Abstract
Background and Purpose
The closing-in phenomenon is the tendency to draw near or on the target when copying figures, which has been found mostly in patients with Alzheimer's disease (AD). We attempted to quantify the degree of closing-in and to compare it between patients with AD and vascular dementia (VaD).
Methods
The subjects (55 AD, 39 VaD and 38 normal controls) were asked to copy the figure of alternating square and triangle, starting at the designated point and continuing from left to right. The patients with AD and VaD did not differ in age, education, severity of dementia or Rey Complex Figure Test copy score. The proximity (Y-axis) of the subject's drawing to the target was plotted at intervals of 2 mm along the X-axis and the degree of closing-in was computed from the slope of the regression line.
Results
The AD and VaD patients showed a steeper slope than the controls. There was no significant difference, however, in the magnitude of closing-in of the AD and VaD patients. When closing-in was defined as a slope that was greater than the mean+2SD of the slope observed for the controls, 32.7% of the AD and 25.6% of the VaD patients showed closing-in.
The closing-in phenomenon refers to a condition in which subjects draw near or on the figure that is to be copied.1 Since Mayer Gross first described this phenomenon,2 many studies reported that closing-in occurs both in patients with various brain injuries and in normal children.3-6 The frequency of closing-in is higher in patients with diffuse brain damage than in patients with focal brain lesions.6 More recent studies of closing-in have been focused on dementia patients.1,7-9
Gainotti et al. compared the frequency of closing-in between patients with Alzheimer's disease (AD) and those with vascular dementia (VaD).1,7 Since the frequency of closing-in of AD was higher than that of VaD in their studies, they postulated that closing-in might be one of the neuropsychological characteristics of AD. Another study on closing-in in AD described three subtypes of closing-in: 1) the overlap type in which subjects draw on the target figures, 2) the adherent type in which subjects draw very close to the target but without overlapping, and 3) the near type, a milder form of the adherent type.10 These authors also investigated the eye movement patterns associated with closing-in and reported that different eye movement patterns are observed according to the subtype of closing-in. Since Chin et al first described a novel method of closing-in quantification using the Luria's Alternating Square and Triangle,11 Kwak performed a closing-in study using the Luria's alternating square and triangle and reported that AD patients exhibited higher occurrence of closing-in compared to subcortical vascular dementia (SVD) patients.8
Prior studies of closing-in involving dementia patients may have some limitations. Firstly, the presence of closing-in and the associated subtype were determined simply by visual inspection without quantification, except Kwak's research. Furthermore, many studies did not use normal controls. Secondly, since the degree of closing-in reflects the proximity of the subject's drawing to the target, it is likely to depend on the distance between the target and the space (working space) in which the subject is allowed to draw. However, all prior studies did not specify the starting point or the working space to use for copying. Thirdly, closing-in may vary as a function of time. For instance, as the subject is drawing, the degree of closing-in may increase over time. In order to investigate this time effect, we thought that it would be better for the target figure to be a continuous line drawing rather than the collection of individual objects used in previous studies.
The aims of this study thus were 1) to present a method of quantifying the degree of closing-in that can overcome the limitations described above and 2) using this method to compare the frequency of closing-in in patients with AD and VaD.
The subjects in this study were 64 patients with AD (age: 71.8±9.0 years, male: 13 patients, education: 7.9±4.7 years), 52 patients with VaD (age: 72.5±8.5 years, men: 22 patients, education: 7.9±5.3 years), and 38 normal controls (age: 68.0±7.2 years, male: 19 subjects, education: 9.7±4.4 years). Ninety-five of the 116 (62 with AD and 33 with VaD) patients were consecutively recruited from the Memory Disorder Clinic of Samsung Medical Center, Seoul Korea, between March 2001 and October 2001 and the remaining 21 patients were recruited from the inpatient department of Yong-in Geriatric Hospital as of July 19, 2001. The patients with AD met the probable AD criteria proposed by the National Institute of Neurological and Communicative Disorders and Stroke / Alzheimer's Disease and Related Disorders Association.12 The patients with VaD fulfilled the probable VaD criteria of the Alzheimer's Disease Diagnostic and Treatment Centers.13 One neurologist blinded to the clinical information performed visual analysis of cerebral ischemia in MRI or CT scans. All but six patients with AD and all the patients with VD were imaged with MRI and the remaining six patients with AD were imaged with CT. Ischemia in MRI was measured by the scale of Fazekas et al.,14 which provides two different scores (periventricular and deep white matter score) each rated on a 4-point scale. Ischemia in CT scan was rated by the scale of Blennow et al.,15 which measures both extent and severity of white matter lesions (WMLs) each on a 4-point rating scale. In AD patients, mean ischemic score in MRI for periventricular hyperintensity was 1.56±0.97, and the mean ischemic score for deep white matter hyperintensity was 1.51±1.7. Ischemia on CT scan was also negligible with the extent of white matter lesion rated as 0.5±0.8 and the severity of white matter lesion rated as 0.5±0.8. In VD patients, mean ischemic score in MRI for periventricular hyperintensity was 2.67±0.61, and the mean ischemic score for deep white matter hyperintensity was 2.73±0.58.
Normal controls with no previous neurologic or psychiatric diseases were recruited from among the spouses or caregivers of the outpatients of Samsung Medical Center during the same period in which the patients were recruited. Both the patients and the controls were right-handed, as assessed by the Edinburgh Handedness Inventory.16 Subjects who were illiterate were excluded from the study.
The target figure to be copied was a modified Luria's alternating square & triangle.17 As presented in Fig 1, the stimulus consisted of 12 units (6 squares and 6 triangles) that appeared in an alternating sequence, except in two places: in one place the triangles appeared contiguously, while in the other, the squares did. The size of each unit was 10×10 mm and the connecting line between each pair of units was 5 mm long. The whole figure was 185 mm long and was drawn with a solid line that was 1 mm thick. The stimulus was printed in black on an A4 size white sheet of paper (297×211 mm), with its longer axis parallel to the longer axis of the paper. The left end of the stimulus was situated 60 mm from the top and 55 mm from the left-hand edge of the paper. There were 3 types of target figure (Fig.1 (A), (B), (C)) and each subject performed one trial of copy per figure. The order of the three trials was random.
The subjects were seated in front of a table and the paper was fixed to the table with its longer axis parallel to the subject's coronal axis. The midpoint of the stimulus was approximately aligned with the midsagittal plane of subject's body and head. The distance from the subject's eyes to the stimulus was about 60 mm, and the subjects were asked to limit the movement of their trunk as much as possible, but that head and eye movements were allowed. The subjects were instructed to copy the target figure starting from the designated point and to proceed from left to right parallel to the stimulus using a pen held in their right hand. The starting point (1 mm in diameter) for the copy was 50 mm from the top along the left end of the stimulus.
A psychometrician, who was blinded to the clinical information concerning the subjects, quantified the degree of the closing-in phenomenon. As presented in Fig 2-B, a grid with dimensions of 2×2 mm was superimposed on the target and the subject's drawing, so that the baseline (connecting line between units) of the target figure was parallel to the horizontal lines of the grid. For each 2 mm interval along the X-axis, the value of the Y-coordinate was obtained. The X- and Y-coordinates of the starting point of the subject's drawing was designated as (0,0). In some patients, several Y-values were recorded for a given X-coordinate, because the drawing was distorted due to visuoconstructive impairment. In such cases, the last Y-value in the direction of the drawing was selected. As illustrated in Fig. 1-C, for each subject, the Y-values were plotted against the X-values at 2 mm intervals. Then, the regression line was obtained by means of a simple regression analysis using SPSS 10.0 for Windows. The unstandardized regression coefficient (b), i.e. the slope of the regression line, was taken as the measure of the severity of closing-in: a positive value denoted that the subject closed in, whereas a negative value denoted that the subject drew away from the target as the copying proceeded. Each subject performed three trials, one for each of the 3 types of target figures, and the mean of these three trials represented each subject's closing-in value.
Previous studies used single objects for copying rather than a continuous figure. In order to compare the degree of closing-in that appeared while copying the RCFT (single object) with that which appeared on the Luria's alternating square and triangle (continuous figure) task, two neurologists who were blinded to the results of Luria's figure visually judged whether any closing-in occurred while copying the RCFT and formed a consensus.
Nine of the 64 patients with AD were excluded from the analysis, because our closing-in measurement was inapplicable for the following reasons. 1) Three patients showed severe distortion in their drawings, as presented in Fig 3-A. 2) Two patients became stuck at the starting point and could not proceed rightward. 3) Three patients refused the test and did not complete the three trials. 4) The remaining one patient could not understand the test instructions. All of these excluded patients belonged to CDR 2 or 3 (2.4±0.6).
Likewise, 13 of the 52 patients with VaD were excluded for the following reasons. 1) Eight patients showed severe distortion in their drawings, as presented in Fig. 3-B. 2) Five patients refused the test and did not complete the three trials. These excluded patients also had severe dementia (CDR: 2.2±0.7).
After excluding those patients for whom our closing-in measurement was inadequate, the final sample consisted of 55 patients with AD, 39 patients with VaD, and 38 normal controls. The demographic characteristics and scores of the RCFT of all subjects and the general cognitive indices of the patients are presented in Table 1. There was no significant difference in age [F(2,129)= 2.350, p=.099] or education [F(2,129)=1.032, p=.359] among the three groups, as determined by the General Lineal Model (GLM). However, the ratio of women to men in the AD patients was higher than that in the other two groups (X2=10.306, p=.006). A comparison of the AD with the VaD patients using the independent t-test showed no significant differences in the MMSE (t=-1.457, p=.148), CDR (t=1.185, p=.273), or RCFT copy (t=1.103, p=.273) scores.
The mean regression coefficient (b) of the normal controls was 0.059±0.024. This coefficient significantly differed from zero, suggesting that even the normal controls copied slightly toward the target stimuli (t=14.979, p<.001). Using multiple regression analysis, we confirmed that age and education did not significantly influence the closing-in tendency (b) in the normal controls.
The mean regression coefficient (b) of the AD patients was 0.096±0.062 and that of the VaD patients was 0.088±0.074. A GLM analysis showed that there was a significant difference in the mean regression coefficient (b) among the control and the two patient groups [F(2,129)=4.846, p=.009]. Post hoc analysis showed that the slopes of the regression lines of the AD and VaD patients were steeper than those of the normal subjects (AD vs. controls: t =-3.527, p=.001; VaD vs. controls: t=-2.350, p=.021). However, no difference was noted between the slopes of the AD and VaD patients (t=.541, p=.590).
The presence of the closing-in phenomenon for an individual patient was defined as an unstandardized regression coefficient (b) greater than mean+2SD of the controls (b>0.107). Using this criterion, we identified 18 patients (32.7%) with closing-in out of the 55 AD patients, while 10 of the 39 (25.6%) VaD patients were considered to have closing-in. A chi-square analysis showed that there was no significant difference in these frequencies (X2=.548, p=.459). In addition, there was no significant difference in the mean regression coefficient (b) between the AD and VaD patients who were considered to have closing-in phenomenon (t=-.782, p=.441).
To evaluate the validity of our method of quantifying the degree of closing-in, we measured the agreement of the closing-in phenomenon that appeared while copying the RCFT (single object) with that which appeared on the Luria's alternating square and triangle (continuous figure) task. The kappa value was .303, and was statistically significant (p=.001).
To investigate whether the degree of closing-in increases as the severity of dementia increases, the MMSE and CDR scores were compared with the degree of closing-in. The results showed that the slope of the line was not correlated with either the MMSE or CDR scores. However, there was a significant correlation between the degree of closing-in and the score of the RCFT copy task (r=.-259, p=.021).
We asked the patients with dementia and the normal controls to copy a continuous figure (Luria's alternating square and triangle) and observed a general tendency that the subjects' drawing approached the target as the copying proceeded from left to right. The extent of this approach was quantified by the slope of the regression line that best represented the proximity of the subject's drawing to the target as a function of the distance from the starting point. Unlike prior methods, our method allows quantification of closing-in by which we can objectively measure the frequency and severity of closing-in. Kwak attempted a similar method but the starting point for the copying was not controlled and the closing-in was simply classified into the three types (near, adherent and overlap types) according to the proximity of subjects' drawing to the target model.8 To investigate the concurrent validity of our quantification method, the frequency of closing-in measured by our method was compared with that measured by the conventional method, i.e., the frequency of closing-in on copying the single object (the Rey-Osterrieth figure). The results showed that there was a significant correlation between the two methods. Furthermore, the degree of closing-in was significantly greater in the dementia patients than in the controls.
It is difficult to determine whether or not there is closing-in when the degree of closing-in is mild. However, our quantification method allows us to detect mild or subtle closing-in. In other words, of the three subtypes of closing-in proposed by Midorikawa et al,10 our regression line analysis is more appropriate for detecting the 'near type' of closing-in compared with the conventional visual analysis. In contrast, our method may be less adequate for quantifying the severe types of closing-in, i.e., the adherent and overlap types.
Regarding the severity of closing-in, the average slope of the regression line in AD patients was 0.096, which represents an approach of approximately 9.6 mm toward the target by the time the copying had proceeded 10 cm from the starting point. Likewise, the patients with VaD made an approach of 8.8 mm toward the target by the time they had copied 10 cm beginning from the starting point. Even the normal subjects closed in as the copying proceeded (5.9 mm approach). Based on the performances of the controls, we defined the presence of closing-in in individual patients as a slope that was more than the mean+2SD of the controls. The cutoff score was 0.107 that means there was an approach of 10 mm when 10 cm of copying had been made.
When the AD and VaD groups were compared, although the slope of the regression line in AD was steeper than that of VaD, these two groups did not differ statistically in terms of the severity of closing-in. No group difference was noted in the frequency of closing-in, either (32.7% in AD, 25.6% in VaD). This finding is inconsistent with those of previous studies conducted by Gainotti et al1,7 and Kwak.8 Gainotti et al compared the frequency of closing-in between patients with Alzheimer's disease (AD) and those with vascular dementia (VaD).1 The two groups (41 patients with AD and 34 patients with VaD) were matched in terms of dementia severity and visuospatial dysfunction. The patients performed two types of task: in one task, the subjects copied figures such as a star, cube or house in a conventional way, while in the other task, the subjects were requested to copy modified figures that were partly drawn with the landmarks. When the subjects showed closing-in in the former task, it was referred to as "classical" closing-in, whereas the closing-in that occurred in the latter task was called "variant" closing-in. The results showed that the frequency of classical closing-in was 24% in AD and 6% in VaD. The frequency of variant closing-in was much higher, with 61% of AD patients and 29% of VaD patients showing this form of closing-in. More recently, Gainotti et al. conducted a new study with dementia patients and reported that 15 out of 49 (30%) AD patients and 3 out of 43 (7%) VaD patients showed closing-in.7
This discrepancy between our study and previous studies1,7,8 may be related to the difference in the severity of dementia between our subjects and those of the studies by conducted by Gainotti et al7 and Kwak.8 Specifically, although a direct comparison is impossible, subjects of Gainotti's study had "mild to moderate" dementia, possibly corresponding to CDR 1 or 2. In comparison, our subjects mainly belonged to CDR 0.5 or 1. In our study, many of the patients with CDR 2 or 3, who presented severe visuoconstructive dysfunction or closing-in, were excluded from the analysis. In the Kwak's study, MMSE score of the AD patient (M=14.58) was lower than that of our patient (M=16.55). An alternative explanation for the discrepancy may be the difference in VaD criteria among studies. Gainotti et al. did not specify which criteria they used and Kwak enrolled patients with SVD according to the criteria outlined by Erkinjuntti.20 Our study recruited only patients with dementia from small vessel disease using the ADDTC criteria.
Previous studies reported that the frequency of the closing-in phenomenon increases as the severity of dementia increases.5,6 Given that our method is relatively sensitive for mild closing-in, whereas the conventional visual inspection method is more adequate for severe closing-in, it is thought that the frequency of mild closing-in may not differ between AD and VaD in their early stage, but that severe closing-in may be greater in AD than in VaD in advanced stages of dementia. Although, in our study, the degree of closing-in was not correlated with the severity of dementia as measured by CDR and MMSE, this also may be attributable to our method of selecting patients.
The mechanisms underlying the closing-in phenomenon have not been fully explained. Mayer-Gross postulated that closing-in is a part of constructional apraxia, as a consequence of the "fear of empty space".2 Muncie suggested that closing-in occurs as a result of "the inability to make an abstract copy through the symbolization from a concrete model".3 Ajuriaguerra et al. viewed closing-in as a form of magnetic reaction similar to primitive behaviors such as grasping, sucking, echolalia, or echopraxia.5 However, Lee et al. posited that closing-in might be related to the patients' compensatory strategies to overcome visuospatial dysfunction or visuospatial working memory deficit.9 In their research, the magnitude of closing-in increased as a function of figure complexity, however closing-in was unchanged by varying the distance from the target to the copying space. They interpreted this results that copying near the target figure is not the re-emergence of a primitive magnetic reaction pattern, but the patients' strategy to compensate for their visuospatial dysfunction or visuospatial working memory deficits. In our research, even though those patients with severe visuoconstructive dysfunction were excluded, our quantification of closing-in correlated with the scores of the RCFT copy, suggesting that closing-in is closely associated with visuoconstructive ability.
In the current study, we presented a method of quantifying the degree of closing-in phenomenon using the statistical analysis. This method is useful for determining the presence of mild closing-in phenomenon. But the anatomical localization of this phenomenon is not yet certain. Thus, the future study has to elucidate the neuronal substrate of the closing-in phenomenon using this method. One limitation of our study is that VaD patients participated in our study may not be a homogeneous group. The ADDTC criteria for VaD does not exclude the patients with AD. Thus, AD patients with ischemic changes might have been included in our VaD patients.
Figures and Tables
Figure 1
The target figure stimuli used for the figure copying tasks were the modified Luria's alternating square and triangles. (A) Stimulus 1. (B) Stimulus 2. (C) Stimulus 3.
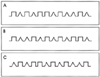
Figure 2
(A) An illustrative case which shows the closing-in phenomenon. (B) and (C) Our quantification method for closing-in. (B) A 2×2 mm grid was superimposed on the patient's drawing illustrated in (A) and Y values were obtained at intervals of 2 mm along the X-axis. (C) With these X- and Y-values, the slope of the regression line was calculated, which represents the severity of closing-in.

References
1. Gainotti G, Parlato V, Monteleone D, Carlomagno S. Neuropsychological markers of dementia on visual-spatial tasks: a comparison between Alzheimer's type and vascular forms of dementia. J Clin Exp Neuropsychol. 1992. 14:239–252.

3. Muncie W. Concrete model and abstract copy: a psychobiological interpretation of the "closing-in" symptom of Mayer-Gross. J Nerv Ment Dis. 1938. 88:1–11.
4. Lhermitte J, Mouzon J. Sur l'apractognosie geometrique et l'apraxie constructive consecutives aux lesions du lobe occipital. Rev Neuol. 1941. 73:415–431.
5. Ajuriaguerra J, De Muller M, Tissot R. A propos de quelques problemes poses par l'apraxie dans les demences. Encephale. 1960. 49:275–401.
6. Gainotti G. A quantitative study of the "closing-in" symptom in normal children and in brain-damaged patients. Neuropsychologia. 1972. 10:429–436.

7. Gainotti G, Marra C, Villa G, Parlato V, Chiarotti F. Sensitivity and specificity of some neuropsychological markers of Alzheimer dementia. Alzheimer Dis Assoc Disord. 1998. 12:152–162.

8. Kwak YT. "Closing-in" phenomenon in Alzheimer's disease and subcortical vascular dementia. BMC Neurology. 2004. 4:3.

9. Lee BH, Chin J, Kang SJ, Kim EJ, Park KC, Na DL. Mechanism of the Closing-in phenomenon in a figure copying task in Alzheimer's disease. Neurocase. 2004. 10(5):393–397.

10. Midorikawa Y, Fukatsu R, Takahata N. Closing-in phenomena observed in patients with Alzheimer's disease - analysis of drawing behavior and eye movements. Seishin Shinkeigaku Zasshi. 1996. 98:151–169.
11. Chin J, Baek MJ, Lee BH, Kang SJ, Jeong Y, Kwon J. The closing-in phenomenon in Alzheimer's disease and vascular dementia. J Int Neuropsychol Soc. 2003. 9:166.

12. Mckhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA work group under the auspices of department of health and human services task force on Alzheimer's disease. Neurology. 1984. 34:939–944.

13. Chui HC, Victoroff JI, Margolin D, Jagust W, Shankle R, Katzan R. Criteria for the diagnosis of ischemic vascular dementia proposed by the state of California Alzheimer's Disease Diagnostic and Treatment Centers. Neurology. 1992. 42:473–480.

14. Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimenr's dementia and normal aging. AJNR Am J Neuroradiol. 1987. 8:421–426.
15. Blennow K, Wallin A, Uhlemann C, Gottifries CG. White-matter lesions on CT in Alzheimer's patients: relation to clinical symptomatologic and vascular factors. Acta Neurol Scand. 1991. 83:187–193.

16. Oldfield RC. The assessment and analysis of handedness: The Edinburgh Inventory. Neuropsychologia. 1971. 9:97–113.

17. Luria A. Human brain and psychological processes. 1966. New York: Harper & Row.
18. Kang YW, Na DL, Hahn SH. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997. 15:300–308.
19. Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993. 43:2412–2414.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download