INTRODUCTION
Duchenne muscular dystrophy (DMD) is an X-linked recessive disorder affecting 1 in every 3500 males that results from mutations in the gene that encodes dystrophin, a sarcolemmal protein abundant in skeletal and cardiac muscle cells.
1 Dystrophin has an important role in maintaining the integrity of the sarcolemma. The dystrophin mutation leads to weakening of the sarcolemma, which results in the loss of membrane integrity, activation of degradative pathways, and ultimately necrosis and fibrosis of the myocyte.
23 Patients with this mutation show progressive skeletal muscle weakness, loss of ambulation, and cardiac dysfunction. Most patients with DMD lose their ambulatory function in their early teens. Cardiac dysfunction starts in the second decade of life, and death mostly occurs in the second or third decade of life due to cardiac failure.
45 Due to the development of supportive care for respiratory dysfunction in patients with DMD,
6 cardiomyopathy is becoming more prevalent and is the leading cause of death for these patients. Therefore, early detection of myocardial involvement is crucial for the survival of patients with DMD.
Transthoracic echocardiography is the gold standard for evaluating cardiac function in DMD, which typically shows the left ventricular ejection fraction (LV EF) and fractional shortening (LV FS), and more advanced tissue Doppler imaging additionally shows myocardial strain. In the past, myocardial strain measurement was performed only with angle-dependent tissue Doppler imaging; recently, angle-independent strain measurement has been made possible by the speckle-tracking technique in echocardiography.
Previous researchers have attempted to detect cardiac abnormalities earlier. A previous study reported that cardiac magnetic resonance imaging (MRI) is useful for identifying subtle myocardial dysfunction even if the LV EF is within the normal limit. It was demonstrated that patients with DMD who were <10 years of age showed lower LV myocardial circumferential strain on cardiac MRI than healthy children.
7
Recently, two-dimensional (2D) echocardiography has become a viable alternative to MRI for the evaluation of myocardial strain. Adamu, et al.
8 were the first to measure three-layer circumferential strain using advanced 2D echocardiography in normal subjects and suggested that it would be feasible to assess myocardial function via this layer-specific strain.
9
The purpose of this study was to analyze myocardial deformation in children with DMD by assessing longitudinal, radial, and circumferential myocardial strain using three–myocardial layer–specific analysis involving speckle-tracking imaging to explore their unique myocardial movement characteristics.
MATERIALS AND METHODS
Subjects
We reviewed the medical records of patients with DMD who were over 10 years of age (15.6±1.6 years, max 18 years, min 12.5 years), who had been followed up at Gangnam Severance Hospital from March 2013 to June 2014. All patients with DMD in this study did not require respiratory support, such as nasal intermittent positive pressure ventilation, and were capable of wheelchair ambulation. Twenty-four children with DMD underwent transthoracic echocardiography. They did not have definite symptoms or signs of heart failure. The diagnosis of DMD was confirmed via skeletal muscle biopsy showing the absence of dystrophin and/or DNA analysis demonstrating a characteristic dystrophin mutation. Twenty-four weight-matched healthy volunteers were enrolled in this study as a control group, and all underwent transthoracic echocardiography with an identical protocol for the comparison.
Echocardiogram and strain analysis
All conventional echocardiographic measurements and advanced myocardial imaging studies were obtained in both patients with DMD and healthy control children using a Siemens model ACUSON SC2000 (Siemens Medical Solutions USA, Inc., Mountain View, CA, USA). Echocardiographic examinations were conducted according to the recommendations of the American Society of Echocardiography. In conventional echocardiographic measurements, the LV EF was measured using the M-mode and the Sympson method. The images were recorded with a frame rate of over 50 frames/s in order to investigate the myocardial strain and strain rate. A parasternal short axis view was acquired for evaluating radial and circumferential strain, as was a four-chamber view for radial and longitudinal strain. Velocity vector imaging was used for the layer-specific analysis of strain by assessing the strain rate at the endocardial, middle myocardial, and epicardial layers.
Statistical analysis
All data and measurements are reported as mean±SD. We compared all demographic and echocardiographic data of children with DMD with those of healthy controls using the independent t-test. Statistical significance was inferred on the basis of a p value less than or equal to 0.05. All statistical calculations were made using SPSS 19.0 (IBM, Armonk, NY, USA).
RESULTS
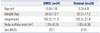
Between patients with DMD and healthy control groups, the weight and body surface area showed no significant differences, although patients with DMD were older than those in the control group (
Table 1).
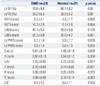
Conventional echocardiographic measurement demonstrated that the LV EF was 53.8±9.8% for patients with DMD. Fractional shortening was 28.0±6.3%. None of the enrolled patients had been diagnosed with cardiomyopathy, which was defined as an LV EF of less than 45%; however, their LV EF was lower than healthy controls. Interventricular septal wall thickness was increased at the end-diastolic phase, and the LV end systolic dimension (LVESD) was larger in patients with DMD than in the control group (
Table 2). The conventional mitral inflow measurements E, E/A, and tissue Doppler diastolic E' were significantly lower in the patients with DMD (
Table 2).
Myocardial strain measurements were acquired via an offline process in the longitudinal, radial, and circumferential directions with three-layer specific analyses at the endocardium, middle myocardium, and epicardium. Radial strain measured in the apical four-chamber view was not significantly different between the two groups (
Table 3). Longitudinal strain did not differ between the two groups in the endocardium and middle myocardium. However, longitudinal strain of the epicardium did significantly decrease in patients with DMD (DMD: -9.3±3.8%; control: -12.3±4.3%;
p=0.012). The strain rate showed no significant difference between the two groups in the apical four-chamber view (
Table 3).
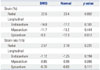
Radial strain measured on the parasternal short axis view was lower in patients with DMD than in healthy controls (DMD: 24.1±11.1%; control: 37.3±25.9%; p=0.027), and the radial strain rate in the DMD patient group was significantly lower (DMD: 1.68±0.91; control: 2.42±0.84; p=0.006).
Circumferential strain in the endocardium (DMD: -17.5±4.7%; control: -24.2±5.3%;
p<0.001), middle myocardium (DMD: -12.7±3.8%; control: -18.0±4.0%;
p<0.001), and epicardium (DMD: -8.4±4.0%; control: -12.2±5.0%;
p=0.006) was significantly decreased in patients with DMD. The circumferential strain rates of patients with DMD also showed lower values in the endocardial (DMD: -1.46±0.38; control: -1.78± 0.27;
p=0.002) and middle myocardial layers (DMD: -1.02±0.27; -1.28±0.22;
p=0.001). In the epicardial layer, the strain rate was also lower in the DMD patient group, although there was no statistical difference (
Table 4).
DISCUSSION
Despite the use of transthoracic echocardiography as the gold standard of cardiac function evaluation in patients with DMD, many physical issues make this echocardiographic examination challenging. Diminished image resolution makes demarcation of the endocardial border difficult and increases the likelihood of measurement mistakes. The standard measures of cardiac function also become more limited as patients become older.
10 Nevertheless, echocardiography is the most universally standardized assessment of myocardial function for patients with DMD in the current era. To diagnose early cardiac deterioration, diverse echocardiographic techniques should be applied for patients with DMD, including conventional and advanced myocardial imaging. Assessment of cardiac function with strain imaging is feasible, and myocardial strain measurements identified early myocardial disease in patients with DMD.
3
In our study results, children with DMD demonstrated significantly lower circumferential strain than healthy controls, as mentioned in other studies.
710 Hor, et al.
7 reported that circumferential strain at the LV free wall on cardiac MRI was significantly lower in patients with DMD than in controls, despite the LV EFs in children with DMD being within normal limits. Ryan, et al.
10 published a study that found that all circumferential strain is significantly decreased in patients with DMD, particularly in the anteroseptal, inferior, and inferolateral myocardial segments.
In our present study, we assessed the myocardium as three layers: endocardium, myocardium, and epicardium. We noticed that myocardial circumferential dysfunction could occur earlier at all three layers, even with preserved longitudinal function. The early deterioration of circumferential strain may be caused by the configuration of the LV myofibril. According to previous research, the direction of LV myofibrils is mainly circumferential.
11 Leitman, et al.
9 reported that the ratio of circumferentially to longitudinally oriented fibers is almost 10:1, increasing toward the base and decreasing toward the apex. Our results are in agreement with Leitman's publication, which showed circumferential strain in patients with regional LV dysfunction. At all myocardial levels, three-layer circumferential strain in the abnormally contracting segments was lower than in the corresponding intact segments, while at the basal epicardial layer, this difference was of borderline significance.
9 Circumferential strain behaves in a different way, with a basal-to-apical gradient in all three myocardial layers; thus, the radius of curvature toward the apex for circumferential strain decreases.
12
LV myocardial architecture has been represented as a muscle band continuum, spatially organized such that the right-handed helical geometry in the subendocardial region gradually changes to left-handed geometry in the subepicardial region. This geometrical difference between the endocardium, middle myocardium, and epicardium creates the circumferential transmural strain gradient.
13 The LV myocardial architecture and the circumferential transmural gradient are considered to be important in electrical propagation and myocardial contraction. As patients with DMD have a structural defect of the myocyte, myofiber dysfunction is thought to lead to contractile dysfunction. In other words, decreased circumferential strain could be an early marker for predicting elusive myocardial dysfunction. Therefore, circumferential strain can be a sensitive indicator of myocardial dysfunction before loss of myocytes and fibrosis.
Furthermore, our study observed the three myocardial layers individually and found that circumferential strain alteration started from the middle myocardial layer and progressed to the endocardial layer, in terms of order and severity. The epicardial layer may deteriorate to a lesser extent or later; it may also remain relatively preserved despite functional decline at the middle myocardium and endocardium. This result is indeed a unique and promising finding for myocardial assessment in children with DMD.
In the second decade of life, respiratory and cardiac muscle diseases become significant contributors to disease progression and quality of life impairment. Improvements in the treatment of respiratory muscle problems, including assistive devices and mechanical ventilation, allow patients to survive longer with enhanced respiratory function. However, this longer lifespan has resulted in cardiac disease emerging as a major cause of patient morbidity and mortality in DMD.
10
With the development of respiratory support care, cardiomyopathy has become the leading cause of death.
614 With this paradigm shift, a sharp focus on the diagnosis and treatment of cardiac problems is critical in patients with DMD.
The purpose of cardiac treatment is to decelerate the deterioration of myocardial function with various drugs in order to enable it to remain close to normal. Until recently, the starting point of cardiac treatment has been the onset of heart failure symptoms or signs. However, although many parameters of conventional echocardiography may be within normal range, detailed functional indicators such as strain measurements must be already decreased, as our study demonstrated. We would therefore reconsider the starting point of cardiac treatment for patients with DMD and subtle myocardial dysfunction.
Several studies showed that patients with DMD obtain a better cardiac outcome with early medical treatment for myocardial deterioration. Duboc, et al.
1516 initiated treatment with angiotensin-converting enzyme inhibitors (ACEi) for patients with DMD aged between 9.5 and 13 years even in normal EF and reported a reduced number of patients with worsening myocardial function 3 years and 5 years later and an increased 10-year survival. Jefferies, et al.
17 suggested that ACEi and/or beta-blockers should be recommended as soon as echocardiographic abnormalities are found, which, as they demonstrated, helped to improve LV dilatation and systolic functional alteration at the 1-year follow up.
These results of myocardial strain analysis by cardiac layer show that it is a promising method for detecting subtle myocardial dysfunction earlier to enable timely cardiac treatment, which would improve cardiac function and prognosis in patients with DMD.
Given the paucity of myocardial strain evaluation in DMD child patients, this study presents very significant information for assessing cardiac function via feasible analysis.
In conclusion, in patients with DMD, myocardial circumferential deformation can deteriorate earlier, even with well-preserved longitudinal function. This might be an early diagnostic indicator for myocardial involvement in predicting the progress of cardiomyopathy, which could enable optimal treatment for myocardial survival in patients with DMD.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download