Abstract
Achromobacter xylosoxidans can cause various types of infections, but its infection in humans is rare. A. xylosoxidans has been reported as a rare etiological agent of infections including primary bacteremia, catheter-related bloodstream infection, endocarditis, otitis, and pneumonia, particularly in immunocompromised hosts. We encountered a case of septic shock caused by A. xylosoxidans in a 52-year-old, immunocompetent woman with no underlying disease, who received extracorporeal shock wave lithotripsy to remove a left upper ureteral stone. She was treated with antibiotics to which the organism was susceptible but died as a result of septic shock.
Achromobacter xylosoxidans, formerly called Alcaligenes xylosoxidans, is an aerobic, non-fermenting, gram-negative bacilli with low virulence. It was first seen in 1971 by Yabuuchi and Ohyama in a patient with chronic, inflammatory otitis media [1]. Due to its ability to easily oxidize xylose, it has been named xylosoxidans. It is primarily found in contaminated soil or water, but it is rare in humans. It is known to infect immunosuppressed patients, including those with tumors, blood diseases, hypogammaglobulinemia, or acquired immune deficiency syndrome (AIDS), or those who have undergone organ transplant [2]. The authors experienced a case of septic shock caused by A. xylosoxidans in an immunocompetent woman with no underlying disease who received extracorporeal shock wave lithotripsy (ESWL). We report this case with a literature review.
A 52-year-old female patient was admitted to the hospital with colicky, left flank pain. The patient had no medical history of chronic or immunodeficiency diseases, nor any previous history of urolithiasis or urinary tract infections. On admission, vital signs were stable; blood pressure was 110/70 mmHg, respiratory rate was 20/min, pulse rate was 69/min, and temperature was 37.0℃. The patient complained of left flank pain without other urinary symptoms. Left costovertebral angle tenderness was noted upon physical examination. A complete blood cell count showed white blood cells (WBCs) were 9,970/mm3 (neutrophils, 84.4%; lymphocytes, 6.4%), hemoglobin was 10.6 g/dL, and platelet count was 142,000/mm3. The C-reactive protein (CRP) was 57.5 mg/dL. Biochemical tests showed blood urea nitrogen (BUN) was 19 mg/dL, creatinine was 0.8 mg/dL, total protein was 6.5 g/dL, albumin was 3.2 g/dL, total bilirubin was 2.2 mg/dL, aspartate aminotransferase was 34 IU/L, and alanine aminotransferase was 47 IU/L. There were no WBCs in the urinalysis, but red blood cells were over 100 per high-power field (RBC/HPF). Cultures were not done at the time of admission. The cause of pain was a urinary stone in the left ureter, noted through ultrasound. On the 3rd and 4th days after admission, the patient underwent ESWL, receiving a total of 8,000 shocks. The ESWL aggravated the flank pain and costovertebral angle tenderness. Three days later, the patient's body temperature rose to 39.9℃.
On the 7th day, her blood pressure fell to 70/50 mmHg, heart rate was 125/min, respiratory rate was 26/min, and body temperature was 39.0℃. Oxygen saturation was 80% on room air. The patient was moved to the intensive care unit and started on mechanical ventilation and shock management. WBCs were 18,400/mm3 (neutrophils, 90.4%; lymphocytes, 5.5%), hemoglobin was 11 g/dL, platelet count was 92,000/mm3, and CRP was 240 mg/dL. BUN was 56 mg/dL; creatinine was 2.4 mg/dL. Cefepime (2 g intravenously every 12 hours) and vancomycin (1 g intravenously every 24 hours) were administered empirically. Computed tomography showed a 4 mm left proximal ureter stone and hydroureteronephrosis. There were no WBCs or RBCs in the urine. The urine cultures were negative but two sets of blood cultures were positive for gram-negative bacilli, which was identified as Achromobacter xylosoxidans (BACTEC™ Plus Aerobic/F Culture Vials; Becton Dickinson and Company, Franklin Lakes, New Jersey, United States). The minimum inhibitory concentrations µg/mL) (BACTEC FX; Becton Dickinson and Company) were as follows: imipenem/cilastatin, 4; meropenem, 4; piperacillin-tazobactam, 8; ampicillin, 16; ciprofloxacin, 2; amikacin, 32; aztreonam, 16; and cefepime, 16. A. xylosoxidans was resistant to cefepime; hence, antibiotics were changed to imipenem (500 mg intravenously every 12 hours). On the 14th day, blood cultures no longer revealed A. xylosoxidans , but the patient's renal function worsened, requiring continuous renal replacement therapy. Burkholderia cepacia was isolated from one set of blood cultures on the 16th day; it was susceptible to imipenem/cilastatin. We removed the central venous catheter to culture for B. cepacia that might have infected the catheter. A tip culture and repeated blood cultures were negative after three days. On the 21st day, the patient had respiratory failure with bilateral opacities on chest imaging. On the 29th day after admission, she passed away from septic shock and multiple organ failure.
16S rRNA sequencing identified the isolate. Primers of 515FPL (TGCCAGCAGCCGCGGTAA) and 13B (AGGCCCGGGAACGTATTCAC) were used for 16S rRNA gene amplification. Sequencing was carried out using Taq polymerase (Solgent, Daejeon, Korea). The resulting sequence was compared with sequences stored in the GenBank (http://www.ncbi.nlm.nih.gov/genbank). It was identified as A. xylosoxidans, with 100% sequence identity.
A. xylosoxidans is an aerobic, non-fermenting, gram-negative bacilli with low virulence [3]. Infections occur mostly in immunocompromised patients, including those with tumors, blood diseases, hypogammaglobulinemia, AIDS, diabetes, or late-stage kidney failure, and those who have undergone organ transplants [4]. For cases that progress to bacteremia, it is most often because of an intravenous catheter infection [5]. Patients with blood diseases or tumors have high mortality rates with this infection [5]. Clinical cases of bacteremia caused by A. xylosoxidans are summarized in Table 1. A total 224 cases of bacteremia were reported: 74 in neonates and 150 in adults [467891011121314]. The most common cause was catheter- related infection (78 cases, 52% in adults) [468101112131415]. Pneumonia was the second most common source (12 cases, 8% in adults) [4689101112131415].
A. xylosoxidans typically causes otitis media, skin infections, intravenous catheter infections, and surgical-site infections [2]. Urinary tract infections were observed only occasionally and the prevalence was unknown. The frequency of urinary tract infection by A. xylosoxidans was 0.04% (proportion of positive urine cultures) in a medical center in Spain [5]. Urinary tract infection due to A. xylosoxidans often develops from the pathogenic bacteria traveling from the intestines to the ureters and bladder. While it has been reported that A. xylosoxidans causes infections in immunocompromised patients and those with urological abnormalities [2], the patient in this case had no such tendencies. It has also been reported that most of these infections occur as nosocomial infections. The patient in this case had a negative blood culture, but the strains were cultured after the symptoms occurred.
According to existing reports, A. xylosoxidans has a high resistance against antibiotics, making treatment difficult. It is sensitive to imipenem, piperacillin-tazobactam, ceftazidime, and trimethoprim-sulfamethoxazole. Resistance was found in second- or third-generation cephalosporins except ceftazidime and fluoroquinolones [8]. In this case, it was sensitive to imipenem, meropenem, trimethoprim-sulfamethoxazole, piperacillin-tazobactam, and ceftazidime, and resistant to ampicillin, ciprofloxacin, amikacin, cefotetan, ceftriaxone, aztreonam, and cefepime, showing similar results to existing reports. Presently, carbapenem, antipseudomonal penicillins, and trimethoprim-sulfamethoxazole are effective treatments [6]. Attempts have been made to combine two or more drugs for treatment, such as by combining gentamicin with piperacillin, doxycycline with azithromycin, or trimethoprim-sulfamethoxazole with azithromycin. These combinations have been effective in reducing resistance and increasing the efficacy of treatment [81516].
In conclusion, A. xylosoxidans can cause infection in immunocompromised patients, while infection in immunocompetent hosts is rare. However, we have observed such a case in a patient who had normal immune function, and report the findings of this case along with a literature review.
Figures and Tables
Table 1
Clinical cases of bacteremia caused by Achromobacter xylosoxidans
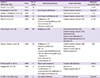
| Authors (Reference No.) | Date | No. of cases | Underlying disease | Source of isolate | Outcome (mortality rate) |
|---|---|---|---|---|---|
| Turel O, et al. [13] | 2013 | 22 | Septicemia in neonate | 13.6% | |
| Turqutalp K, et al. [14] | 2011 | 1 | End-stage renal disease | Central venous catheter | Expired |
| Molina-Cabrillana J, et al. [10] | 2007 | 52 | Septicemia in neonate | 7.7% | |
| Tena D, et al. [12] | 2005 | 4 | End-stage renal disease (4) | Central venous catheter (4) | Cured |
| Shie SS, et al. [11] | 2005 | 40 |
Malignancy (23) Chronic renal insufficiency (9) Liver cirrhosis (6) Diabetes mellitus (6) |
Central venous catheter (22) | 47.5% |
| Aisenberg G, et al. [6] | 2004 | 46 | Malignancy (46) |
Primary bacteremia (10) Central venous catheter (13) Pneumonia (6) Urinary tract infection (5) Mucocutaneous infection (3) Sinusitis (1) |
15% |
| Gómez-Cerezo J, et al. [9] | 2003 | 54 |
Malignancy (21) Diabetes mellitus (6) HIV (6) Chronic renal insufficiency (6) Chronic obstructive pulmonary disease (3) Liver cirrhosis (2) Cystic fibrosis (1) |
Central venous catheter (28) Pneumonia (6) Surgical wound site (4) Undetermined (9) |
15% |
| Weitkamp JH, et al. [4] | 2000 | 1 | Hyper-IgM syndrome | Lymph node infection | Cured |
| Duggan JM, et al. [8] | 1996 | 4 |
No medical history (1) Cerebral palsy (1) Acute lymphocytic leukemia (1) End stage renal disease (1) |
Sputum (1) Central venous line (3) |
25% |
| Lee JH, et al. [This case] | 2014 | 1 | No medical History | Primary bacteremia | Expired |
References
1. Yabuuchi E, Oyama A. Achromobacter xylosoxidans n. sp. from human ear discharge. Jpn J Microbiol. 1971; 15:477–481.
2. Mandell WF, Garvey GJ, Neu HC. Achromobacter xylosoxidans bacteremia. Rev Infect Dis. 1987; 9:1001–1005.
3. Eshwara VK, Mukhopadhyay C, Mohan S, Prakash R, Pai G. Two unique presentations of Achromobacter xylosoxidans infections in clinical settings. J Infect Dev Ctries. 2011; 5:138–141.

4. Weitkamp JH, Tang YW, Haas DW, Midha NK, Crowe JE Jr. Recurrent Achromobacter xylosoxidans bacteremia associated with persistent lymph node infection in a patient with hyper-immunoglobulin M syndrome. Clin Infect Dis. 2000; 31:1183–1187.

5. Tena D, González-Praetorius A, Pérez-Balsalobre M, Sancho O, Bisquert J. Urinary tract infection due to Achromobacter xylosoxidans: report of 9 cases. Scand J Infect Dis. 2008; 40:84–87.

6. Aisenberg G, Rolston KV, Safdar A. Bacteremia caused by Achromobacter and Alcaligenes species in 46 patients with cancer (1989-2003). Cancer. 2004; 101:2134–2140.

7. Amoureux L, Bador J, Siebor E, Taillefumier N, Fanton A, Neuwirth C. Epidemiology and resistance of Achromobacter xylosoxidans from cystic fibrosis patients in Dijon, Burgundy: first French data. J Cyst Fibros. 2013; 12:170–176.

8. Duggan JM, Goldstein SJ, Chenoweth CE, Kauffman CA, Bradley SF. Achromobacter xylosoxidans bacteremia: report of four cases and review of the literature. Clin Infect Dis. 1996; 23:569–576.

9. Gómez-Cerezo J, Suárez I, Ríos JJ, Peña P, García de Miguel MJ, de José M, Monteagudo O, Linares P, Barbado-Cano A, Vázquez JJ. Achromobacter xylosoxidans bacteremia: a 10-year analysis of 54 cases. Eur J Clin Microbiol Infect Dis. 2003; 22:360–363.
10. Molina-Cabrillana J, Santana-Reyes C, González-García A, Bordes-Benítez A, Horcajada I. Outbreak of Achromobacter xylosoxidans pseudobacteremia in a neonatal care unit related to contaminated chlorhexidine solution. Eur J Clin Microbiol Infect Dis. 2007; 26:435–437.

11. Shie SS, Huang CT, Leu HS. Characteristics of Achromobacter xylosoxidans bacteremia in northern Taiwan. J Microbiol Immunol Infect. 2005; 38:277–282.
12. Tena D, Carranza R, Barberá JR, Valdezate S, Garrancho JM, Arranz M, Sáez-Nieto JA. Outbreak of long-term intravascular catheter-related bacteremia due to Achromobacter xylosoxidans subspecies xylosoxidans in a hemodialysis unit. Eur J Clin Microbiol Infect Dis. 2005; 24:727–732.

13. Turel O, Kavuncuoglu S, Hosaf E, Ozbek S, Aldemir E, Uygur T, Hatipoglu N, Siraneci R. Bacteremia due to Achromobacter xylosoxidans in neonates: clinical features and outcome. Braz J Infect Dis. 2013; 17:450–454.

14. Turgutalp K, Kiykim A, Ersoz G, Kaya A. Fatal catheter-related bacteremia due to Alcaligenes (Achromobacter) xylosoxidans in a hemodialysis patient. Int Urol Nephrol. 2012; 44:1281–1283.

15. Saiman L, Chen Y, Gabriel PS, Knirsch C. Synergistic activities of macrolide antibiotics against Pseudomonas aeruginosa, Burkholderia cepacia, Stenotrophomonas maltophilia, and Alcaligenes xylosoxidans isolated from patients with cystic fibrosis. Antimicrob Agents Chemother. 2002; 46:1105–1107.

16. Vay CA, Almuzara MN, Rodríguez CH, Pugliese ML, Lorenzo Barba F, Mattera JC, Famiglietti AM. 'In vitro' activity of different antimicrobial agents on Gram-negative nonfermentative bacilli, excluding Pseudomonas aeruginosa and Acinetobacter spp. Rev Argent Microbiol. 2005; 37:34–45.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download