Abstract
Purpose
Clinical outcomes and radiologic results after cervical arthroplasty have been reported in many articles, yet relatively few studies after cervical arthroplasty have been conducted in severe degenerative cervical disc disease.
Materials and Methods
Sixty patients who underwent cervical arthroplasty (Mobi-C®) between April 2006 and November 2011 with a minimum follow-up of 18 months were enrolled in this study. Patients were divided into two groups according to Pfirrmann classification on preoperative cervical MR images: group A (Pfirrmann disc grade III, n=38) and group B (Pfirrmann disc grades IV or V, n=22). Visual analogue scale (VAS) scores of neck and arm pain, modified Oswestry Disability Index (mODI) score, and radiological results including cervical range of motion (ROM) were assessed before and after surgery.
Results
VAS and mean mODI scores decreased after surgery from 5.1 and 57.6 to 2.7 and 31.5 in group A and from 6.1 and 59.9 to 3.7 and 38.4 in group B, respectively. In both groups, VAS and mODI scores significantly improved postoperatively (p<0.001), although no significant intergroup differences were found. Also, cervical dynamic ROM was preserved or gradually improved up to 18 months after cervical arthroplasty in both groups. Global, segmental and adjacent ROM was similar for both groups during follow-up. No cases of device subsidence or extrusion were recorded.
In degenerative cervical disc disease, anterior cervical decompression and fusion have been widely performed in those unresponsive to conservative treatment; however, fusion surgery may lead to loss of range of motion (ROM) of the cervical spine and accelerate adjacent cervical disc degeneration.1,2,3,4 Therefore, cervical arthroplasty has been increasingly adopted as an alternative to fusion surgery, because, theoretically, it maintains cervical spine ROM and prevents degeneration of adjacent segments.5,6,7,8 For this reason, cervical arthroplasty has usually been performed in cases of mild degenerative cervical disc disease. On the other hand, anterior cervical decompression and fusion are still considered classic methods for managing severe degenerative cervical disc disease, despite reports of marked reductions in ROM of the cervical spine.2,9 Although many authors have reported on clinical outcomes and radiologic results after cervical arthroplasty, few have addressed these issues in severe degenerative cervical disc disease.10,11,12 As a result, no direct comparative study has been undertaken to assess the results of cervical arthroplasty in relation to the severity of disc degeneration. In the present study, we retrospectively compared clinical and radiological results after cervical arthroplasty in patients with mild disc degeneration to those in patients with moderate to severe disc degeneration.13
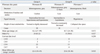
Sixty patients that underwent single-level cervical arthroplasty from C3 to C7 from April 2006 to November 2011 with a minimum follow-up of 18 months were identified. After obtaining Institutional Review Board approval (MD-Scholar-12-03), 35 men and 25 women were enrolled in the present study. The patients' ages at the time of surgery ranged from 24 to 59 years (mean 42.7 years). All patients had a history of radiculopathic or myelopathic symptoms refractory to conservative treatment for a minimum of 6 weeks (mean duration 13.3 months, range 1.5-120 months). Preoperative signs and symptoms consisted of radiculopathy in 36 patients (60%), myelopathy in 9 patients (15%), and combined radiculopathy and myelopathy in 15 patients (25%). Cervical disc degeneration was graded by a neuroradiologist using the Pfirrmann classification based on analyses of preoperative cervical MR images. Pfirrmann classification is useful in assessing degrees of disc degeneration on T2-weighted images: Grade 1 (normal shape, no horizontal bands, clear distinction of nuclei and annuli), Grade 2 (non-homogeneous shape with horizontal bands, some blurring between nuclei and annuli), Grade 3 (non-homogeneous shape with blurring between nuclei and annuli, annuli shape still recognizable), Grade 4 (non-homogeneous shape with hypointensity, annuli shape not intact and distinction between nuclei and annuli impossible, disc height usually decreased), and Grade 5 (same as Grade 4, but with collapsed disc space). Grades 1 to 2 were classified as normal discs, while grades 3 to 5 were defined as degenerative.13,14 In this study, all patients were divided into two groups, namely, group A (Pfirrmann grade III) and group B (Pfirrmann grade IV or V) (Table 1, Fig. 1). Thirty-eight patients were of Pfirrmann grade III, 18 patients were of Pfirrmann grade IV, and four were of Pfirrmann grade V. All surgical procedures were performed by a single neurosurgeon using the same protocol.
The surgical indications consisted of intractable pain treatment, as well as radiculopathy and myelopathy with compatible MR image findings. Inclusion criteria were single level degenerative disc disease between C3-C4 and C6-C7 in patients with radiculopathy or myelopathy not responsive to conservative treatment. Cases of predominantly anterior compression of the cervical spinal cord or nerve roots were considered good candidates. Exclusion criteria included infection, metabolic bone disease, neoplastic disease, severe kyphosis and osteoporosis. Target levels were consecutive in all cases [i.e., C3-C4 (n=2), C4-C5 (n=8), C5-C6 (n=35), and C6-C7 (n=15)]. The exclusion criteria that were applied included cases of facet syndrome, cervical stenosis caused by posterior compression, deformity, osteoporosis, and infection.
A standard Smith-Robinson approach was used to expose treatment levels in all patients,15 and the surgical technique used was basically the same in both groups. The cartilaginous endplate was removed with a curette taking caution not to damage the bony endplate. Uncovertebral joints were partially removed. An artificial disc (Mobi-C® disc; LDR Medical, Troyes, France) was used for cervical arthroplasty. This disc prosthesis comprises of a 3-piece, biarticulating, metal on polyethylene, semiconstrained device,16 consisting of two metal base plates with an ultra-high molecular weight polyethylene insert. This insert is said by the manufacturer to utilize mobile-bearing technology that improves ROM. Two lateral stops on the inferior endplate limit movement of the insert. Furthermore, this artificial disc has received approval from the Food and Drug Administration to undergo an Investigational Device Exemption trial in the United States.
Clinical evaluations were performed by a nurse, who is specially trained in pain management and was unaware of treatment details, utilizing the visual analogue scale (VAS) of neck and arm pain, as well as the modified Oswestry Disability Index (mODI: questions concerning sex life were excluded).17 Patients were asked to check mODI and VAS before surgery and at 1, 6, 12, and 18 months postoperatively. The mODI scores varied from 0 to 45, and mODI results were transformed to a scale ranging from 0% (no disability) to 100% (maximum disability). Pain intensities were rated from 0 to 10 using a subjective numerical rating scale (VAS; 0=no pain; 10=worst pain imaginable).
Cervical dynamic lateral radiography was performed preoperatively and at 1, 6, 12, and 18 months postoperatively to determine the ROM of global, treated, and adjacent segments. The angles on cervical dynamic lateral radiographs were recorded by two different neurosurgeons, independently from each other. If the recorded measurement of an angle differed between physicians (for more than 5 angles), the angle was rechecked and the median angle was selected. Sagittal alignments were calculated using Cobb's angle method, and ROM of the cervical spine was defined as the difference between Cobb's angles in full flexion and extension (Fig. 2). The global segment was bounded by lines drawn at the inferior margin of the C2 vertebral body and at the inferior margin of the C7 vertebral body. Global ROM was defined as the difference between Cobb's angles in full flexion and extension in the global segment. To analyze the ROM of a diseased segment, the treated segment angle formed by lines drawn at the superior margin of the superior vertebral body and at the inferior margin of inferior vertebral body was measured, and segment ROM was defined as the difference between Cobb's angles in full flexion and extension in the treated segment. Adjacent segment angle was also measured to assess adjacent segment degeneration, and was defined as the angle formed by a line drawn at the superior margin of the upper level vertebral body of the treated segment and by a line drawn at the inferior margin of the lower level vertebral body of the subject adjacent segment. Adjacent segment ROM was defined as the difference between the Cobb's angles of adjacent segments in full flexion and extension. Lower adjacent ROM was not checked in patients with cervical arthroplasty at level C6-C7, because the lower level margin was obscured on radiographs. Angles were measured using PACS solution software (Marosis-enterprise, Marotech, Seoul, Korea). Computed tomography was routinely performed at 12 months postoperatively to check for prosthesis subsidence or extrusion.
Results are expressed as means±standard deviations. The chi-square test, Student's t-test, and the paired t-test were used to determine significant differences in clinical and radiological variables in the two groups at each time point. SPSS software for Windows (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses, and statistical significance was accepted for all p-values <0.050.
A total of 60 patients were enrolled in this study: 38 Pfirrmann grade III patients (group A) and 22 Pfirrmann grade IV or V patients (group B). Table 1 summarizes the demographic data of the two groups. Average ages at surgery were similar between the two groups (p=0.473). Overall, 63% and 50% of the patients were male in groups A and B, respectively, and no significant difference was found in regards to gender ratios (p=0.327). Target levels were consecutive in 2 cases at C3-C4, 3 cases at C4-C5, 22 cases at C5-C6, and 11 cases at C6-C7 in group A, and in 5 cases at C4-C5, 13 cases at C5-C6, and 4 cases at C6-C7 in group B. Group level distributions were not statistically different (p=0.250). The mean follow-up periods were also similar between groups A and B (21.4 months, range 12-45 months vs. 22.6 months, range 12-36 months, respectively; p=0.545).
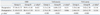
In group A, the average VAS score for neck pain decreased significantly (p<0.001), from a preoperative score of 5.13 to a postoperative score of 2.74, among the 38 patients followed for 18 months. Similarly, in group B, the average VAS score for neck pain decreased significantly B (p<0.001), from a preoperative score of 6.09 to a postoperative score of 3.68, for the 22 patients followed for 18 months (Table 2). Although group A showed greater improvements in postoperative VAS score than group B at 12 months, preoperative and postoperative VAS scores were not significantly different between the two groups (p=0.131 and 0.066, respectively). The average VAS scores of arm pain also decreased significantly (p<0.001) in both groups A and B at 18 months, from a preoperative score of 5.53 to a postoperative score of 2.44 months in group A and from a preoperative score of 5.92 to a postoperative score of 2.83 in group B. Nevertheless, preoperative and postoperative VAS scores of arm pain were not significantly different between groups A and B (p=0.314 and 0.136, respectively). As for the VAS results, in group A, the average mODI score decreased significantly (p<0.001), from a preoperative score of 57.58 to postoperative score of 31.45, for the 38 patients followed for 18 months (Table 2). Similarly, in group B average mODI score decreased significantly (p<0.001), from a preoperative score of 59.91 to a postoperative score of 38.41, for the 22 patients followed for 18 months. Although preoperative and postoperative mODI at 12 months were not significantly different between groups A and B (p=0.452 and 0.114, respectively), postoperative mODI improvement in group B was less than that in group A at 18 months.
The intraclass correlation between the two neurosurgeons who conducted the radiological analyses was found to be 0.910. Global ROM was 16.35 in group A and 18.10 in group B preoperatively, and respectively, 12.08 and 7.60 at 1 month, 16.07 and 13.24 at 6 months, 15.12 and 16.21 at 18 months postoperatively (Table 3). In both groups, global ROM significantly decreased at 1 month postoperatively (p<0.001), but gradual improvement and restoration to preoperative ROM levels were observed in both groups (final global ROM was not significantly different from preoperative ROM; p=0.186 and 0.161 for groups A and B). The only difference between global ROM in the groups was observed at 1 month postoperatively, and this was due to smaller improvements in group A (p=0.016). Segmental ROM preoperatively was 6.56 and 5.16 in groups A and B, respectively, and 4.78 and 4.20 at 1 month, 6.46 and 5.61 at 6 months, 6.59 and 6.41 at 18 months postoperatively. In group A, segmental ROM significantly decreased at 1 month postoperatively (p<0.001), but not in group B (p=0.134). Segmental ROM in both groups gradually improved and was restored to preoperative ROM levels. In fact, final segmental ROM was not significantly different from preoperative segmental ROM in group A (p=0.838); however, final segmental ROM in group B improved greatly compared with preoperative ROM (p=0.026). Upper adjacent ROM was 10.19 in group A and 10.64 in group B preoperatively, and respectively, 5.98 and 6.92 at 1 month, 9.70 and 9.56 at 6 months, 11.27 and 12.27 at 18 months postoperatively. In both groups, upper adjacent ROM was significantly poorer at 1 month postoperatively (p<0.001 and 0.009), but gradually improved and exceeded preoperative ROM, although without statistical significance (p=0.174 and 0.088). The lower adjacent ROM of 45 cases without C6-C7 involvement was 10.51 in group A and 9.80 in group B preoperatively, and respectively, 6.28 and 7.26 at 1 month, 10.17 and 9.91 at 6 months, 11.79 and 11.76 at 18 months postoperatively. In group A, lower adjacent ROM was significantly poorer at 1 month postoperatively (p<0.001), but this was not observed in group B (p=0.075). Gradual improvements to preoperative lower adjacent ROM levels were observed in both groups [final lower adjacent ROM was not significantly different from preoperative lower adjacent ROM (p=0.139 and 0.091 in group A and B, respectively)]. No device subsidence or extrusion was observed during the 12-month follow-up period on computed tomography. Other observed complications after anterior cervical arthroplasty included infection (n=1), hematoma (n=1), dysphagia (n=2) and fusion (n=2), but these were not significantly different according to Pfirrmann disc grade.
Fusion surgery may lead to a loss of ROM of the cervical spine and alter normal spinal biomechanics, which may result in the acceleration of adjacent cervical disc degeneration and the need for subsequent reoperation.2,4,14 Cervical disc prostheses are designed to maintain ROM of the cervical spine after anterior discectomy and preserve physiologic ROM, rather than fusing the degenerative spine, and this may limit the degenerative progression of adjacent segments.5,6 With the results of the first human trial on cervical prostheses reported in 1998, many authors have demonstrated that cervical arthroplasty offers beneficial effects on spinal biomechanics.10,1112,18 Cervical arthroplasty restores intervertebral disc and foraminal height, and eventually preserves ROM of the cervical spine, which results in an unchanged load distribution on the cervical spine.19 As a result, degenerative progression of an adjacent segment can be prevented, and reestablishment of cervical curvature aided.20 Thereby, complications related to anterior cervical decompression and fusion encourage the use of cervical arthroplasty as an alternative to fusion surgery.21,22,23,24,25,26 Nevertheless, many studies that have conducted radiographic follow-up review of patients treated by arthroplasty and fusion have demonstrated disappointing clinical results.27,28
On this basis, cervical arthroplasty has been restricted to patients with mild degenerative cervical disc disease with preoperatively preserved ROM of the cervical spine. Cervical arthroplasty can be readily applied in patients presenting with neurologic deficit, radiculopathy or myelopathy, as the surgical approach and anterior spinal cord decompression technique is identical to that for cervical disc replacement and traditional cervical decompression. Generally, cervical arthroplasty had been used in mild disc degeneration to preserve cervical motion. However, some studies included severe cervical spondylosis with radiculopathy and/or myelopathy.12,29,30 Indeed, in lumbar total disc replacement, a study based on the dataset of SWISSspine suggested that diagnoses of disc degeneration and radiculopathy might not be considered as absolute or relative contraindications for mono-segmental lumbar total disc replacement.31 Accordingly, we considered that cervical arthroplasty might be effective in cases of severe disc degeneration, because the implantation of an artificial disc can restore disc space and preserve the ROM of treated segments and, thus, that it might be preferable to fusion surgery from the perspective of spinal biomechanics. In the present study, we divided patients into two groups based on preoperative MRI disc grade, and performed clinical and radiological assessments of these groups to compare the outcomes of cervical arthroplasty with respect to degree of degeneration. The clinical outcomes recorded showed significant improvements relative to preoperative conditions in both groups. Nevertheless, preoperative and postoperative mODI scores were not significantly different in groups A and B; this result demonstrates the equivalent clinical efficacy of cervical arthroplasty in cases with mild/moderate or severe disc degeneration.
According to radiological assessments, group A showed no significant decrease in ROM at final follow-up, despite a significant temporary decrease at 1 month after surgery, and similar results were observed for global, segmental, and adjacent segments. Group B also showed no significant decrease in global or adjacent ROM at final follow-up; in fact, significant improvements in segmental ROM at final follow-up were observed in this group. Radiographic results showed that the ROM of treated segments was significantly poorer at 1 month postoperatively in groups A and B. This could have been the result of surgical site pain or patient non-compliance to movements as an early response to surgery. However, cervical ROM recovered to preoperative values at final follow-up in both groups with no significant intergroup difference. This result demonstrates the radiologic equivalence of cervical arthroplasty in cases of mild/moderate and severe disc degeneration. Indeed, our results indicated that cervical arthroplasty is more effective in terms of segmental ROM in cases with moderate to severe disc degeneration, as segmental ROM was found to be significantly improved.
In the present study, groups A and B showed no distinctive differences in terms of postoperative radiological or clinical outcomes. In fact, both groups achieved favorable radiological and clinical outcomes, with the exception of global ROM limitation at 1 month postoperatively in group B. Importantly, radiological and clinical outcomes in group B were not found to be inferior to those of group A, which suggests cervical arthroplasty might not only be effective in patients with mild disc degeneration.
A few limitations of this study warrant consideration. First, this study was designed as a retrospective case review series without any randomized control study. In fact, if the study were trying to prove the indication of cervical arthroplasty in patients with moderate to severe cervical disc degeneration, a prospective, controlled and randomized study comparing arthroplasty and fusion would have been an ideal study design. Second, this report included a small sample size, including only patients with single level disc disease, and the follow-up period was relatively too short for examining reoperation rates or for determining the rate of adjacent segment degeneration. As well, cervical disc grading using Pfirrmann classification is difficult because cervical discs have smaller annuli than lumbar discs. Nevertheless, despite these limitations, we performed cervical arthroplasty for patients with single level disc disease and showed favorable results, even in the moderate to severe disc disease group. This study may suggest cervical arthroplasty as another treatment strategy for patients with moderate to severe disc disease who are still only considered for anterior cervical decompression and fusion in modern medical paradigms. In the near future, large-scale studies with a longer follow-up duration are required to re-examine the effects of cervical arthroplasty in patients with severe disc degeneration, and this task has already been undertaken by our study group.
In conclusion, the clinical and radiological results of patients with severe degenerative cervical disc disease treated by cervical arthroplasty were no different from those of patients with mild degenerative disease at 18 months after surgery. Although larger-scale comparative studies of longer follow-up are needed to prove the efficacy of cervical arthroplasty in patients with severe disc degeneration, our findings suggest that cervical arthroplasty is equally effective in patients with mild or moderate to severe disc degeneration.
Figures and Tables
Fig. 1
Radiological illustration of representative cases from groups A and B. Cases of Pfirrmann grade III (A) were assigned to Group A, while cases of Pfirrmann grade IV (B) or V (C) were assigned to Group B. Follow-up images were taken at 12 months after operation.

Fig. 2
Radiological illustration of global and segmental cervical range of motion in dynamic lateral radiographs: (A) global cervical range of motion was defined as the angles formed between lines drawn parallel to the inferior margin of C2 vertebral body (white line) and the inferior margin of C7 vertebral body (black line); (B) segmental cervical range of motion was defined as the angle formed between a line drawn to the upper endplate of the most cranial vertebra (white dot line) and a line drawn to the lower endplate of the most caudal vertebra (black dotted line) at the prosthesis inserted level; (C) adjacent segmental cervical range of motion was defined as the angle formed between a line drawn to the upper endplate of the most cranial vertebra (white dot line) and a line drawn to the lower endplate of the most caudal vertebra (black dotted line) at the disc level above or below the Mobi-C® prosthesis.

References
1. Agrillo U, Faccioli F, Fachinetti P, Gambardella G, Guizzardi G, Profeta G. Guidelines for the diagnosis and management of the degenerative diseases of cervical spine. J Neurosurg Sci. 1999; 43:11–14.
2. Gore DR, Sepic SB. Anterior cervical fusion for degenerated or protruded discs. A review of one hundred forty-six patients. Spine (Phila Pa 1976). 1984; 9:667–671.
3. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958; 40-A:607–624.

4. Wigfield C, Gill S, Nelson R, Langdon I, Metcalf N, Robertson J. Influence of an artificial cervical joint compared with fusion on adjacent-level motion in the treatment of degenerative cervical disc disease. J Neurosurg. 2002; 96:1 Suppl. 17–21.

5. Anderson PA, Rouleau JP. Intervertebral disc arthroplasty. Spine (Phila Pa 1976). 2004; 29:2779–2786.

6. Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine. 2007; 6:198–209.

7. Park JH, Roh KH, Cho JY, Ra YS, Rhim SC, Noh SW. Comparative analysis of cervical arthroplasty using mobi-c(r) and anterior cervical discectomy and fusion using the solis(r)-cage. J Korean Neurosurg Soc. 2008; 44:217–221.

8. Yoon DH, Yi S, Shin HC, Kim KN, Kim SH. Clinical and radiological results following cervical arthroplasty. Acta Neurochir (Wien). 2006; 148:943–950.

9. Jacobs B, Krueger EG, Leivy DM. Cervical spondylosis with radiculopathy. Results of anterior diskectomy and interbody fusion. JAMA. 1970; 211:2135–2139.

10. Nabhan A, Ahlhelm F, Shariat K, Pitzen T, Steimer O, Steudel WI, et al. The ProDisc-C prosthesis: clinical and radiological experience 1 year after surgery. Spine (Phila Pa 1976). 2007; 32:1935–1941.
11. Sekhon LH. Cervical arthroplasty in the management of spondylotic myelopathy: 18-month results. Neurosurg Focus. 2004; 17:E8.

12. Wang Y, Zhang X, Xiao S, Lu N, Wang Z, Zhou M. Clinical report of cervical arthroplasty in management of spondylotic myelopathy in Chinese. J Orthop Surg Res. 2006; 1:13.

13. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001; 26:1873–1878.

14. Takatalo J, Karppinen J, Taimela S, Niinimäki J, Laitinen J, Sequeiros RB, et al. Association of abdominal obesity with lumbar disc degeneration--a magnetic resonance imaging study. PLoS One. 2013; 8:e56244.
15. Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999; 81:519–528.

16. Shin DA, Yi S, Yoon DH, Kim KN, Shin HC. Artificial disc replacement combined with fusion versus two-level fusion in cervical two-level disc disease. Spine (Phila Pa 1976). 2009; 34:1153–1159.

17. Kim DY, Oh CH, Yoon SH, Park HC, Park CO. Lumbar disc screening using Back Pain Questionnaires: Oswestry Low Back Pain Score, Aberdeen Low Back Pain Scale, and Acute Low Back Pain Screening Questionnaire. Korean J Spine. 2012; 9:153–158.

18. Cherubino P, Benazzo F, Borromeo U, Perle S. Degenerative arthritis of the adjacent spinal joints following anterior cervical spinal fusion: clinicoradiologic and statistical correlations. Ital J Orthop Traumatol. 1990; 16:533–543.
19. Chang UK, Kim DH, Lee MC, Willenberg R, Kim SH, Lim J. Changes in adjacent-level disc pressure and facet joint force after cervical arthroplasty compared with cervical discectomy and fusion. J Neurosurg Spine. 2007; 7:33–39.

20. Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001; 10:320–324.

21. Döhler JR, Kahn MR, Hughes SP. Instability of the cervical spine after anterior interbody fusion. A study on its incidence and clinical significance in 21 patients. Arch Orthop Trauma Surg. 1985; 104:247–250.
22. Hunter LY, Braunstein EM, Bailey RW. Radiographic changes following anterior cervical fusion. Spine (Phila Pa 1976). 1980; 5:399–401.

23. McGrory BJ, Klassen RA. Arthrodesis of the cervical spine for fractures and dislocations in children and adolescents. A long-term follow-up study. J Bone Joint Surg Am. 1994; 76:1606–1616.

24. Davis RJ, Kim KD, Hisey MS, Hoffman GA, Bae HW, Gaede SE, et al. Cervical total disc replacement with the Mobi-C cervical artificial disc compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled multicenter clinical trial: clinical article. J Neurosurg Spine. 2013; 19:532–545.

25. Chen Y, Wang X, Lu X, Yang H, Chen D. Cervical disk arthroplasty versus ACDF for preoperative reducible kyphosis. Orthopedics. 2013; 36:e958–e965.

26. Phillips FM, Lee JY, Geisler FH, Cappuccino A, Chaput CD, DeVine JG, et al. A prospective, randomized, controlled clinical investigation comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion 2-year results from the US FDA IDE clinical trial. Spine (Phila Pa 1976). 2013; 38:E907–E918.
27. Verma K, Gandhi SD, Maltenfort M, Albert TJ, Hilibrand AS, Vaccaro AR, et al. Rate of adjacent segment disease in cervical disc arthroplasty versus single-level fusion: meta-analysis of prospective studies. Spine (Phila Pa 1976). 2013; 38:2253–2257.

28. Yin S, Yu X, Zhou S, Yin Z, Qiu Y. Is cervical disc arthroplasty superior to fusion for treatment of symptomatic cervical disc disease? A meta-analysis. Clin Orthop Relat Res. 2013; 471:1904–1919.

29. Goffin J, van Loon J, Van Calenbergh F, Lipscomb B. A clinical analysis of 4- and 6-year follow-up results after cervical disc replacement surgery using the Bryan Cervical Disc Prosthesis. J Neurosurg Spine. 2010; 12:261–269.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download