Abstract
Background
Thyroid cancer is a common disease and its prevalence is increasing. Recent reports have shown that an elevated thyrotropin (thyroid stimulating hormone, TSH) level is associated with thyroid cancer risk. However, the association between TSH level and thyroid cancer risk is not yet known for euthyroid patients diagnosed with papillary thyroid microcarcinoma (PTMC).
Methods
Our study included 425 patients who underwent thyroid surgery and were diagnosed with PTMC between 2008 and 2009. Control group patients were diagnosed with benign nodules ≤ 1 cm in size by US-guided fine needle aspiration. Nodules with one or more suspected malignant-ultrasonographic feature(s) were excluded from this study. Patients who were not euthyroid or who took thyroid medication were also excluded.
Results
The mean age of all patients was 48.5 ± 11.0 years and 88.8% were women. The mean age of those with PTMC was significantly lower than that of the control group. The mean TSH level was 1.78 ± 0.93 mIU/L, and the mean free T4 level was 15.96 ± 2.32 pmol/L. There was no difference in TSH level between the PTMC and control groups (1.77 ± 0.93 mIU/L vs. 1.79 ± 0.91 mIU/L, P = 0.829). After adjusting for age, TSH level was not correlated with tumor size (r = 0.02, P = 0.678) in the PTMC group. Moreover, the TSH level did not differ between patients with stage I and stage III-IV carcinoma (stage I, 1.77 ± 0.95 mIU/L; stage III-IV, 1.79 ± 0.87 mIU/L; P = 0.856).
The incidence of thyroid cancer is increasing worldwide, especially the most common form-papillary thyroid carcinoma [1,2]. According to the World Health Organization, if the maximum size of a thyroid carcinoma is ≤ 1 cm, it is a papillary thyroid microcarcinoma (PTMC) [3]. The recent increase in papillary thyroid carcinoma is likely due to increasing early detection of small thyroid nodules because of widespread use of high-resolution ultrasound (US) as well as the accuracy of US-guided fine needle aspiration biopsy (US-guided FNAB). Thyroid papillary carcinoma has a better prognosis than other types of thyroid carcinoma; PTMC in particular is known to have a better prognosis [4,5]. However, some reports have shown that PTMC is associated with lymph nodes and distant metastases [5,6]. One study reported recurrence in 5% of PTMC patients [7]. Therefore, early detection and treatment of PTMC is believed to be important. US-guided FNAB is the gold standard method for diagnosis of thyroid nodules. However, more "inadequate specimens" are found after US-guided FNAB for nodules ≤ 1 cm in size compared with nodules > 1 cm [8]. Thus, if physicians can identify another clinical risk factor for nodules ≤ 1 cm, diagnosis of PTMC may be easier.
Recently, multiple reports have shown an association between serum thyroid stimulating hormone (TSH) level and thyroid cancer. Some studies reported that an elevated serum TSH level was associated with thyroid cancer [9-13], and one study suggested that the serum TSH level was a novel predictor of malignancy [10]. However, another study showed that the serum TSH level was not elevated in papillary thyroid carcinoma [14]. Most studies of associations between serum TSH level and thyroid cancer did not differentiate between the sizes of the thyroid carcinomas studied; only 2 focused on PTMC [13,14]. One of these studies analyzed PTMC patients [14], and the other analyzed patients with differentiated thyroid carcinomas and included a subset analysis of PTMC patients [13].
The purpose of this study was to evaluate whether serum TSH level is elevated in euthyroid PTMC patients and whether it is an important predictor of PTMC.
This was a retrospective study, and information was obtained from patient medical records. We included preoperatively euthyroid patients who underwent thyroid surgery between January 2008 and December 2009 and who were diagnosed with PTMC. If any patient had multiple thyroid papillary carcinomas, the inclusion criterion was that these had a maximal size of ≤ 1 cm. The control group included euthyroid patients who were diagnosed, during the same time period, with benign nodules that were ≤ 1 cm via US-guided FNAB. Among these, nodules with one or more suspected malignant-ultrasonographic feature(s) were excluded. Two clinicians performed the US-guided FNAB, and one of these reviewed the US images and confirmed suspected malignant ultrasonographic features, such as marked hypoechoic nodules, nodules with fine or dense calcification, nodules that were taller than they were wide, and nodules with irregular or speculated margins. Patients who took thyroid medication, had a history of thyroid disease or thyroid surgery, or had atypical cells or suspected malignancy following FNAB were excluded from this study. Euthyroid function was defined as TSH and free T4 levels within reference ranges. Autoimmune thyroiditis was defined as the presence of anti-thyroperoxidase antibody (TPO Ab) and/or anti-thyroglobulin antibody (Tg Ab).
Serum TSH and free T4 levels were determined for all subjects by electric chemiluminescence immunoassay (Roche Diagnostics, Mannheim, Germany); the reference ranges were 0.4-4.7 mIU/L and 9.0-24.5 pmol/L, respectively.
Tumor size was measured from surgical specimens; if multiple PTMCs were found, the largest carcinoma was measured. The size of benign nodules was determined by ultrasonography. The TNM criteria of the American Joint Committee on Cancer were used for staging PTMC [15].
Statistical analysis was performed using SPSS for Windows version 14.0 (SPSS Inc., Chicago, IL, USA), and data are presented as mean ± standard deviation. A two-sample t-test and a chi-square test were used to evaluate variables between the PTMC and control groups. A Pearson correlation test and age-adjusted partial correlation test were performed to evaluate relationships between variables. P value of < 0.05 was considered statistically significant.
A total of 562 patients were available for analysis. Their mean age was 48.5 ± 11.0 years, and 88.8% were women. The mean serum TSH level was 1.78 ± 0.93 mIU/L, and the mean serum free T4 level was 15.96 ± 2.32 pmol/L. After surgery, 425 patients were histologically diagnosed with PTMC, of which 89.6% were women. A total of 13.4% of PTMC patients underwent lobectomy (Table 1).
PTMC patients were significantly younger than control group patients, and there was no between-group difference in sex. The serum TSH level in the PTMC group was not significantly different compared with that in the control group (1.77 ± 0.93 mIU/L vs. 1.79 ± 0.91 mIU/L; P = 0.829); the serum free T4 level was also not significantly different. The nodule size was significantly smaller among patients in the PTMC group (PTMC, 0.52 ± 0.24 cm vs. control, 0.69 ± 0.18 cm; P = 0.001). The prevalence of autoimmune thyroiditis was higher in PTMC than in benign nodules (Table 1).
When autoimmune thyroiditis was defined as the presence of TPO Ab and/or Tg Ab, we found higher rates of PTMC in patients with autoimmune thyroiditis (autoimmune thyroiditis, 82.1% vs. control, 73.3%; P = 0.036). However, serum TSH levels within the normal range did not differ depending on the presence of autoimmune thyroiditis (autoimmune thyroiditis, 1.90 ± 1.00 mIU/L vs. control, 1.73 ± 0.90 mIU/L; P = 0.075).
Correlations between TSH level and other variables are shown in Table 2. We analyzed correlations between serum TSH and other variables among all patients. The serum TSH level was negatively correlated with the serum free T4 level (r = -0.224, P < 0.001), but it was not correlated with age (r = -0.048, P = 0.253) or nodule size (r = 0.027, P = 0.527). After adjustment for age, the negative correlation between serum TSH and free T4 persisted (r = -0.229, P < 0.001). Similar results were observed among the subset of PTMC patients. Serum TSH and free T4 had a significantly negative correlation (r = -0.232, P < 0.001), but serum TSH was not correlated with age (r = -0.010, P = 0.832) or tumor size (r = 0.019, P = 0.696).
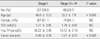
Of the PTMC patients, 17.9% (n = 76) had microscopic extrathyroidal invasion (T3) and none had T4 stage carcinoma. In addition, 25.6% (n = 109) had cervical lymph node metastasis. Serum TSH levels according to TNM stage are shown in Fig. 1. The serum TSH level in patients with T3 stage carcinoma was significantly increased compared with that in patients with T1 stage carcinoma (1.98 ± 0.95 mIU/L vs. 1.72 ± 0.92 mIU/L; P = 0.03). There was no difference in serum TSH levels based on lymph node metastasis (N0, 1.81 ± 0.95 mIU/L; N1, 1.67 ± 0.90 mIU/L; P = 0.188). Stage I, II, III, and IV cancer was found in 337, 0, 82, and 6 patients, respectively. Because of the small number of patients with stage IV cancer, we merged the patients with stage III and IV cancer into 1 group. Comparisons between patients with limited-(stage I) and advanced-stage (stage III-IV) cancer are shown in Table 3. Patients with advanced-stage cancer were significantly older and had significantly larger tumors (P < 0.001). Serum TSH levels did not differ between limited- and advanced-stage cancer patients (stage I, 1.77 ± 0.95 mIU/L; stage III-IV, 1.79 ± 0.87 mIU/L; P = 0.856).
This study showed that in euthyroid patients with PTMC, the serum TSH level is not significantly different from that in patients with benign nodules ≤ 1 cm in size and that serum TSH level is not associated with tumor size or cancer stage.
PTMC is known to have a favorable prognosis compared with papillary carcinomas > 1 cm in size. However, lymph node metastasis and distant metastasis can still occur in PTMC patients [5,6]. In this study, although no patient had distant metastasis, 25.6% had lymph node metastasis and 20.7% had advanced-stage cancer (stages III-IV). Therefore, we suggest that clinicians continue to attempt to identify microcarcinomas in patients with nodules ≤ 1 cm in size.
Serum TSH level plays an important role in the diagnosis of thyroid nodules. The American Thyroid Association recommends that serum TSH levels be measured in patients with thyroid nodules and if the TSH level is suppressed, a thyroid scan must be performed to confirm nodule autonomy [16]. It is known that serum TSH level is related to thyroid cancer. The relationship between serum TSH and thyroid cancer is supported by reports indicating that in differentiated thyroid cancer, the suppression of serum TSH level by exogenous thyroid hormone reduces cancer progression and recurrence [17,18]. However, other report showed that suppression of serum TSH have no significant clinical benefit in patients with low-risk thyroid cancer [19]. These reports argue that other factors, such as IGF-1, have a more important role in cancer growth [20] and that the expression of the TSH receptor gene in thyroid cancer is associated with a favorable prognosis [21]. In summary, many studies have attempted to confirm the relationship between the development of thyroid cancer and serum TSH level, and most have shown that an elevated TSH level is related to thyroid cancer. The elevated serum TSH level in patients with thyroid abnormalities is associated with thyroid cancer; even within the normal range, there is a higher risk of thyroid cancer among patients with a higher serum TSH level [9-12]. However, few studies have included only PTMC patients; therefore, the results have been conflicting. In a separate subset analysis of nodules ≤ 1 cm in size, Haymart et al. [13] showed that a higher TSH level increased the risk of differentiated thyroid cancer. Gesrschpacher et al. [14] reported that the serum TSH level was not elevated in patients with PTMC, even if the study had patients with medullary thyroid carcinoma or C-cell hyperplasia in the control group. Although Haymart et al. [13] showed that a higher serum TSH level, even within the normal range, was associated with differentiated thyroid cancer by a subset analysis of differentiated thyroid cancer of less than 1 cm, the relationship between serum TSH level and PTMC has not been described for euthyroid patients with PTMC.
Studies of the relationship between autoimmune thyroiditis and thyroid cancer have also reported conflicting results. Boelaert et al. [10] showed that TPO Ab-positive patients had higher rates of thyroid cancer compared with those in Ab-negative patients. However, in another study, the frequency of papillary thyroid cancer was not significantly different between antibody (TPO Ab and/or Tg Ab)-positive and antibody (TPO Ab and/or Tg Ab)-negative patients, and the risk of thyroid cancer was higher in patients with a higher serum TSH level [12]. Our study found higher rates of thyroid cancer in Ab-positive patients, but serum TSH level within the normal range did not differ between Ab-positive and Ab-negative patients.
We studied patients with PTMC and benign nodules ≤ 1 cm and showed that a higher serum TSH level was not associated with PTMC. Contrary to Haymart's results, when we divided patients into three groups based on TSH levels, a higher TSH level did not increase the risk of differentiated thyroid cancer. Yoshihara et al. [22] showed the serum TSH levels shifted to higher ranges as the age of the groups increased in a Japanese population. The fact that PTMC patients were younger than those in the control group could have influenced our results even though age was not correlated with serum TSH level in our study. Serum TSH level within the normal range did not differ between thyroid Ab-positive and Ab-negative patients.
In our study, serum TSH level was not associated with tumor size or cancer stage, but the TSH level in T3 stage carcinomas (extrathyroidal invasion) was significantly higher compared with that in T1 stage carcinomas. It is well known that serum TSH is a thyroid tissue growth factor. One study showed that suppression of the TSH level by exogenous thyroid hormone prevented the growth of preexisting thyroid nodules as well as the development of new nodules [23]. Long-term suppression of the TSH level also reduces progression, recurrence, and cancer-related mortality in thyroid cancer [17, 18]. Thus, it is believed that the serum TSH level is associated with thyroid cancer growth. Some studies have shown that a higher serum TSH level is associated with cancer stage; however, these did not analyze thyroid microcarcinomas [12,13]. In one study including PTMCs, the authors observed a positive trend between serum TSH level and tumor size, but the number of subjects in the study was very small [14]. Our study revealed that serum TSH level was not correlated with tumor size, but a higher TSH level was observed in patients with extrathyroidal invasion. Thus, further studies evaluating the relationship between PTMC progression and serum TSH level are required.
Our study has some limitations. First, the number of patients with benign nodules was smaller than the number of PTMC patients. Among the euthyroid patients with benign nodules identified by US-guided FNAB, 29.7% were excluded from our study because they had nodules with one or more suspected malignant ultrasonographic features. This may have created a significant selection bias. Second, although one clinician reviewed the US findings and excluded nodules with one or more suspected malignant ultrasonographic features, there is a possibility that PTMC patients were included in the control group. We selected the control group from patients who had one or more US-guided FNABs, but 83.2% of all patients had one FNAB, and the follow-up period was short. Cytologically, they had no malignant features and never had any suspected malignant ultrasonographic features. However, the final diagnosis for patients in the benign control group was not confirmed histologically. Therefore, further research with a control group that has had at least 2 FNABs and a longer term follow-up is required. Third, in lobectomy cases, the remaining contralateral lobe was not explored for PTMCs. If the remaining lobe had PTMCs, differences in tumor size could have influenced our correlation analysis of serum TSH level and tumor size.
In conclusion, it is known that an elevated TSH level is associated with thyroid cancer risk. However, in euthyroid PTMC patients, the association between serum TSH level and cancer risk has, to date, remained unknown. This study showed that in such patients, the serum TSH level was not significantly different compared with that in patients with benign nodules ≤ 1 cm in size. Moreover, the TSH level was not associated with tumor size. Therefore, further evaluations are required to determine whether serum TSH can be used as a tumor marker for small nodules ≤ 1 cm in euthyroid patients.
Figures and Tables
Fig. 1
Comparison of thyroid stimulating hormone (TSH) levels according to tumor, node and metastasis (TNM) stage. (A) TSH level in stage T3 was significantly higher than that in stage T1. (B) TSH level in N0 was not significantly different compared with that in N1. NS, not significant.

References
1. Sherman SI. Thyroid carcinoma. Lancet. 2003. 361:501–511.
2. Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006. 295:2164–2167.
3. Hedinger C, Williams ED, Sobin LH. The WHO histological classification of thyroid tumors: a commentary on the second edition. Cancer. 1989. 63:908–911.
4. Yamamoto Y, Maeda T, Izumi K, Otsuka H. Occult papillary carcinoma of the thyroid. A study of 408 autopsy cases. Cancer. 1990. 65:1173–1179.
5. Noguchi S, Yamashita H, Uchino S, Watanabe S. Papillary microcarcinoma. World J Surg. 2008. 32:747–753.
6. Strate SM, Lee EL, Childers JH. Occult papillary carcinoma of the thyroid with distant metastases. Cancer. 1984. 54:1093–1100.
7. Kim TY, Hong SJ, Kim JM, Gu Kim W, Gong G, Ryu JS, Kim WB, Yun SC, Shong YK. Prognostic parameters for recurrence of papillary thyroid microcarcinoma. BMC Cancer. 2008. 8:296.
8. Choi YJ, Park YL, Koh JH. Prevalence of thyroid cancer at a medical screening center: pathological features of screen-detected thyroid carcinomas. Yonsei Med J. 2008. 49:748–756.
9. Lim AK, Daykin J, Holder R, Sheppard MC, Franklyn JA. Measurement of serum TSH in the investigation of patients presenting with thyroid enlargement. QJM. 1998. 91:687–689.
10. Boelaert K, Horacek J, Holder RL, Watkinson JC, Sheppard MC, Franklyn JA. Serum thyrotropin concentration as a novel predictor of malignancy in thyroid nodules investigated by fine-needle aspiration. J Clin Endocrinol Metab. 2006. 91:4295–4301.
11. Jonklaas J, Nsouli-Maktabi H, Soldin SJ. Endogenous thyrotropin and triiodothyronine concentrations in individuals with thyroid cancer. Thyroid. 2008. 18:943–952.
12. Fiore E, Rago T, Provenzale MA, Scutari M, Ugolini C, Basolo F, Di Coscio G, Berti P, Grasso L, Elisei R, Pinchera A, Vitti P. Lower levels of TSH are associated with a lower risk of papillary thyroid cancer in patients with thyroid nodular disease: thyroid autonomy may play a protective role. Endocr Relat Cancer. 2009. 16:1251–1260.
13. Haymart MR, Repplinger DJ, Leverson GE, Elson DF, Sippel RS, Jaume JC, Chen H. Higher serum thyroid stimulating hormone level in thyroid nodule patients is associated with greater risks of differentiated thyroid cancer and advanced tumor stage. J Clin Endocrinol Metab. 2008. 93:809–814.
14. Gerschpacher M, Göbl C, Anderwald C, Gessl A, Krebs M. Thyrotropin serum concentrations in patients with papillary thyroid microcancers. Thyroid. 2010. 20:389–392.
15. Patel SG, Shah JP. TNM staging of cancers of the head and neck: striving for uniformity among diversity. CA Cancer J Clin. 2005. 55:242–258.
16. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009. 19:1167–1214.
17. Mazzaferri EL, Jhiang SM. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med. 1994. 97:418–428.
18. Sipos JA, Mazzaferri EL. The therapeutic management of differentiated thyroid cancer. Expert Opin Pharmacother. 2008. 9:2627–2637.
19. Biondi B, Filetti S, Schlumberger M. Thyroid-hormone therapy and thyroid cancer: a reassessment. Nat Clin Pract Endocrinol Metab. 2005. 1:32–40.
20. Derwahl M, Broecker M, Kraiem Z. Clinical review 101: thyrotropin may not be the dominant growth factor in benign and malignant thyroid tumors. J Clin Endocrinol Metab. 1999. 84:829–834.
21. Shi Y, Zou M, Farid NR. Expression of thyrotrophin receptor gene in thyroid carcinoma is associated with a good prognosis. Clin Endocrinol (Oxf). 1993. 39:269–274.
22. Yoshihara A, Noh JY, Ohye H, Sato S, Sekiya K, Kosuga Y, Suzuki M, Matsumoto M, Kunii Y, Watanabe N, Mukasa K, Ito K, Ito K. Reference limits for serum thyrotropin in a Japanese population. Endocr J. 2011. 58:585–588.
23. Papini E, Petrucci L, Guglielmi R, Panunzi C, Rinaldi R, Bacci V, Crescenzi A, Nardi F, Fabbrini R, Pacella CM. Long-term changes in nodular goiter: a 5-year prospective randomized trial of levothyroxine suppressive therapy for benign cold thyroid nodules. J Clin Endocrinol Metab. 1998. 83:780–783.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download