 patients (45%) became seizure-free, and the seizure frequency reduced by ≥ 50% was demonstrated in an additional 20 patients (33%). The response rate to ZNS was 78%. However, five patients (8%) had a poor response to ZNS (reduction in seizure frequency of < 50%), and eight patients (13%) experienced no change in seizure frequency. The efficacy of ZNS monotherapy against various seizure types is shown in Figure 2. The seizure-free rates for simple partial seizures, complex partial seizures, partial seizures with secondary generalization, and generalized seizures were 75%, 0%, 29%, and 77%, respectively. All JME patients (n=6) were seizure-free for a mean of 23 months (range, 12-34 months). The response rates of partial seizures with or without secondary generalization and generalized seizures were excellent (86-100%), whereas that of complex partial seizures was not (44%).
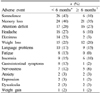
Adverse events that occurred with ZNS monotherapy are listed in Table 2. Forty-eight patients (80%) reported mild-to-moderate adverse events during long-term treatment (≥ 6 months), the most frequent of which were memory loss (35%), attention deficit (27%), and weight loss (20%). Fifty-four patients (90%) reported adverse events during short-term treatment (< 6 months), the most frequent of which were somnolence (43%), memory loss (40%), and attention deficit (28%). The frequency of CNS symptoms such as somnolence, headache, dizziness, and fatigue decreased dramatically after 6 months of treatment, with that of cognitive dysfunction and weight loss decreasing less.
This chart-review study supports previous findings on the efficacy of ZNS as a long-term monotherapy for various seizure types. With a mean ZNS treatment duration of 20 months, more than 70% of patients experienced seizure control for simple partial seizures with or without secondary generalization and generalized seizures, with the seizure-free rate being high for generalized seizures including JME. However, despite its efficacy, there was a high incidence of adverse events during ZNS medication. Cognitive impairment was a common adverse event, and this had not disappeared even after 6 months of treatment.
Recently, ZNS monotherapy (100-1000 mg/day) for durations from 2 weeks to 180 months was found to be a safe, effective, and well-tolerated treatment option in pediatric and adult epilepsy patients.5-8,11,12 Seizure freedom occurred in 24-56% of patients, and a seizure frequency reduction of ≥ 50% was demonstrated in 64-77% of patients. All seizure types responded well to ZNS monotherapy. The seizure-free rates among patients with complex partial seizures and generalized seizures were 44-62% and 34-53%, respectively. The efficacy profile of JME was not described. Our results for the seizure-free and response rates were similar to these previously reported results, except that no seizure freedom occurred in complex partial seizures and the seizure-free rate was higher (77%) in generalized seizures. A prospective, observational study of 1,102 adults with symptomatic, localization-related epilepsy found that standard AED therapy resulted in 21-28% of patients with complex partial seizures being seizure-free at 12 months.19 In contrast, none of our patients were seizure-free with ZNS therapy. Since the seizure-free rate can vary with the underlying etiology, AED therapy, or even follow-up duration, future large population studies should attempt to elucidate the efficacy of ZNS against complex partial seizures. All of our JME patients (n=6) achieved seizure freedom for almost 2 years. Although valproate has been recommended for the treatment of JME, a recent study found that 80% of patients on ZNS monotherapy showed ≥ 50% reduction in seizure frequency for 1 year.20 Despite the likelihood of ZNS being effective against generalized seizures, previous long-term studies were open-label and retrospective, and had investigated a small number of patients, and case selection bias could have been present. Therefore, further studies including larger numbers of patients are needed to clarify the true efficacy of ZNS monotherapy against specific seizure or epilepsy types.
The reported incidence of adverse events with ZNS monotherapy is 5-33%.5-8,11,12 ZNS was well tolerated and associated with only mild-to-moderate adverse events. In a postmarketing surveillance study of more than 1,000 patients treated for 1-3 years, the most common adverse events included mental/psychic, gastrointestinal, and neurological symptoms.6 Cognitive dysfunction has been reported in 1-17% of patients.5-8,11 Adverse events that may lead to discontinuation are most likely to occur within the first 3 months of treatment.5,6,8 The severity of adverse events tends to decrease over time, suggesting that patients develop a tolerance to them.6,8,10 In contrast, we found a much higher incidence of adverse events (80%) even after 6 months of treatment. Although most of the adverse events were mild or moderate, the incidence of cognitive dysfunction such as memory loss (35%) and attention deficit (27%) was high. Compared to adverse events of short-term treatment, the frequency of CNS symptoms such as somnolence, headache, dizziness, and fatigue decreased during long-term treatment. However, the frequency of cognitive dysfunction decreased less. These observations may indicate that cognitive dysfunction induced by ZNS treatment will not be tolerated over a longer period.
There are several possible reasons for the discrepancies in the frequencies of cognitive complaints between our study and previous studies. First, the dosage requirements and the potential for toxic reactions to psychotropic medication might differ between racial and ethnic groups.21 However, since the frequency of cognitive dysfunction in many Japanese studies was much lower than that of our study, it is impossible to deduce that the cognitive impairment is solely due to ethnic variations. Second, ZNS patients in previous trials may have had poor awareness of their cognitive dysfunction and they may not have reported these problems spontaneously. The lack of awareness of a cognitive deficit might be influenced by personality factors, perhaps augmented by the stress involved in a chronic condition.22 Therefore, specific questioning about cognitive problems and brief cognitive testing during clinic visits by patients may be particularly important when managing patients receiving AEDs. Third, psychosocial factors such as depression or anxiety may affect epilepsy patients, and mood disorders are known to independently compromise the integrity of memory processing.23 Furthermore, epilepsy patients who have mood disorders tend to overstate memory problems.22 Although the incidence of mood complaints was trivial in our study, both events may increase cognitive complaints.
In conclusion, long-term ZNS monotherapy is effective at treating a broad spectrum of seizure disorders, except complex partial seizures. However, a specific adverse event, such as cognitive impairment, is common and long-lasting. Cognitive effects are only one factor in AED selection, with it being possible that the risks of cognitive dysfunction are outweighed by the potential for seizure control and overall improvement in the quality of life in particular patients. Even though our patients showed cognitive dysfunction associated with ZNS, they continued to take the medicine due to its efficacy. However, the ultimate goal for epilepsy treatment is to choose the AED that best controls the patient's seizures with the fewest side effects. Cognitive function exerts important effects on the quality of life in younger patients who are more affected by academic or occupational functioning. Therefore, further objective studies such as neuropsychological or neuroimaging investigations are needed to clarify the effect of ZNS on cognition. Moreover, the optimal target dose of ZNS monotherapy should be determined to minimize dose-related adverse events.
Figures and Tables
Figure 1
Efficacy of zonisamide monotherapy. The percentage reduction in seizure frequency from baseline to the end of the treatment period was measured in 60 patients. Seizure freedom occurred in 45% of patients, and the reduction of seizure frequency by ≥ 50% was observed in 78% of patients.

References
1. Masuda Y, Ishizaki M, Shimizu M. Zonisamide: pharmacology and clinical efficacy in epilepsy. CNS Drug Rev. 1998. 4:341–360.

3. Oommen KJ, Mathews S. Zonisamide: a new antiepileptic drug. Clin Neuropharmacol. 1999. 22:192–200.
4. Leppik IE, Willmore LJ, Homan RW, Fromm G, Oommen KJ, Penry JK, et al. Efficacy and safety of zonisamide: results of a multicenter study. Epilepsy Res. 1993. 14:165–173.

5. Tosches WA, Tisdell J. Long-term efficacy and safety of monotherapy and adjunctive therapy with zonisamide. Epilepsy Behav. 2006. 8:522–526.

6. Ohtahara S, Yamatogi Y. Erratum to "Safety of zonisamide therapy: prospective follow-up survey". Seizure. 2007. 16:87–93.

7. Wilfong AA. Zonisamide monotherapy for epilepsy in children and young adults. Pediatr Neurol. 2005. 32:77–80.

8. Kothare SV, Kaleyias J, Mostofi N, Valencia I, Melvin JJ, Hobdell E, et al. Efficacy and safety of zonisamide monotherapy in a cohort of children with epilepsy. Pediatr Neurol. 2006. 34:351–354.

9. Brodie MJ. Zonisamide as adjunctive therapy for refractory partial seizures. Epilepsy Res. 2006. 68:Suppl 2. S11–S16.

10. Leppik IE. Practical prescribing and long-term efficacy and safety of zonisamide. Epilepsy Res. 2006. 68:Suppl 2. S17–S24.

11. Newmark ME, Dubinsky S. Zonisamide monotherapy in a multi-group clinic. Seizure. 2004. 13:223–225.

12. Fukushima K, Seino M. A long-term follow-up of zonisamide monotherapy. Epilepsia. 2006. 47:1860–1864.

13. Lee KS, Ahn JH, Kim BS, Kang MS, Chung SW, Kim YI, et al. The effect of zonisamide in epileptic patients. J Korean Neurol Assoc. 1991. 9:220–227.
14. Lee SY. The antiepileptic effect of zonisamide (P-132). New Med J. 1991. 34:79–84.
15. Chang HI, Yoon DJ, Oh DJ, Song JY, Lim OG, Lee KK, et al. A clinical study on the antiepileptic effect of zonisamide. J Korean Neuropsychiatr Assoc. 1992. 31:778–784.
16. Kim KJ, Chae SA, Ko TS, Kim DW, Hwang YS. The effect of zonisamide in children with refractory epilepsies. Korean J Pediatr. 1993. 36:1139–1145.
17. Cho KH, Kim YS, Sin KC, Son JH, Kim BC, Kim MK, et al. The antiepileptic effect and safety of zonisamide in patients with intractable seizure. New Med J. 1994. 37:89–95.
18. Korean Zonisamide Study Group (KZSG). Double-blind, randomized, comparative clinical trial of zonisamide and carbamazepine as initial monotherapy in newly diagnosed epilepsy. J Korean Epilep Soc. 1999. 3:50–57.
19. Mattson RH, Cramer JA, Collins JF. Prognosis for total control of complex partial and secondarily generalized tonic clonic seizures. Department of Veterans Affairs Epilepsy Cooperative Studies No. 118 and No. 264 Group. Neurology. 1996. 47:68–76.

20. Kothare SV, Valencia I, Khurana DS, Hardison H, Melvin JJ, Legido A. Efficacy and tolerability of zonisamide in juvenile myoclonic epilepsy. Epileptic Disord. 2004. 6:267–270.
21. Lin KM, Poland RE, Lesser IM. Ethnicity and psychopharmacology. Cult Med Psychiatry. 1986. 10:151–165.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download