Abstract
Purpose
During carotid angioplasty and stenting (CAS), hemodynamic instability (HDI) can occur, possibly causing post-procedural ischemic complications. The goal of this study was to investigate the risk factors of HDI focusing on characteristics of plaque.
Materials and Methods
Thirty nine CAS patients were retrospectively evaluated for HDI. Prolonged HDI that lasted over 30 minutes was analyzed in relation to characteristics of calcified plaque.
Results
Nineteen (48.7%) patients had HDI. Ten of the 19 had both bradycardia and hypotension, and nine had only bradycardia. All bradycardia was treated well with a transcutaneous temporary cardiac pacemaker. But eight patients presented with prolonged hypotension in spite of recovery of bradycardia. Calcified plaque was a related factor associated with HDI (odds ratio, 8.571; 95% confidence interval, 1.321-55.62; p=0.024). Extensive and eccentric type calcified plaques were associated with prolonged hypotension (p=0.04, and p=0.028, respectively).
Carotid angioplasty and stenting (CAS) are a widely accepted procedure due to its simplicity and noninvasiveness.1-3 However, because of anatomical closeness of the procedure to the carotid sinus, hemodynamic instability (HDI) can occur during the procedure. Many studies have been performed to determine the risk factors of HDI.4-12 Nevertheless, most of the studies failed to clearly show the relationship between calcified plaques and hemodynamic instability.
The goal of this study was to investigate the risk factors of HDI focusing on characteristics of plaque.
This study was approved by the local ethical committee. This retrospective analysis was performed in patients who had CAS from January 2007 to April 2011 at a single center. A total of 48 patients underwent CAS during this period. Seven procedures were performed under emergent situations due to rapid progression of a stroke, one case was lost to follow-up after the CAS, and one CAS was conducted in a patient with general anesthesia due to irritability. These cases were excluded from the study, and a total of 39 patients were included in this analysis.
HDI was defined as systolic blood pressure <90 mm Hg or heart rate <50 beats/min (bpm).13 Prolonged HDI was defined as HDI lasting over 30 min. Stenosis was calculated by the NASCET14 method. Before the procedure, patient's neurological conditions were recorded with a NIHSS score, and fluid status, vital signs, and medical history, including the presence of hyperlipidemia, hypertension (HTN), diabetes mellitus (DM), systemic coagulopathy, and coronary artery disease, were recorded. Preprocedural radiologic tests were conducted with carotid computed tomography (CT), duplex ultrasound, angio-CT and magnetic resonance angiography to evaluate the plaque characteristics and confirm the stenotic lesions.
Plaques were categorized into three longitudinal groups; extensive, proximal, and distal. Extensive plaque included both sides of carotid bifurcation within 5 mm. Proximal plaque and distal plaque included internal carotid artery (ICA) within 5 mm and beyond 5 mm from the bifurcation, respectively (Fig. 1).15 A calcified plaque was defined as a structure with a density exceeding 130 Hounsfield units within the vessel wall that was hyperdense to the contrast-enhanced lumen and surrounding parenchyma on axial carotid CT.16 Calcified plaques were divided into two groups, based on symmetry (eccentric versus concentric) on axial images (Fig. 2), and eccentric plaques were subdivided into two categories, anterior wall versus posterior wall.12 Every radiologic finding was recorded by two qualified endovascular neurosurgeons and the discrepancies were reevaluated by third reader.
Before the procedure, all patients took oral aspirin (100 mg) and clopidogrel (75 mg) for more than 7 days. While patients were in a fasting state, each procedure was conducted under local anesthesia through a trans-femoral approach with an elective schedule. Each patient had a percutaneous cardiac pacing patch set at 50 bpm/20 mA to control bradycardia.17 Electrocardiogram, blood pressure, and blood oxygen saturation levels were continuously checked, and intravenous fluids and dopamine were prepared to respond to HDI. Drugs, such as atropine, diazepam, nicardipine, and pain relievers, were also prepared. During each step of the procedure, neurological changes and respond to HDI were evaluated.
After a 6-F guiding sheath was introduced, 3000-4000 units of heparin were administered intravenously. During the procedure, the heparin-mixed fluid was injected (1000 units of heparin in 1L sodium chloride solution) continuously to flush the catheter. After a roadmap was established, a Spider FX cerebral protection device (ev3 Endovascular, Inc., Plymouth, MN, USA) or FilterWire EZ device (Boston Scientific Corporation, Natick, MA, USA) was applied distally to the stenotic lesion. An Amiia or Aviator balloon catheter (Cordis Corporation, Miami, FL, USA) was used for pre-stent dilatation at nominal atmosphere (ATM) in the cases in which dilatation was needed. A PRECISE-RX (Cordis Corporation, Miami, FL, USA) or PROTÉGÉ (ev3 Endovascular, Inc., Plymouth, MN, USA) stent was applied at the stenotic segment. Post-stent balloon dilatations were used in only two patients. Every angiogram was conducted with the Artis zee Biplane system (Siemens, Forchheim, Germany). After the procedure, patients were closely observed in the intensive care unit for 24 h.
Continuous data are presented as the median±standard deviation. A Fisher's exact test was used to compare the discrete variables, and a Mann-Whitney U test was conducted to compare the unpaired continuous data. A binary logistic regression model was used to determine the risk factors of HDI induced by hypotension and bradycardia. The results of the logistic regression model were presented as odds ratios (OR), 95% confidence intervals (95% Cl), and p-values. p-values <0.05 were regarded as statistically significant. Statistics were performed with SPSS version 12 (SPSS, Chicago, IL, USA).
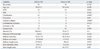
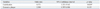
Thirty-nine patients (70.2±8.5 years) were examined. These patients were mostly male (n=32, 82.1%), and the majority had symptomatic lesions (n=25, 64.1%). Stenosis value was 79.4±6.6. Nineteen of the 39 patients had HDI due to hypotension or bradycardia during and after CAS. Prolonged HDI lasting over 30 min occurred in eight patients. The vital signs of transient HDI were normalized in an average of 7.8 min after development (range, 0.5-24 min). Bradycardia occurred in 19 patients, hypotension occurred in 10 patients, and both occurred in 10 patients. All bradycardia recovered well within 30 min with the use of a transcutaneous temporary cardiac pacemaker.17 All patients with hypotension were treated by intravenous fluid replacement, and eight patients received dopamine which was started at a dosage of 5 µg/kg/min. Among them, systolic pressure normalized in two patients 24 h after onset. The demographic and clinical characteristics of the 39 patients are shown in Table 1. The results revealed that calcified plaques and extensive plaque from carotid bulb to common carotid artery (CCA) were associated with HDI due to hypotension and bradycardia (p=0.001 and p=0.006, respectively). Other risk factors including age, coronary artery disease, HTN, ulceration of the plaque, maximal ATM used for ballooning, degree of diameter, and length of the stent and balloon did not differ significantly. A binary logistic regression model was used to determine the risk factors of HDI (Table 2). The presence of calcified plaque was an only significant predictable factor of HDI (OR, 8.571; 95% CI, 1.321-55.62; p=0.024)
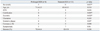
Prolonged HDI was found in eight patients. Each prolonged HDI was caused by hypotension, despite recovery of heart beats to over 60 bpm. A calcified plaque was found in eight patients with prolonged HDI and four patients with transient HDI (p=0.005). Eccentric calcified plaques were found in eight patients with prolonged HDI and two patients with transient HDI (p=0.028) (Table 3), and most (n=8) were posterior. There were no neurological and hemodynamic complications after CAS at this institution due to proper treatment without delay.
HDI can occur during CAS due to its close location to baroreceptors. When stretch receptors located in carotid sinus are activated during inflation of balloon or deployment of stent, activation of nerve fibers to the nucleus tracts solitaries through the glossopharyngeal nerve can occur, which causes the vague nerve to stimulate the parasympathetic pathway to the cardiac nodes. The results can be lowered heart rate and reduced peripheral resistance.18,19 HDI can lead to permanent or transient adverse effects. Minor neurological problems such as transient ischemic attacks and serious complications such as acute renal failure, myocardial infarctions (MI), intra-cerebral hemorrhages, and cerebral ischemia have been reported.20,21
Many studies have been performed to reveal risk factors that contribute to the development of HDI. These HDI risk factors have been grouped into three sectors by their radiological findings, combined underlying diseases, and demographic characteristics. Radiological findings included lesions involving the carotid bulb, isolated ICA lesion near the carotid bulb, the right side of CAS, ulceration or calcification of the plaque, eccentric posterior carotid plaque, and the presence of a contra-lateral occlusion.22 Combined underlying diseases included coronary artery disease,9 major or minor strokes, DM, HTN, hyperlipidemia, and a previous history of carotid endarterectomy. Demographic characteristics involved male or female gender,11 old age,9 and the presence of symptoms.4-6,22,23 General anesthesia is also related to the development of HDI.22
Most studies have focused on finding contributory risk factors to HDI. Transient HDI can be treated well without complications. Thus, more emphasis has to be put on prolonged HDI due to its greater chance of causing complications such as cerebral infarction, renal failure, and MI. Intraprocedural hypotension has been suggested as a predictor of persistent hypotension.11,24 Nonaka, et al.12 reported that distance from carotid bifurcation to maximal stenotic lesion and eccentric type stenois on angiogram and fibrous plaque and combined calcification on ultrasonogram are related to prolonged hypotension lasting more than 3 h. However, ultrasonography is not always an exact means of revealing characteristics of plaques. Furthermore, echogenicity of plaque and calcification of plaque with ultrasonogram may be overlapped.12
The present study is different from previous studies in two aspects. First, location of plaque was categorized by including the CCA near to carotid bifurcation or only carotid bulb longitudinally. Many studies reported that lesion with carotid bulb is a risk factor for HDI. Although, a high density of baroreceptors is found in the wall of ICA just above the carotid bifurcation, baroreceptors are also located in CCA near to the carotid bifurcation.25,26 This may imply that more extensive plaque that is located from carotid bulb to CCA is vulnerable to the development of HDI. Second, calcification of plaque was described in detail by the eccentricity of the plaque. Baroreceptors are stretch receptors and their activation is affected by the rate of increasing pressure and degree of pressure. Thus, uneven pressure may be transmitted to baroreceptors and its increasing inflation rate may be different in the presence of eccentric calcified plaque during arterial distension.
The development of hypotension can be explained by decreased cardiac output due to bradycardia and venous return due to decrease in peripheral resistance. Among patients with prolonged hypotension, some characteristics of plaque were related. Eccentric calcified plaque was associated to prolonged hypotension (p=0.028) and extensive plaque that covered from CCA to carotid sinus was also related to the development of prolonged hypotension (p=0.04).
Reducing sudden and high activation of baroreceptors is a key factor in lowering the incidence of HDI and its complications. Therefore, when extensive plaque is found with eccentric calcified plaque, another strategy is needed, such as suboptimal expansion at a slow rate and preventive measures to increase venous return. Suboptimal distension of stenotic lesion was suggested in some studies. Setacci, et al.27 reported the benefit of cutting-balloon angioplasty for the treatment of highly calcified de novo stenotic lesions, and Jin, et al.28 reported good results for suboptimal pre-stent balloon angioplasty without post-stent balloon dilatation. The preventive measures for increasing venous return may be done with enough intravenous fluid administration before and during the procedure and apply of compression stocking in high risk patients.
In conclusion, HDI can occur during and after CAS, and transient HDI can be treated well with transcutaneous temporary cardiac pacemaker, fluid replacement and inotrophic agents without complication. When extensive plaque combined with eccentric calcification is found, however, more caution is required and another treatment plan is needed to prevent prolonged HDI.
Figures and Tables
Fig. 1
The classification of plaque on distribution of longitudinal image. (a) Extensive plaque located from CCA to ICA within 5 mm from bifurcation (arrow) on both sides. (b) Proximal plaque included ICA within 5 mm from bifurcation. (c) Distal plaque included ICA beyond 5 mm from bifurcation. CCA, common carotid artery; ICA, internal carotid artery.

Fig. 2
Carotid CT and Dyna-CT show the classification of calcified plaque on distribution of cross-sectional image. (A) Eccentric calcified plaque. (B) Concentric calcified plaque.

Notes
References
1. Dietz A, Berkefeld J, Theron JG, Schmitz-Rixen T, Zanella FE, Turowski B, et al. Endovascular treatment of symptomatic carotid stenosis using stent placement: long-term follow-up of patients with a balanced surgical risk/benefit ratio. Stroke. 2001. 32:1855–1859.

2. Brown MM, Venables G, Clifton A, Gaines P, Taylor RS. Carotid endarterectomy vs carotid angioplasty. Lancet. 1997. 349:880–881.

3. Brooks WH, McClure RR, Jones MR, Coleman TL, Breathitt L. Carotid angioplasty and stenting versus carotid endarterectomy for treatment of asymptomatic carotid stenosis: a randomized trial in a community hospital. Neurosurgery. 2004. 54:318–324.

4. Schulz UG, Rothwell PM. Sex differences in carotid bifurcation anatomy and the distribution of atherosclerotic plaque. Stroke. 2001. 32:1525–1531.

5. Cayne NS, Faries PL, Trocciola SM, Saltzberg SS, Dayal RD, Clair D, et al. Carotid angioplasty and stent-induced bradycardia and hypotension: impact of prophylactic atropine administration and prior carotid endarterectomy. J Vasc Surg. 2005. 41:956–961.

6. Dangas G, Laird JR Jr, Satler LF, Mehran R, Mintz GS, Larrain G, et al. Postprocedural hypotension after carotid artery stent placement: predictors and short- and long-term clinical outcomes. Radiology. 2000. 215:677–683.

7. Harrop JS, Sharan AD, Benitez RP, Armonda R, Thomas J, Rosenwasser RH. Prevention of carotid angioplasty-induced bradycardia and hypotension with temporary venous pacemakers. Neurosurgery. 2001. 49:814–820.

8. Howell M, Krajcer Z, Dougherty K, Strickman N, Skolkin M, Toombs B, et al. Correlation of periprocedural systolic blood pressure changes with neurological events in high-risk carotid stent patients. J Endovasc Ther. 2002. 9:810–816.

9. Mlekusch W, Schillinger M, Sabeti S, Nachtmann T, Lang W, Ahmadi R, et al. Hypotension and bradycardia after elective carotid stenting: frequency and risk factors. J Endovasc Ther. 2003. 10:851–859.

10. Pappadà G, Beghi E, Marina R, Agostoni E, Cesana C, Legnani F, et al. Hemodynamic instability after extracranial carotid stenting. Acta Neurochir (Wien). 2006. 148:639–645.

11. Qureshi AI, Luft AR, Sharma M, Janardhan V, Lopes DK, Khan J, et al. Frequency and determinants of postprocedural hemodynamic instability after carotid angioplasty and stenting. Stroke. 1999. 30:2086–2093.

12. Nonaka T, Oka S, Miyata K, Mikami T, Koyanagi I, Houkin K, et al. Prediction of prolonged postprocedural hypotension after carotid artery stenting. Neurosurgery. 2005. 57:472–477.
13. Cieri E, De Rango P, Maccaroni MR, Spaccatini A, Caso V, Cao P. Is haemodynamic depression during carotid stenting a predictor of peri-procedural complications? Eur J Vasc Endovasc Surg. 2008. 35:399–404.

14. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1991. 325:445–453.
15. Uwatoko T, Toyoda K, Inoue T, Yasumori K, Hirai Y, Makihara N, et al. Carotid artery calcification on multislice detector-row computed tomography. Cerebrovasc Dis. 2007. 24:20–26.

16. Nandalur KR, Baskurt E, Hagspiel KD, Finch M, Phillips CD, Bollampally SR, et al. Carotid artery calcification on CT may independently predict stroke risk. AJR Am J Roentgenol. 2006. 186:547–552.

17. Im SH, Han MH, Kim SH, Kwon BJ. Transcutaneous temporary cardiac pacing in carotid stenting: noninvasive prevention of angioplasty-induced bradycardia and hypotension. J Endovasc Ther. 2008. 15:110–116.

18. Chalmers J, Pilowsky P. Brainstem and bulbospinal neurotransmitter systems in the control of blood pressure. J Hypertens. 1991. 9:675–694.

19. Mangin L, Medigue C, Merle JC, Macquin-Mavier I, Duvaldestin P, Monti A, et al. Cardiac autonomic control during balloon carotid angioplasty and stenting. Can J Physiol Pharmacol. 2003. 81:944–951.

20. Leisch F, Kerschner K, Hofman R, Bibl D, Engleder C, Bergmann H. [Carotid stenting: acute results and complications]. Z Kardiol. 1999. 88:661–668.
21. Morrish W, Grahovac S, Douen A, Cheung G, Hu W, Farb R, et al. Intracranial hemorrhage after stenting and angioplasty of extracranial carotid stenosis. AJNR Am J Neuroradiol. 2000. 21:1911–1916.
22. Taha MM, Toma N, Sakaida H, Hori K, Maeda M, Asakura F, et al. Periprocedural hemodynamic instability with carotid angioplasty and stenting. Surg Neurol. 2008. 70:279–285.

23. Wong JH, Findlay JM, Suarez-Almazor ME. Hemodynamic instability after carotid endarterectomy: risk factors and associations with operative complications. Neurosurgery. 1997. 41:35–41.

24. Mendelsohn FO, Weissman NJ, Lederman RJ, Crowley JJ, Gray JL, Phillips HR, et al. Acute hemodynamic changes during carotid artery stenting. Am J Cardiol. 1998. 82:1077–1081.

25. Fadel PJ. Arterial baroreflex control of the peripheral vasculature in humans: rest and exercise. Med Sci Sports Exerc. 2008. 40:2055–2062.
26. Fadel PJ, Ogoh S, Keller DM, Raven PB. Recent insights into carotid baroreflex function in humans using the variable pressure neck chamber. Exp Physiol. 2003. 88:671–680.

27. Setacci F, Sirignano P, de Donato G, Chisci E, Galzerano G, Iacoponi F, et al. Carotid highly-calcified de novo stenosis and cutting-balloon angioplasty: a tool to prevent haemodynamic depression? J Cardiovasc Surg (Torino). 2009. 50:357–364.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download