Abstract
Purpose
In Korea, there was no specific guidelines for the management of benign prostatic hyperplasia (BPH). We reviewed the practice patterns of Korean urologists in the management of BPH and aimed to describe the need to develop specific guidelines.
Materials and Methods
A probability sample was taken from the Korean Urological Association Registry of Physicians, and a structured questionnaire, that explored practice patterns in the management of BPH, was mailed to a random sample of 251 Korean urologists.
Results
For the initial evaluation of BPH, most urologists routinely performed prostatic specific antigen (PSA) (96.4%), digital rectal exam (94.4%), international prostate symptom score (IPSS) (83.2%) and transrectal ultrasound (79.2%). Symptom assessment (36.4%) followed by transrectal ultrasound of prostate (TRUS) (20.0%) was considered as the most important diagnostic examination affecting the decision about individual treatment options. Almost all urologists (92.2%) chose medical treatment as the first-line treatment option for uncomplicated BPH with moderate symptoms. Of the respondents, 57.2% had prescribed alpha blocker and 41.6% alpha blocker plus 5-alpha reductase inhibitors as the medical treatment option for BPH. The prescription of 5-ARIs was dependent on the size of the prostate and the severity of symptoms.
Conclusion
The results of our current survey provide useful insight into variations in the clinical practice of Korean urologists. They also indicate the need to develop further practical guidelines based on solid clinical data and to ensure that these guidelines are widely promoted and accepted by the urological community.
During the past two decades, the diagnosis and management of patients with benign prostatic hyperplasia (BPH) has dramatically changed. A range of options including pharmacological therapies, device therapies and new surgical procedures have emerged, and many of these new technologies have become available for the treatment of BPH.1,2 However, these new therapeutic modalities have been accompanied by controversy about the optimal strategies for treatment of BPH, and they leave a great deal of room for the personal opinions of individual physicians in the choice of treatment for patients with BPH. Despite several clinical practice guidelines suggesting optimal frameworks for the diagnosis and management of patients with BPH,3-9 there is a paucity of literature providing evidence from randomized clinical trials as a basis for preferred management strategies. Therefore, there are still arguments about applying these guidelines to the practical treatment of individual patients.5 In Asian populations, there is an another hurdle in applying these guidelines directly to the practical treatment of patients with BPH: in Asian men, the clinical characteristics related to BPH are different from those of BPH patients in Western populations. For example, Asian men have a similar incidence of lower urinary tract symptoms (LUTS) compared with men in the Western hemisphere, despite having a smaller average prostate volume and lower serum prostatic specific antigen (PSA) level.10,11 The current practical patterns in the management of patients with BPH may provide useful insights for setting up specific guidelines that include consideration of the clinical characteristics of the Asian population. To define the current spectrum of practice of Korean urologists for management of BPH, we performed a nationwide survey of the current strategies used by Korean urologists for diagnosis and management of patients with BPH.
We obtained a probability sample (n = 448) of Korean urologists from the Korean Urological Association (KUA) Registry of Physicians and selected 320 participants who were informed of the purpose of the survey and agreed to be enrolled before the survey began. Eligibility criteria required that participants should be urologists not in residency training and in active practice at least 20 hours per week.
The survey was conducted from May 2007. It was based on a structured questionnaire delivered via mail. Participants received the survey instrument, which consisted of a cover letter that identified the author and described the purpose of the survey and the survey questionnaire itself. The questionnaire was developed by the authors of this paper. The survey instrument was also reviewed and revised by additional experts and pretested for clarity and convenience for answering. The survey questionnaire was divided into two parts. The physician's preference in nonmedical therapy for BPH and a subjective estimation of the changes in treatment pattern related to patients with BPH were collected through Part 1 of the questionnaire (6 separate items). Part 2 of the questionnaire comprised 15 separate items related to the diagnosis and management of patients with BPH. It consisted of the practical view and patterns of diagnostic procedures, strategy for medication, and the individual physician's preference for medical therapy.
Student's t-test was done to determine the differences of practice patterns between the urologists in private clinics and general hospitals.
A total of 251 completed questionnaires were returned by urologists. The consent rate in the survey was 71.4% (80.2% in private clinics, 59.7% in general hospitals, respectively), and the compliance rate for the 320 urologists who initially agreed to participate was 78.4%.
Fig. 1 shows the symptoms that are frequently complained of by patients with suspected BPH. Almost all patients complained of voiding difficulties such as nocturia (98.8%), weak stream (96.8%), post voiding residual urine sense (95.6%) and daytime frequency (51.2%) while the incidence of the terminal dribbling (0.4%) was extremely low. For initial diagnostic assessments, the most frequently used tests were serum PSA evaluation (96.4%) and DRE (94.4%), and 91.6% of total respondents believed that the use of PSA in the initial evaluation of BPH had increased in Korea during the past decade. Symptom assessment, uroflowmetry, DRE and residual urine volume were frequently used more in general hospital rather than in private clinic as the initial evaluation of BPH (Table 1).
Table 1 lists various examinations and tests that were routinely performed during the follow-up period for patients with BPH. More than half the respondents (51.2%) reported that they routinely performed repeated checks of the symptom score during the follow-up period. The preference for uroflowmetry (38%), serum PSA level (36%), DRE (35.2%) and post voiding residual urine measurement (30.8%) were similar. The preference for IPSS and uroflowmetry was higher for urologists in general hospitals, while urologists in private clinics performed DRE most frequently (48%) (p < 0.05).
As seen in Fig. 2, 92.2% of respondents replied that they chose medical treatment as the initial management option for patients with BPH. Among 137 urologists who had experience of BPH-related surgery, 81% of respondents reported that they performed transurethral resection of the prostate (TURP) in at least one case during the past 12 months, while 25.5%, 22.4% and 15.3% of respondents performed open prostatectomy, photoselective vaporization of the prostate (PVP) and transurethral needle ablation (TUNA), respectively (Fig. 2). There was a significant difference in the use of nonmedical treatment for BPH between urologists in general hospitals and private clinics. Most common nonmedical treatment option was TURP among urologists in general hospitals (98%) while 38.5% for urologists in private clinics (p < 0.05). However, laser ablation was more common nonmedical treatment option for urologists in private clinics than that in general hospitals (33.3% vs. 19.5%, respectively, p < 0.05).
Of the pharmacological options, almost all urologists reported that they prescribed alpha blocker in the management of patients with BPH, while 5-ARIs were used less frequently. Of the respondents, 57.2% had prescribed alpha blocker as the primary treatment, and 41.6% prescribed alpha blocker with 5-ARIs as the primary treatment. Only 0.4% of the respondents preferred 5-ARI monotherapy as the initial treatment option for pharmacotherapy (Fig. 3). There was no significant difference in the medical treatment regimen between urologists in general hospitals and in private clinics.
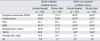
The judgment of severity of BPH is entirely individual urologists' estimation, but the proportion of combination therapy (alpha blocker with 5-ARIs) increased with the estimated severity of BPH. The proportion of alpha blocker monotherapy decreased from 77.8% in mild BPH to 21.9% in severe BPH, while the proportion of combination therapy increased in severe BPH (19.5% to 75.8%). Among the factors that were thought to be important when choosing the prescribed drugs were rapid relief of the symptoms (98.8%), the severity of BPH (85.2%), compliance of patients (80.0%) and adverse effects of the drug (78.8%) (Fig. 4). However, there was no significant difference in main concerns related to the decision of medical treatments between urologists in general hospitals and private clinics.
The evaluation and management of BPH has changed markedly, and these changes include the development of guidelines for investigation of BPH, the use of standard symptom scores and quality of life assessment, and the introduction of new medical therapies and technology. Despite the voluminous literature on BPH, many uncertainties still exist regarding the appropriate evaluation and management of individuals. Although several clinical practice guidelines have addressed the optimal treatment of men with BPH, there remain wide variations in patterns of practice. There are, in fact, several differences in the recommendations of the AUA guidelines and the EAU guidelines, which are widely accepted as the standard references for the management of patients with BPH.3,6 The differences in the recommendations of the guidelines may have originated not only from the difference in the patients' demographics and genetic factors but also from the medical insurance system, the accessibility of hospitals, manpower issues and cultural differences. There are no country-specific practice guidelines for Korea. Although the AUA and EAU guidelines are accepted in Korea as the two alternative choices for the management of patients with BPH, there is a paucity of literature concerning whether they really affect patient evaluation and management. Considering these points, the current report may provide some indication of the influence of the international guidelines on Korean urologists. DRE, assessment of symptoms score and PSA are the common recommendations of most of the international guidelines.5 In this survey, it was revealed that these examinations and evaluations are routinely performed by most of the urologists in Korea. We found that the preference for TRUS, uroflowmetry and post voiding residual urine measurement as the routine monitoring for BPH was significantly higher compared with the urologists' preference in other countries.12-14 TRUS is an optional test in both AUA and EAU guidelines, while uroflowmetry and postvoiding residual urine measurement are recommended only in the EAU guidelines.3,6 There might be multiple factors affecting the urologists' preference for these additional tests in evaluation of BPH. The authors believe that the public medical insurance system in Korea might be one of the most important factors. Korea is one of the advanced countries that have a well-established public medical insurance system, meaning that medical costs are very much cheaper than in other countries. For example, the medical fee for DRE in Korea is only three US dollars, and indeed the authors of this survey usually do not charge the DRE fee to patients. On the other hand, TRUS and uroflowmetry are relatively expensive, and the public insurance does not cover them. Although this is not the only possible explanation of the difference in the preferences of urologists in Korea, it is possible that these specific socioeconomic factors in Korea could affect the pattern of urologists' preferences in BPH evaluation practice. It was one of the important points of this survey that we could obtain information about the patterns of monitoring of patients with BPH by urologists. Despite numerous reports about the initial evaluation of BPH, there is little literature about the patterns of follow-up.
The surgical treatment of BPH has gradually decreased in Korea during recent decades. At the same time, the proportion of patients with BPH given medical treatment increased.10 We also found through this survey that most urologists believe that the incidence of TURP and other BPH-related surgery has given way to medical treatment as the optimal treatment for BPH.
The results of our current survey provide useful insights into variations in the clinical practice of Korean urologists. They also indicate the need to develop further practical guidelines, based on solid clinical data, and to ensure that these guidelines are widely promoted and accepted by the urological community. Further information on the preferences of patients themselves will help to advance the effectiveness of BPH treatment. Moreover, country-specific guidelines that take into consideration the characteristics of Korean men and the specific socioeconomic status of the individual country are needed for the advancement of evaluation and management of patients with BPH.
Figures and Tables
Fig. 1
Common symptoms that are frequently complained by patients with benign prostatic hyperplasia.
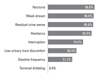
Fig. 2
The choice of non pharmacological therapy during the preceding 12 months (multiple choice). TURP, transurethral resection of the prostate; TUNA, transurethral needle ablation; TUDP, transurethral balloon dilation of the prostate.
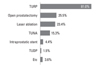
Fig. 3
The initial choices of pharmacological therapy for the newly diagnosed BPH patients. CAM, complimentary alternative medicine; BPH, benign prostatic hyperplasia.
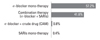
Fig. 4
Main concerns of the urologists that affect the initial treatment of the patients with BPH. BPH, benign prostatic hyperplasias; AUR, acute urinary retention.

ACKNOWLEDGEMENTS
We would like to thank all participating urologists of the Korean Urological Association for their cooperation in this survey.
References
1. Pomer S, Dobrowolski ZF. The therapy of benign prostatic hyperplasia using less-invasive procedures: the current situation. BJU Int. 2002. 89:773–775.

2. Sountoulides P, Tsakiris P. The evolution of KTP laser vaporization of the prostate. Yonsei Med J. 2008. 49:189–199.

3. AUA Practice Guidelines Committees. AUA guideline on management of benign prostatic hyperplasia (2003). Chapter 1: Diagnosis and treatment recommendations. J Urol. 2003. 170:530–547.
4. Irani J, Brown C, Van der Meulen J, Emberton M. [International comparison of guidelines for the management of benign prostatic hyperplasia: use of a validated generic tool]. Prog Urol. 2004. 14:29–32.
5. Irani J, Brown CT, Van der Meulen J, Emberton M. A review of guidelines on benign prostatic hyperplasia and lower urinary tract symptoms: are all guidelines the same? BJU Int. 2003. 92:937–942.

6. Madersbacher S, Alivizatos G, Nordling J, Sanz CR, Emberton M, de la Rosette JJ. EAU 2004 guidelines on assessment, therapy and follow-up of men with lower urinary tract symptoms suggestive of benign prostatic obstruction (BPH guidelines). Eur Urol. 2004. 46:547–554.

7. Nickel JC, Herschorn S, Corcos J, Donnelly B, Drover D, Elhilali M, et al. Canadian guidelines for the management of benign prostatic hyperplasia. Can J Urol. 2005. 12:2677–2683.
8. Oelke M, Michel MC, Höfner K. [German guidelines for the assessment of BPH. What's new in 2007?]. Urologe A. 2008. 47:149–154.
9. Spatafora S, Conti G, Perachino M, Casarico A, Mazzi G, Pappagallo GL. AURO. it BPH Guidelines Committee. Evidence-based guidelines for the management of lower urinary tract symptoms related to uncomplicated benign prostatic hyperplasia in Italy: updated summary. Curr Med Res Opin. 2007. 23:1715–1732.

10. Chung BH, Hong SJ, Cho JS, Seong DH. Relationship between serum prostate-specific antigen and prostate volume in Korean men with benign prostatic hyperplasia: a multicentre study. BJU Int. 2006. 97:742–746.

11. Lee E, Yoo KY, Kim Y, Shin Y, Lee C. Prevalence of lower urinary tract symptoms in Korean men in a community-based study. Eur Urol. 1998. 33:17–21.

12. Barry MJ, Fowler FJ Jr, Bin L, Oesterling JE. A nationwide survey of practicing urologists: current management of benign prostatic hyperplasia and clinically localized prostate cancer. J Urol. 1997. 158:488–491.
13. Ramsey EW, Elhilali M, Goldenberg SL, Nickel CJ, Norman R, Perreault JP, et al. Practice patterns of Canadian urologists in benign prostatic hyperplasia and prostate cancer. Canadian Prostate Health Council. J Urol. 2000. 163:499–502.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download