Abstract
Purpose
Accurate indications and the extent of surgery for branch duct intraductal papillary mucinous neoplasm (IPMN) of the pancreas are still debatable. In particular, small tumor is located at the head portion of pancreas presents a dilemma. The purpose of this study is to compare the efficacy of enucleation (EN) with that of pancreaticoduodenectomy (PD) in patients with small (2 cm<size<3 cm) branch duct IPMN located at the head of pancreas or uncinate process.
Materials and Methods
Among 155 patients who underwent pancreatic surgery due to pancreatic cystic tumors between January 2000 and December 2007 at Yonsei University Health System in Seoul, Korea, 14 patients with small (2 cm<size<3 cm) branch duct IPMN located at the head of pancreas or uncinate process were included in this study. Ten patients underwent PD, and four patients underwent EN. We compared short term surgical outcomes between the two groups. Correlation of the variables was analyzed using Mann-Whitney test and Fisher's exact test (SPSS Window 12.0). p-values less than 0.05 were considered significant.
Thanks to the development of diagnostic tools, intraductal papillary mucinous neoplasm (IPMN) of the pancreas has increasingly been detected in asymptomatic patients.1-3 A branch duct IPMN smaller than 3 cm should sometimes be considered as an indication for surgical resection, even though it is associated with a lower risk of malignancy.4 Since the malignant risk of small branch duct IPMNs is uncertain, it is difficult for surgeons to determine the treatment modality, especially if the lesion is located at the head of pancreas or uncinate process.
Possible surgical modalities for a branch duct IPMN at the pancreatic head include pancreaticoduodenectomy (PD), pylorus preserving PD (PPPD), duodenum preserving pancreatic head resection, and enucleation. PD is recommended whenever there is a doubt for the presence of malignant risks. However, it is difficult to accurately diagnose the presence of carcinoma in situ or invasive carcinoma for IPMN on preoperative imaging study. Thus, indications and extent of surgery for branch duct IPMN of the pancreas are still debatable. For branch duct IPMNs with a borderline risk of malignancy, a limited resection (duodenum preserving pancreatic head resection or enucleation) can be applied with less invasiveness. However, duodenum preserving pancreatic head resection is technically more demanding than PD. Numerous studies have examined the feasibility of surgical resection of a small branch duct IPMN, however, most of them have focused only on organ preserving pancreatic resection.5-7 We, therefore, compared the efficacy of enucleation with that of PD in patients with small (2 cm<size<3 cm) branch duct IPMN located at the head of pancreas and uncinate process.
This study, including the retrospective chart review and data collection, was approved by the Institutional Review Board of Yonsei University. We retrospectively reviewed 155 patients who underwent pancreatic surgery for cystic lesions in the pancreas between January 2000 and December 2007 at the Department of Surgery, Yonsei University College of Medicine.
Among these patients, 14 patients who had branch duct type IPMN at the pancreatic head and uncinate portion with sizes between 2 cm and 3 cm were selected for the study. Among them, 10 patients underwent PD or PPPD, and 4 underwent enucleation. In the enucleation group (EN group), the tumor was located away from the main pancreatic duct, not abutting to the main pancreatic duct and there was no mural nodule on imaging studies. We did not routinely perform Endoscopic Ultrasonography Fine Needle Aspiration. We determined surgery and the type of surgery according to tumor size, presence of mural nodule, and distance between tumor and main pancreatic duct (not abutting to the main pancreatic duct). Pathologic diagnoses were provided by an expert pathologist and all patients were closely followed until December 2008. All patients were followed up for more than 12 months, and the mean duration of follow up was 53.57 months (range: 12 to 129).
The patients were divided into two groups according to the type of surgery: PD group and EN group. The two groups were compared in terms of age, gender, size of tumor, pathology, short term surgical outcomes such as operation time, blood loss, length of hospital stay, complications, operative mortality, and tumor recurrence.
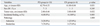
This study included 8 male and 6 female patients. Their average age was 62.21 years (±6.71 years). There was no significant difference in age, gender, size of tumor and pathology between the two groups (Table 1). However, tumor size was significantly larger in the EN group than the PD group.
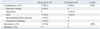
The mean operation time and intraoperative blood loss were significantly less in the EN group than the PD group. Both the length of hospital stay and time to normal intake of soft diet were shorter in the EN group, but there was no statistical significance (Table 2).
Postoperative complications occurred in 2 of 4 patients in the EN group, acute pancreatitis in 1 patient (amylasemia, no clinical symptoms) and delayed gastric emptying in 1 patient (Table 3). There was no operative mortality in either groups.
The average follow up period was 43.25 months (range: 12 to 112) in the EN group, and 57.70 months (range: 13 to 129) in the PD group. In the latter group, a single case with borderline IPMN lesions recurred in the remnant pancreas 96 months after PD. The patient refused surgery, and we decided to observe the lesions.
Pancreatic cystic lesions are increasingly identified due to several factors, including better quality of diagnostic tools, increasing routine physical check-ups, and increasing life span. Many studies correlating size and malignancy risk have revealed that small branch duct IPMNs are less likely to be malignant. A recent consensus conference recommended follow up every 3-6 months for lesions larger than 20 mm.8 However, based on results of a large-scale study on branch duct IPMNs in Korea,9 our institutional policy has been changed to perform surgical exploration for patients with lesions ≥2 cm in diameter. In this study, 1 patient (7.1%) had malignant lesions, which is in accordance with the results of other series that reported malignancy rates ranging between 6-46% in small branch duct IPMNs.8,9
Numerous factors are involved in deciding between surgical treatment or observation with routine radiologic check up for the management of small branch duct IPMN, such as the presence of mural nodule, tumor size, tumor location, age-specific life expectancy for benign cysts, and type of surgery. If the branch duct IPMN is located at the body or tail of the pancreas, there should be no hesitation in selecting a left side pancreatectomy with relatively low rate of morbidity than PD. A dilemma in selecting treatment modality arises if small branch IPMN lesions smaller than 3 cm are located at the head or uncinate process of pancreas. The natural course of small branch duct IPMN over time has not been well evaluated. Therefore, many surgeons have argued over an aggressive approach to the surgical management of pancreatic IPMNs. Recently, clinicians have recommended a more conservative approach.10 However, the malignancy potential of such lesions has been reported to range from 6% to 46%,11-19 which is much higher than the surgical mortality of PD in large volume centers.20-23 Therefore, we think that surgical resection is necessary for branch IPMN even if they are small in size and without clinical symptoms.
There are many operative procedures for the management of small branch duct IPMNs located at the pancreatic head. Possible surgical modalities include PD, PPPD, duodenum preserving pancreatic head resection, and enucleation. For branch duct IPMN with low risk of malignancy, limited resection such as duodenum preserving pancreatic head resection and enucleation can be applied with less invasiveness and organ preservation. However, duodenum preserving pancreatic head resection is technically more demanding than PD. Compared to major pancreas resection surgery, enucleation is advantageous in that it entails lower surgical mortality, lower morbidity and complication rates, shorter hospital stay, and earlier return to normal daily activity.24-28
However, enucleation has two major drawbacks: recurrence rate and injury of the main pancreatic duct. To avoid the injury of the main pancreatic duct, we inserted an endoscopic pancreatic stent before operation. There was no early endoscopic procedure-related complications except pancreatitis.
From an oncological point of view, complete frozen section biopsy of surgical margins is recommended for adequate surgical management.29 IPMNs should be re-resected if the operative margins are positive for malignancy. However, treatment for patients with margins positive for benign IPMN is controversial. In this study, only one case of recurrence was observed in the PN group. Because this recurrence occurred after definitive resection (R0 resection), one might assume that the transformation developed in the remnant pancreas. Misdiagnosis of an underlying IPMN could provide another explanation. The risk of developing a metachronous IPMN in a remnant pancreas is poorly elucidated. Nevertheless, we believe that this potential does not justify recommending total pancreatectomy for IPMN.
This study suggests that enucleation could be a safe and effective tool for surgical extirpation. Small branch duct IPMN of the pancreatic head using intra-operative frozen section biopsy to rule out a small foci of malignancy will permit enucleation as a acceptable mode of therapy.
In conclusion, it is controversial whether surgical treatment is needed for small branch duct IPMNs. However, there are some reasonable grounds for operation. It is not easy to preoperatively confirm a diagnosis and malignant potential of cystic tumors of the pancreas, and frequent follow up required for unconfirmed cystic lesions is socially-economically expensive. Moreover, there is a time dependent risk of malignant or invasive carcinoma throughout the adenoma-carcinoma sequence. This study suggests that enucleation for small (2 cm<size<3 cm) branch duct IPMNs at the pancreatic head portion in asymptomatic patients could be feasible, and as safe as PD, despite a high rate of minor complications. The procedure may yield accurate diagnosis in uncertain cases preoperatively and the ability to treat the disease when management is still possible before progression to invasive carcinoma. Since this study included a very limited number of enucleation cases, more experience and long term surveillance for enucleation group should be followed.
Figures and Tables
Table 1
Patient Characteristics according to Type of Operation on Small Branch Duct Intraductal Papillary Mucinous Neoplasms of the Pancreatic Head Portion
ACKNOWLEDGEMENTS
This article was presented at the 7th Congress of the European Hepato Pancreatic Biliary Association (EHPBA, 2009) in Athens, Greece on 18-20 June 2009.
References
1. Kiely JM, Nakeeb A, Komorowski RA, Wilson SD, Pitt HA. Cystic pancreatic neoplasms: enucleate or resect? J Gastrointest Surg. 2003. 7:890–897.

2. Fernández-del Castillo C, Targarona J, Thayer SP, Rattner DW, Brugge WR, Warshaw AL. Incidental pancreatic cysts: clinicopathologic characteristics and comparison with symptomatic patients. Arch Surg. 2003. 138:427–434.
3. Megibow AJ, Lombardo FP, Guarise A, Carbognin G, Scholes J, Rofsky NM, et al. Cystic pancreatic masses: cross-sectional imaging observations and serial follow-up. Abdom Imaging. 2001. 26:640–647.

4. Allen PJ, D'Angelica M, Gonen M, Jaques DP, Coit DG, Jarnagin WR, et al. A selective approach to the resection of cystic lesions of the pancreas: results from 539 consecutive patients. Ann Surg. 2006. 244:572–582.
5. Hung JS, Yang CY, Hu RH, Lee PH, Tien YW. Surgical treatment of pancreatic serous cystadenoma: aggressive for operations but limited resections. Pancreas. 2007. 35:358–360.

6. Beger HG, Gansauge F, Siech M, Schwarz M, Poch B. Duodenum-preserving total pancreatic head resection for cystic neoplastic lesions in the head of the pancreas. J Hepatobiliary Pancreat Surg. 2008. 15:149–156.

7. Beger HG, Rau BM, Gansauge F, Schwarz M, Siech M, Poch B. Duodenum-preserving total pancreatic head resection for cystic neoplasm: a limited but cancer-preventive procedure. Langenbecks Arch Surg. 2008. 393:589–598.

8. Tanaka M, Chari S, Adsay V, Fernandez-del Castillo C, Falconi M, Shimizu M, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006. 6:17–32.

9. Jang JY, Kim SW, Lee SE, Yang SH, Lee KU, Lee YJ, et al. Treatment guidelines for branch duct type intraductal papillary mucinous neoplasms of the pancreas: when can we operate or observe? Ann Surg Oncol. 2008. 15:199–205.

10. Le Borgne J, de Calan L, Partensky C. Cystadenomas and cystadenocarcinomas of the pancreas: a multiinstitutional retrospective study of 398 cases. French Surgical Association. Ann Surg. 1999. 230:152–161.
11. Lee SY, Lee KT, Lee JK, Jeon YH, Choi D, Lim JH, et al. Long-term follow up results of intraductal papillary mucinous tumors of pancreas. J Gastroenterol Hepatol. 2005. 20:1379–1384.

12. Terris B, Ponsot P, Paye F, Hammel P, Sauvanet A, Molas G, et al. Intraductal papillary mucinous tumors of the pancreas confined to secondary ducts show less aggressive pathologic features as compared with those involving the main pancreatic duct. Am J Surg Pathol. 2000. 24:1372–1377.

13. Kobari M, Egawa S, Shibuya K, Shimamura H, Sunamura M, Takeda K, et al. Intraductal papillary mucinous tumors of the pancreas comprise 2 clinical subtypes: differences in clinical characteristics and surgical management. Arch Surg. 1999. 134:1131–1136.

14. Obara T, Maguchi H, Saitoh Y, Itoh A, Arisato S, Ashida T, et al. Mucin-producing tumor of the pancreas: natural history and serial pancreatogram changes. Am J Gastroenterol. 1993. 88:564–569.
15. Sugiyama M, Atomi Y. Intraductal papillary mucinous tumors of the pancreas: imaging studies and treatment strategies. Ann Surg. 1998. 228:685–691.
16. Yamaguchi K, Ogawa Y, Chijiiwa K, Tanaka M. Mucin-hypersecreting tumors of the pancreas: assessing the grade of malignancy preoperatively. Am J Surg. 1996. 171:427–431.

17. Tanaka M. Intraductal papillary mucinous neoplasm of the pancreas: diagnosis and treatment. Pancreas. 2004. 28:282–288.

18. Sahani DV, Saokar A, Hahn PF, Brugge WR, Fernandez-Del Castillo C. Pancreatic cysts 3 cm or smaller: how aggressive should treatment be? Radiology. 2006. 238:912–919.

19. Lee CJ, Scheiman J, Anderson MA, Hines OJ, Reber HA, Farrell J, et al. Risk of malignancy in resected cystic tumors of the pancreas < or =3 cm in size: is it safe to observe asymptomatic patients? Amulti-institutional report. J Gastrointest Surg. 2008. 12:234–242.

20. Balcom JH 4th, Rattner DW, Warshaw AL, Chang Y, Fernandez-del Castillo C. Ten-year experience with 733 pancreatic resections: changing indications, older patients, and decreasing length of hospitalization. Arch Surg. 2001. 136:391–398.
21. Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002. 346:1128–1137.

22. Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003. 349:2117–2127.

23. Garcea G, Dennison AR, Pattenden CJ, Neal CP, Sutton CD, Berry DP. Survival following curative resection for pancreatic ductal adenocarcinoma. A systematic review of the literature. JOP. 2008. 9:99–132.
24. Spinelli KS, Fromwiller TE, Daniel RA, Kiely JM, Nakeeb A, Komorowski RA, et al. Cystic pancreatic neoplasms: observe or operate. Ann Surg. 2004. 239:651–657.
25. Talamini MA, Moesinger R, Yeo CJ, Poulose B, Hruban RH, Cameron JL, et al. Cystadenomas of the pancreas: is enucleation an adequate operation? Ann Surg. 1998. 227:896–903.
26. Madura JA, Yum MN, Lehman GA, Sherman S, Schmidt CM. Mucin secreting cystic lesions of the pancreas: treatment by enucleation. Am Surg. 2004. 70:106–112.
27. Tien YW, Hu RH, Hung JS, Wang HP, Lee PH. Noninvasive pancreatic cystic neoplasms can be safely and effectively treated by limited pancreatectomy. Ann Surg Oncol. 2008. 15:193–198.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download