Abstract
This is a case report on papillary thyroglossal duct cyst (TGDC) carcinoma along with synchronous occult papillary thyroid microcarcinoma. A 46-year-old woman visited our hospital because she had an anterior midline neck mass below her hyoid bone. Preoperative ultrasound-guided fine-needle aspiration cytology revealed signs of papillary TGDC carcinoma. We performed a Sistrunk operation and a total thyroidectomy. Histopathological examination of the specimen revealed papillary carcinoma arising in the TGDC and papillary microcarcinoma of the thyroid gland without extrathyroidal extension. Surgeons should be aware of TGDC carcinoma during surgical planning and postoperative treatment and should differentiate this carcinoma from an anterior midline neck mass.
Thyroglossal duct cyst (TGDC) carcinoma is a rare tumor, and just over 200 cases have so far been reported.1 TGDC carcinoma may be clinically indistinguishable from benign TGDC, and the diagnosis in most cases is incidental after surgical resection. The use of fine needle aspiration cytology under ultrasound guidance may enhance the preoperative diagnosis. In case of malignancy, clinicians should consider a Sistrunk operation and a thyroidectomy.
This is a report on a case of papillary TGDC carcinoma together with synchronous occult papillary thyroid microcarcinoma.
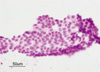
A 46-year-old female visited our clinic because of anterior midline neck mass. The mass was a 2×2 cm soft, non-tender mass in the midline below the hyoid bone. The thyroid gland was felt normal by palpation and no cervical lymph nodes were found. A neck ultrasound showed a 2.2×1.7 cm irregular heterogeneous echoic mass below the hyoid bone and no mass in the thyroid gland. Ultrasound-guided fine-needle aspiration cytology was performed and the results revealed a papillary carcinoma (Fig. 1). A neck computed tomography (CT) showed a 2.0×1.2 cm heterogeneously enhancing mass in the midline of the anterior neck and no abnormality in the thyroid or cervical lymph nodes (Fig. 2).
Thyroid function test revealed normal triiodothyronine, thyroxine, and thyroid stimulating hormone (TSH) levels but increased thyroglobulin levels of 59.52 ng/mL (0-25 ng/mL). Other laboratory investigations revealed no abnormalities. The patient underwent Sistrunk operation under general anesthesia. The frozen section revealed papillary carcinoma arising in a TGDC, therefore, a total thyroidectomy was performed.
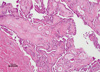
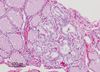
Histopathological examination disclosed papillary carcinoma that was confined to the cyst (Fig. 3). The non-neoplastic cystic spaces were partially lined by flattened epithelial cells. Pathologic analysis showed a 1 mm papillary carcinoma in the right lobe of the thyroid gland without extrathyroidal extension (Fig. 4). These findings suggested that the mass was a papillary carcinoma arising in a TGDC and occult microcarcinoma in the thyroid gland. After an operation, she was discharged without significant complications. Three months after the operation, blood level of thyroglobulin after TSH stimulation was normal (< 1 ng/mL) and anti-thyroglobulin antibody was 31 U/mL (0-55 U/mL). Six months after the operation, ultrasound of the neck displayed no recurrence in the thyroid gland or cervical lymph nodes.
Thyroglossal duct is the epithelial connection between the thyroid gland and the foramen cecum. The duct is normally obliterated during the 8th to 10th week of gestation. If the duct fails to involute completely, the remaining epithelium can lead to the development of a TGDC. Ellis and van Nostrand2 suggested that this failure to involute occurs in approximately 7% of the population.
The malignant transformation of the TGDC is uncommon. The incidence of TGDC carcinoma varies from 0.7 to 1% of all cases of TGDC.1,3 According to Widström, et al.,4 criteria for the diagnosis of primary carcinoma of the thyroglossal duct include the following: histological identification of a TGDC by demonstrating that the duct or cyst has an epithelial lining on which there are normal thyroid follicles within the wall of the cysts, normal thyroid tissue adjacent to the tumor, and histopathological examination of the thyroid gland showing no sign of primary carcinoma.5 The histologic findings of thyroglossal duct carcinoma are most commonly papillary carcinoma (75-80%), but other thyroid tumors such as follicular, Hürthle cell, and mixed papillary-follicular carcinomas have been reported.6
The most common clinical presentation is the presence of an anterior neck mass indistinguishable from that of a benign TGDC. However, neoplasia must be suspected in cases of TGDC in light of the recent changes in the clinical features. Imaging diagnostic techniques (ultrasound, scintigraphy and CT) are usually unable to preoperatively diagnose a malignant disease5 and fine needle aspiration yields a correct result in only 66% of the cases.7 There is a great deal of controversy around the surgical treatment of TGDC carcinoma. Although some surgeons consider the Sistrunk procedure alone to be sufficient for patients with no signs of disseminated diseases,8 recent reports recommend a total thyroidectomy in addition to the Sistrunk procedure.9 The number of reported incidences of primary thyroid carcinoma, concomitant with TGDC carcinoma is between 11 and 33%. The foci of such carcinomas are small (ranging from 0.2 cm to 1.5 cm), and are frequently not palpable or detectable by preoperative imaging techniques1,3,10 similar to our case. A total or subtotal thyroidectomy has been recommended if there is cystic wall invasion by the carcinoma, or if the TGDC carcinoma is greater than 1.0 cm, because larger lesions are more likely to behave aggressively.1 Removal of the thyroid gland allows for long-term monitoring of thyroglobulin levels and the use of I131 scintigraphy and I131 ablation therapy.
The prognosis for papillary TGDC carcinoma is excellent, with occurrence of metastatic lesions in less than 2% of cases.3 Follow-up procedures consist of physical examinations, ultrasound of the surgical region and thyroid, and a total body scintigraphy.
TGDC carcinoma is rare, occurring in approximately 1% of all TGDC cases. And the presence of papillary carcinoma in a TGDC with synchronous occult papillary thyroid microcarcinoma is a unique feature.
However, surgeons should be aware of thyroglossal duct carcinoma in surgical planning and postoperative treatment and should differentiate this tumor from an anterior midline neck mass.
Figures and Tables
Fig. 1
Sheet of follicular cells showing enlarged nuclei and intranuclear cytoplasmic inclusions (Papanicolaou,×400).
References
1. Heshmati HM, Fatourechi V, van Heerden JA, Hay ID, Goellner JR. Thyroglossal duct carcinoma: report of 12 cases. Mayo Clin Proc. 1997. 72:315–319.

2. Ellis PD, van Nostrand AW. The applied anatomy of thyroglossal tract remnants. Laryngoscope. 1977. 87:765–770.

3. Fernandez JF, Ordoñez NG, Schultz PN, Samaan NA, Hickey RC. Thyroglossal duct carcinoma. Surgery. 1991. 110:928–934.
4. Widström A, Magnusson P, Hallberg O, Hellqvist H, Riiber H. Adenocarcinoma originating in the thyroglossal duct. Ann Otol Rhinol Laryngol. 1976. 85:286–290.

5. Martín-Pérez E, Larrañaga E, Marrón C, Monje F. Primary papillary carcinoma arising in a thyroglossal duct cyst. Eur J Surg. 1997. 163:143–145.
6. Van Vuuren PA, Balm AJ, Gregor RT, Hilgers FJ, Loftus BM, Delprat CC, et al. Carcinoma arising in thyroglossal remnants. Clin Otolaryngol Allied Sci. 1994. 19:509–515.

7. Bardales RH, Suhrland MJ, Korourian S, Schaefer RF, Hanna EY, Stanley MW. Cytologic findings in thyroglossal duct carcinoma. Am J Clin Pathol. 1996. 106:615–619.

9. Kennedy TL, Whitaker M, Wadih G. Thyroglossal duct carcinoma: a rational approach to management. Laryngoscope. 1998. 108:1154–1158.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download