Abstract
Objective
To assess the role of fertility preservation in the treatment of patients with early epithelial ovarian cancer (EOC).
Methods
We retrospectively analyzed the medical records of 21 patients with early EOC from January 1995 to December 2006. All eligible patients with a strong desire to preserve fertility were younger than 35 years and underwent fertility-sparing surgery with or without adjuvant chemotherapy.
Results
Twenty-one eligible patients with a median age of 26.7 years (range, 20 to 33 years) were identified, and the mean follow-up period was 43 months (range, 5 to 86 months). Only one patient with stage IC recurred 34 months after the first operation. A total of five patients were able to become pregnant at least once after the first fertility preserving treatment, with or without adjuvant chemotherapy. All five patients succeeded in full-term vaginal delivery with healthy infants. No patients died of their disease.
Patients with epithelial ovarian cancers have an advanced disease at diagnosis in more than two thirds of the cases, because the patients are usually asymptomatic until the cancer has metastasized.
Recently, with the help of several developed diagnostic tools, and an increase in self-health monitoring among women, early detection of ovarian cancer has increased. Approximately 25% of patients given the diagnosis of ovarian cancer are classified as stage I, or with early epithelial ovarian cancer (EOC) with five-year survival rates approaching 90%.1
The necessary treatment for most of the common cancer types occurring in younger women implies either removal of the reproductive organs or cytotoxic treatment that could partially or definitively affect reproductive function. However, most young patients with malignancies want to be managed focusing on the quality of life after treatment. One of these changes is fertility-preservation management in epithelial ovarian cancer.
Early loss of ovarian function not only puts the patients to the risk for menopause-related complications at a very young age but is also associated with loss of fertility. Therefore, there has been a gradual increase in patients facing the risk of premature ovarian failure and therefore seeking help in preserving fertility.
In the absence of large prospective randomized trials and cohort studies, it is difficult to determine how to best manage these young patients. The current study is a retrospective review of our experience of fertility preservation in patients with early epithelial ovarian cancer. Here, we report data from a single institute as a helpful guide in determining the best management of early epithelial ovarian cancer in young patients.
We retrospectively reviewed the charts of 21 women with early epithelial ovarian cancer who had a strong desire to preserve fertility and had been treated with simple unilateral salpingo-oophorectomy (USO) or a staging operation (USO, bilateral pelvic and para-aortic lymphadenectomy, omentectomy, and multiple biopsies) as a primary fertility-sparing operation at General Hospital and Women's Healthcare Center from January 1995 to December 2006. The criteria for performing USO in 7 patients included pathologically confirmed absence of capsule invasion, well differentiated grade, favorable histologic type, and no evidence of intra-operatively suspicious lesion such as enlarged lymph nodes. The other unfavorable factors were included in the criteria for a staging operation. For inclusion in the study, women must have been pathologically confirmed as International Federation of Obstetrics and Gynecology (FIGO) stage I, have no distant metastasis on magnetic resonance imaging (MRI) or ultrasonography (USG), have a strong desire to preserve fertility, and have received extensive counseling regarding the possibility of tumor recurrence or progression.
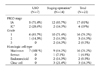
The mean age at diagnosis was 26.7 years (range, 22 to 33 years). The mean follow-up period was 43 months (range, 5 to 86). Of the 21 women, 17 were FIGO stage IA, and the other four were FIGO stage IC. With respect to grade, sixteen cases were grade 1, three were grade 2, and two were grade 3. Also, sixteen cases were mucinous histologic cell type, two were endometrioid type, two were clear cell type, and one had a serous type (Table 1).
Of the 21 patients, seven received a simple USO and fourteen received a staging operation (USO, bilateral pelvic and paraaortic lymphadenectomy, omentectomy and multiple biopsy). Thirteen high-risk patients received adjuvant chemotherapy (high risks: unfavorable cell type such as clear cell, poor differentiation, Stage IC including positive cytology). Of the 21 women, only one patient with FIGO stage IC recurred 34 months after the first operation; she had the mucinous cell type, grade 1 and received a staging operation with adjuvant chemotherapy (Table 2).
A total of five patients were able to become pregnant after the first fertility preserving treatment, with or without adjuvant chemotherapy. The other patients have not any record of pregnancy in our hospital. All five women became pregnant naturally, without assisted reproductive technology (ART). All five patients succeeded in full-term vaginal delivery. The mean duration between treatment and pregnancy was seven months (range, 2 to 54 months). All five patients were stage IA. There were two pregnancies among seven patients who underwent USO, and three pregnancies among the fourteen patients who underwent the staging operation. Also, there were two out of thirteen patients who received adjuvant chemotherapy and three out of eight patients who did not receive adjuvant therapy (Table 3).
EOC is the leading cause of death among all gynecological malignancies.2 The standard management of EOC is based on the primary surgery, including hysterectomy and bilateral salpingo-oophorectomy with peritoneal sampling (peritoneal washing, omentectomy, multiple peritoneal biopsies, and the removal of peritoneal implants) with lymph-node biopsy.
During the past two decades, there has been an increasing incidence of early EOC in young women who have a strong desire to preserve fertility due to evolving early detection methods and an increase in late gravidity. Several reports have estimated that 3-17% of all EOCs occur in women under 40 years of age.3-7 In these patients, the preservation of the reproductive and endocrine functions is crucial. Therefore, fertility-sparing surgery has figured prominently in the consideration of appropriate gynecologic malignancy treatment.
In contrast to simple unilateral salpingo-oophorectomy, the fertility-preserving staging operation is more aggressive, and postoperative pelvic adhesions may be more common, which might be considered a mechanical cause of infertility. However, our present study indicates that there was no difference in the pregnancy of the two subgroups (all pregnancies occurred naturally).
Also, several authors have reported lymph node metastases in patients with clinically apparent Stage I ovarian cancer.8-11 Cass and colleagues, for example, noted that 14 of 96 women (15%) with apparent Stage I epithelial ovarian cancer at the time of surgery had occult lymph nodal metastases.11 Therefore, in order to preserve fertility while guaranteeing patient survival, a complete staging operation should be performed.
Adjuvant chemotherapy in patients with Stage I epithelial ovarian cancer is necessary in situations including unfavorable cell types, poor histologic differentiation, and stage IC. A number of studies have concluded that the use of adjuvant chemotherapy offers no survival advantage to patients with well-differentiated Stage IA epithelial ovarian cancers.12-14 These data were well supported by our results showing that eight of 21 patients with Stage IA grade 1 cancers in the present study received no adjuvant chemotherapy, and all of these patients had no evidence of recurrence. In contrast, adjuvant chemotherapy improved in the survival of patients with moderately or poor differentiated Stage I EOC. In our study, thirteen of 21 patients received adjuvant chemotherapy, a group that included four patients with grade 2 or grade 3, four with Stage IC, and two with clear cell type histology. However, at present, there is little evidence to suggest that there are different indications for chemotherapy in Stage I ovarian cancer patients treated with conservative surgery when compared to similar patients treated with more radical surgery.15,16
Also, we should consider any cytotoxic effects on ovarian tissue when adjuvant chemotherapy is applied to improve the in the survival of patients undergoing fertility-preserving treatment. However, in contrast to the past regimens of which have involved alkylating agents (Cyclophosphamide, Melphalan, Busulfan, Chlorambucil, Procarbazine, Nitrosureas, Ifosfamide), the recent regimens of chemotherapy include paclitaxel and carboplatin, the cytotoxic effects of which have not been proven. In the present study, the majority of regimens included platinum-based cyclophosphamide, but there was no evidence of cytotoxic effects on the fertility in two pregnancies out of 13 patients with chemotherapy, compared to three out of 8 patients without adjuvant chemotherapy. Two out of 13 patients received adjuvant chemotherapy, and three out of eight patients who did not receive adjuvant therapy (p-value=0.248). A more advanced, larger study investigating the cytotoxity of chemotherapeutic agents should be conducted.
The ultimate aim of fertility-preserving treatment in patients with early EOC is childbearing and delivery of a healthy infant. Recently, ART technology has advanced, with treatment ranging from the routinely utilized embryo cryopreservation to more experimental techniques such as oocyte and ovarian-tissue cryopreservation. In our study, the mean duration between the fertility-preserving operation and pregnancy was seven months (range, 2 to 54 months). All five patients who eventually became pregnant did not receive any ART. If all 21 patients in the present study had received ART to become pregnant, the rate of pregnancy might be higher. However, we make a point of considering unresolved problems that include the starting time of ART after first fertility-preserving treatment, the effects on prognosis of EOC, and proper follow-up methods.
In conclusion, fertility-preserving treatment can be considered a proper treatment strategy in patients with early EOC. To improve the quality of life in young patients with early EOC, a much more detailed study regarding the conservative management of early gynecologic malignancies should be required.
Figures and Tables
References
1. Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, et al. Cancer statistics, 2006. CA Cancer J Clin. 2006. 56:106–130.
2. Greenlee RT, Hill-Harmon MB, Murray T, Thun M. Cancer statistics, 2001. CA Cancer J Clin. 2001. 51:15–36.
3. Duska LR, Chang YC, Flynn CE, Chen AH, Goodman A, Fuller AF, et al. Epithelial ovarian carcinoma in the reproductive age group. Cancer. 1999. 85:2623–2629.
4. Plaxe SC, Braly PS, Freddo JL, McClay E, Kirmani S, Howell SB. Profiles of women age 30-39 and age less than 30 with epithelial ovarian cancer. Obstet Gynecol. 1993. 81:651–654.
5. Rodriguez M, Nguyen HN, Averette HE, Steren AJ, Penalver MA, Harrison T, et al. National survey of ovarian carcinoma XII. Epithelial ovarian malignancies in women less than or equal to 25 years of age. Cancer. 1994. 73:1245–1250.
6. Swenerton KD, Hislop TG, Spinelli J, LeRiche JC, Yang N, Boyes DA. Ovarian carcinoma: a multivariate analysis of prognostic factors. Obstet Gynecol. 1985. 65:264–270.
7. Smedley H, Sikora K. Age as a prognostic factor in epithelial ovarian carcinoma. Br J Obstet Gynaecol. 1985. 92:839–842.
8. Piver MS, Barlow JJ, Lele SB. Incidence of subclinical metastasis in stage I and II ovarian carcinoma. Obstet Gynecol. 1978. 52:100–104.
9. Chen SS, Lee L. Incidence of para-aortic and pelvic lymph node metastases in epithelial carcinoma of the ovary. Gynecol Oncol. 1983. 16:95–100.
10. Burghardt E, Girardi F, Lahousen M, Tamussino K, Stettner H. Patterns of pelvic and paraaortic lymph node involvement in ovarian cancer. Gynecol Oncol. 1991. 40:103–106.
11. Cass I, Li AJ, Runowicz CD, Fields AL, Goldberg GL, Leuchter RS, et al. Pattern of lymph node metastases in clinically unilateral stage I invasive epithelial ovarian carcinomas. Gynecol Oncol. 2001. 80:56–61.
12. Young RC, Walton LA, Ellenberg SS, Homesley HD, Wilbanks GD, Decker DG, et al. Adjuvant therapy in stage I and stage II epithelial ovarian cancer: Results of two prospective randomized trials. N Engl J Med. 1990. 322:1021–1027.
13. NIH Consensus Development Panel on Ovarian Cancer. NIH consensus conference: Ovarian cancer. Screening, treatment, and follow-up. JAMA. 1995. 273:491–497.
14. Le T, Krepart GV, Lotocki RJ, Heywood MS. Clinically apparent early stage invasive epithelial ovarian carcinoma: Should all be treated similarly? Gynecol Oncol. 1999. 74:252–254.
15. Colombo N, Chiari S, Maggioni A, Bocciolone L, Torri V, Mangioni C. Controversial issues in the management of early epithelial ovarian cancer: conservative surgery and role of adjuvant therapy. Gynecol Oncol. 1994. 55(3 Pt 2):S47–S51.
16. Zanetta G, Chiari S, Rota S, Bratina G, Maneo A, Torri V, et al. Conservative surgery for stage I ovarian carcinoma in women of childbearing age. Br J Obstet Gynaecol. 1997. 104:1030–1035.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download