Abstract
Cerebral salt wasting is characterized by inappropriate natriuresis and volume contraction with associated cerebral pathology. It is distinct from the syndrome of inappropriate antidiuretic hormone secretion, which is characterized by inappropriate retention of free water. We report a patient with a porencephalic cyst who developed cerebral salt wasting. His initial treatment was supplementation of water and salt, which did not improve natriuresis or volume contraction. Fludrocortisone administration effectively managed the cerebral salt wasting.
Hyponatremia is a common complication of surgery and intracranial afflictions including injury, tumor, infection, and stroke.1 Neurological dysfunction resulting from cerebral edema is the principal manifestation of hyponatremia. The causes of hyponatremia should be evaluated in order to distinguish cerebral salt wasting (CSW) from syndrome of inappropriate secretion of antidiuretic hormone (SIADH), since the treatments for the two conditions are very different.1,2 CSW is defined as the renal loss of sodium leading to hyponatremia and extracellular fluid volume loss.3 Water and salt supplementation is the primary therapy for CSW, whereas water restriction is the primary treatment for SIADH.4 In the literature, it has been noted that mineralocorticoid administration is also of benefit in CSW cases.5-10 In the present case, a 17-year-old male patient was diagnosed with CSW and was managed effectively with fludrocortisone.
A 17-year-old boy was admitted to our hospital with the chief complaint of poor oral intake and general weakness on admission. He had been previously admitted at seven months of age for delayed development, increased head circumference, and the inability to make eye contact. Computed tomography at that time revealed a porencephalic cyst in the left parieto-occipital and right frontal area, agenesis of the corpus callosum, and absence of a septum pellucidum (Fig. 1). Electroencephalography illustrated an extremely dynamic background voltage suppression in the left hemisphere. Cysto-parietal shunt surgery was performed, and anticonvulsant medications were prescribed due to a diagnosis of Lennox-Gastaut syndrome. Approximately 5 months prior to the presently reported admission, he was admitted to our hospital with the same symptoms and recovered after fluid replacement. On his most recent admission, the chief complaint was poor oral intake and general weakness. His lips and tongue were dried because he had little oral intake of food and fluid for 15 days. His serum sodium level was 131 mEq/L, potassium was 3.3 mEq/L, chloride was 91 mEq/L, urine sodium was 87 mEq/L, and his urine specific gravity was 1.025. The serum blood urea nitrogen level was 57.2 mg/dL, uric acid was 5.6 mg/dL, and creatinine was 1.28 mg/dL. Initial vital signs showed a blood pressure of 95/62 mm Hg, heart rate of 136/min, and a urine output of 3.1 mL/kg/hr. This volume was replaced with intravenous fluid containing sodium chloride. However, excessive urine output continued and increased up to 5.1 mL/kg/hr. Although the urine sodium level and volume were not normalized, his serum sodium level increased to 134 mEq/L after sodium chloride infusion. Hormone levels from the laboratory test were as follows: antidiuretic hormone (ADH) level of 5.55 pg/mL, renin level of 3.48 ng/mL/hr, aldosterone level of 154.2 pg/mL, and a cortisol level of 164.94 ng/mL. Renal ultrasonography was performed, and both kidneys did not show any abnormal findings. We then started fludrocortisone 2.5 µg/kg every 12 hours for two days, but the patient did not respond to the treatment. His blood pressure increased to 111/81 mm Hg, and his heart rate was stabilized at 95/min. His serum sodium level further decreased to 130 mEq/L, while his chloride level decreased to 94 mEq/L, his osmolality to 270 mOsm/kg, and his urine sodium level to 62 mEq/L. The fludrocortisone dose was then increased to 3.75 µg/kg every 12 hours. Urine output, urine sodium, and serum sodium levels were improved. After administration of fludrocortisone for five days, the patient's serum sodium level returned to 141 mEq/L, while his urine sodium returned to 75 mEq/L, specific gravity to 1.015, urine osmolality to 501 mOsm/L, and serum osmolality to 287 mOsm/L (Fig. 2). The patient's serum blood urea nitrogen level thereafter was 10.2 mg/dL, and his creatinine level was 0.53 mg/dL. The patient was discharged with instructions to continue the medication.
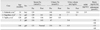
CSW is characterized by hyponatremia, excessive natriuresis, as well as volume depletion and generally occurs in patients with cerebral injury, tumor, infection or stroke.1 Water and salt replacement is the primary management for CSW, and the mechanism and treatment thereof are completely distinct from those of SIADH.3 An incorrect diagnosis can lead to inappropriate fluid restriction which may worsen the hypovolemia. Clinicians must distinguish CSW from SIADH by reviewing the clinical features and laboratory findings (Table 1). The key feature of CSW is a negative sodium balance, resulting in hyponatremia and extracellular fluid volume contraction.4 In contrast, SIADH involves inappropriate secretion of ADH or increased renal sensitivity to ADH, leading to renal conservation of water and euvolemic or hypervolemic hyponatremia.5,7 Proper replacement of urine salt and water using 0.9% or 3% sodium chloride is the salient treatment for CSW.5 The clinical and laboratory status of patients with CSW may continue to be poor in spite of replacement of urine salt and water.
The lack of a response to hypertonic saline led us to try treatment with fludrocortisone. The administration of fludrocortisone to manage CSW was firstly reported in the 1980s in adults with head injury and in isolated cases.10 Use in pediatric cases has been reported sporadically (Table 2).
Fludrocortisone is a synthetic corticosteroid with moderate glucocorticoid potency and substantial mineralocorticoid potency.1 It is primarily used to replace the missing hormone aldosterone in various forms of adrenal insufficiencies including Addison's disease and the classic salt wasting form of congenital adrenal hyperplasia.
Infants with CSW may have very high mineralocorticoid requirements in the first few months of life, usually 0.1-0.3 mg daily in two divided doses but occasionally up to 0.4 mg daily, and often require sodium supplementation (sodium chloride, 1-3 g) in addition to the mineralocorticoid.3 Older infants and children are typically maintained with a 0.05-0.1 mg dose of fludrocortisones.3 Our patient demonstrated that fludrocortisone administration was effective for CSW treatment and refractory hyponatremia after intracranial surgery.
CSW is generally induced by surgery or infection and our patient's CSW was due to a porencephalic cyst. CSW was diagnosed in the present case by elevated urine osmolality and a history of intracranial disease. In addition, our patient had normal blood pressure, implying relatively normal effective circulating volume (ECV); however, ECV is often low in such cases, causing low blood pressure.
Considering the potential adverse effects of fludrocortisone, we initiated treatment with a low dose of 2.5 µg/kg twice a day. With no improvement observed over two days, we increased the fludrocortisone dose from 2.5 µg/kg to 3.75 µg/kg twice a day, which effectively corrected the hyponatremia. Fludrocortisone was used for three days after discharge, and follow-up at outpatient department was planned. However, the patient was lost to follow up. Although fludrocortisone has some adverse effects including sodium and water retention, hypokalemia, and high blood pressure, it can be considered as an appropriate alternative treatment in cases of CSW, similar to the case presented herein.
Figures and Tables
Fig. 1
The computed tomography shows a porencephalic cyst in the left parieto-occipital and right frontal areas, showing the inserted cysto-parietal shunt.

Fig. 2
(A) Changes in serum Na level following fludrocortisone use (mmol/L). (B) Changes in random urine Na level following fludrocortisone use (mmol/L). Na, sodium.

References
1. Rahman M, Friedman WA. Hyponatremia in neurosurgical patients: clinical guidelines development. Neurosurgery. 2009. 65:925–935.
2. Lee P, Jones GR, Center JR. Successful treatment of adult cerebral salt wasting with fludrocortisone. Arch Intern Med. 2008. 168:325–326.

3. Taplin CE, Cowell CT, Silink M, Ambler GR. Fludrocortisone therapy in cerebral salt wasting. Pediatrics. 2006. 118:e1904–e1908.

4. Betjes MG. Hyponatremia in acute brain disease: the cerebral salt wasting syndrome. Eur J Intern Med. 2002. 13:9–14.

5. Ozdemir H, Aycan Z, Degerliyurt A, Metin A. The treatment of cerebral salt wasting with fludrocortisone in a child with lissencephaly. Turk Neurosurg. 2010. 20:100–102.
6. Hegde RM. Cerebral salt wasting syndrome: a case report. Crit Care Resusc. 1999. 1:180–183.
7. Kinik ST, Kandemir N, Baykan A, Akalan N, Yordam N. Fludrocortisone treatment in a child with severe cerebral salt wasting. Pediatr Neurosurg. 2001. 35:216–219.

8. Sakarcan A, Bocchini J Jr. The role of fludrocortisone in a child with cerebral salt wasting. Pediatr Nephrol. 1998. 12:769–771.

9. Nagotkar L, Shanbag P, Dasarwar N. Cerebral salt wasting syndrome following neurosurgical intervention in tuberculous meningitis. Indian Pediatr. 2008. 45:598–601.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download