1. Kim ES. Targeted therapies in thyroid cancer. Endocrinol Metab. 2010; 25:94–97.
3. Choi JY, Youn YK. Vision of thyroid surgery: past, present and future. J Korean Thyroid Assoc. 2012; 5:1–5.
4. Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, Braverman LE. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002; 87:489–499.
5. Choi HS, Park YJ, Kim HK, Choi SH, Lim S, Park DJ, Jang HC, Cho NH, Cho BY. Prevalence of subclinical hypothyroidism in two population based-cohort: Ansung and KLoSHA cohort in Korea. J Korean Thyroid Assoc. 2010; 3:32–40.
6. Yi KH, Park YJ, Koong SS, Kim JH, Na DG, Ryu JS, Park SY, Park IA, Baek CH, Shong YK, Lee YD, Lee J, Lee JH, Chung JH, Jung CK, Choi SH, Cho BY. Revised Korean thyroid association management guidelines for patients with thyroid nodules and thyroid cancer. Korean J Otorhinolaryngol-Head Neck Surg. 2011; 54:8–36.
7. Kim JS. Postoperative quality of life in patients with papillary thyroid cancer. J Korea Acad Industr Coop Soc. 2011; 12:1260–1269.
8. Crevenna R, Zettinig G, Keilani M, Posch M, Schmidinger M, Pirich C, Nuhr M, Wolzt M, Quittan M, Fialka-Moser V, Dudczak R. Quality of life in patients with non-metastatic differentiated thyroid cancer under thyroxine supplementation therapy. Support Care Cancer. 2003; 11:597–603.
9. Tagay S, Herpertz S, Langkafel M, Erim Y, Bockisch A, Senf W, Gorges R. Health-related quality of life, depression and anxiety in thyroid cancer patients. Qual Life Res. 2006; 15:695–703.
10. Park CS, Kang HY, Kwon I, Kang DR, Jung HY. Cost-of-illness study of asthma in Korea: estimated from the Korea National Health Insurance Claims Database. J Prev Med Public Health. 2006; 39:397–403.
11. Lee S, Chung W, Hyun KR. Socioeconomic costs of liver disease in Korea. Korean J Hepatol. 2011; 17:274–291.
12. Jung HK, Jang B, Kim YH, Park J, Park SY, Nam MH, Choi MG. Health care costs of digestive diseases in Korea. Korean J Gastroenterol. 2011; 58:323–331.
13. Jung YH. Cost of illness and health-friendly fiscal policy. Health Welf Policy Forum. 2009; 156:50–61.
14. Chung HK. Environmental factors and thyroid dysfunction. Endocrinol Metab. 2012; 27:191–193.
15. Drummond MF, Sculpher MJ, Torrance GW, O'Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press;2005. p. 17–25. p. 55–72.
16. Park MJ, Choi YS, Tae YH, Choi JH, Baek SJ, Lee HY. Survey on the benefit coverage rate of National Health Insurance in 2010. Seoul: National Health Insurance Service;2011. p. 63–82.
18. Korea Institute for Health and Social Affairs. A Report of Korea health panel survey 2008 (1). Seoul: Korea Institute for Health and Social Affairs;2010. p. 106–135.
26. Noh IC, Suh MH, Kim YR. Socioeconomic costs and policy issues of alcohol drinking. Seoul: Korea Institute for Health and Social Affairs;1997. p. 80.
27. Jung YH, Ko SJ. An estimation of economic costs of 5 major diseases. Health Welf Policy Forum. 2003; 79:55–65.
28. Jung YH, Ko S. The socioeconomic cost of diseases in Korea. J Prev Med Public Health. 2006; 39:499–504.
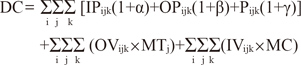
 =age; j gender, k age person's survival ratio at the time of k+τ
=age; j gender, k age person's survival ratio at the time of k+τ =employment rate; j gender, k age person's employment rate at the time of k+τ
=employment rate; j gender, k age person's employment rate at the time of k+τ =annual average wage; j gender, k age person's annual average wage at the time of k+τ
=annual average wage; j gender, k age person's annual average wage at the time of k+τ



 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download