Abstract
Syphilis, along with the recent increase of human immunodeficiency virus (HIV) patients, has also been on the rise. It has a broad spectrum of clinical manifestations, among which cerebral gumma is, a kind of neurosyphilis, however, it is rare and can be cured by penicillin. Thus, cerebral gumma needs to be differentially diagnosed from other brain masses that may be present in syphilis patients. We have experienced a case where the patient was first suspected of brain tumor, but confirmed by surgery to be cerebral gumma due to neurosyphilis. This is the first such case encountered in Korea, therefore, we report it here in. A 40-year old woman complaining of headaches was found to have a brain mass on her CT scans and MRI. Suspecting a brain Tumor, a resection was performed on the patient, and histological results revealed that the central portion of the mass contained necrotic material and the peripheral region was infiltrated with plasma cells. Warthin-Starry staining of the region revealed spirochetes, and the patient was thus diagnosed as brain gumma. Venereal Disease Research Laboratory (VDRL) of cerebrospinal fluid (CSF) was reactive. After an operation, penicillin-G at a daily dose of 24×106 U was given for 10 days from post-operative day 10, and thereafter, the mass disappeared.
Syphilis is a systemic infectious disease caused by a spirochete, Treponema pallidum (T. pallidum), and can affect most organs. It is commonly transmitted via sexual contact, however, it is vertically transmitted from mother to fetus in some cases. Clinically, syphilis progresses through the following series of stages: incubation period after infection, primary syphilis, secondary syphilis, latent syphilis, and late syphilis (or tertiary syphilis). Late syphilis includes cardiovascular syphilis, neurosyphilis, and late benign syphilis (gummatous syphilis).1 Recent studies showed that syphilis is prevalent in human immunodeficiency virus (HIV)-positive patients, and that broad spectrum of symptoms are observed in patients with syphilis. Of the various types of neurosyphilis, gummatous neurosyphilis is very rare; its occurrence is not associated with HIV infection, and it is commonly misdiagnosed as brain tumor.2-4 Brain gumma is a completely curable disease, therefore, an appropriate diagnosis is essential for patient treatment and prognosis. Accordingly, gumma should be differentially diagnosed from a brain mass in patients with syphilis.
We encountered a patient with gumma accompanied by neurosyphilis. The patient was suspected of having a brain tumor and underwent surgery. Here, we report this case with a review of literature.
A 40-year-old woman visited the Department of Neurosurgery at our hospital with the chief complaint of a 3- to 4-month history of headache. She was referred to our hospital after computed tomography (CT) scans at an another hospital revealed that she had a brain tumor. Prior to her referral, she frequently suffered from headaches and used analgesics to control them. She had no past history of diabetes mellitus or hypertension, but had received treatment for pulmonary tuberculosis 20 years ago. She had also undergone a right salpingo-oophorectomy for ovarian cyst 22 years ago. She underwent hysterectomy for uterine myoma 4 months prior to the referral. It was not clear whether she had received a blood transfusion during the surgery. It was noted that she had engaged in prostitution in the past. Vital signs at admission were as follows: blood pressure, 126/88 mmHg; pulse rate, 75 beats/min; respiratory rate, 20 breaths/min; and body temperature, 36.4℃. She presented with acute sickness. On chest auscultation, the respiratory sounds were found to be normal and there were no crackles. She had a flat abdomen without pain or tenderness. She was mentally alert and did not have any cognitive or memory disturbance. She also did not show any evidence of language impairment. Both pupils showed normal light reflex. The result of the examination of deep tendon reflexes was normal, and there were no other neurological deficits. She had no numbness in the upper and lower extremities. Her muscle strength was normal, and she had no muscle atrophy.
The results of the following investigations were normal: complete blood count, serum electrolytes, liver function test, blood urine nitrogen, and serum creatinine. Her serum Venereal Disease Research Laboratory (VDRL) titer was 1 : 32, with a positive fluorescent treponemal antibody-absorption (FTA-ABS) (IgG). She was negative for hepatitis B surface antigen (HBsAg), antibody to HBsAg (HBsAb), and anti-HIV antibody (Ab). Urinalysis revealed no abnormal findings. The findings of chest radiography suggested inactive tuberculosis of the right superior chest. An electrocardiogram revealed no abnormal findings. Brain MRI scans revealed a mass measuring 1.6 cm with an ill-defined margin. It was accompanied with severe swelling in the region anterior to the temporal lobe of the left cerebrum (Fig. 1). A T1-weighted sagittal magnetic resonance (MR) image of the round mass-like lesion showed that the central portion was hypointense and the peripheral portion was isointense with the surrounding gray substance. A T2-weighted coronal image showed that the central portion of the lesion was hyperintense and the peripheral portion was isointense. A contrast-enhanced T1-weighted image demonstrated enhancement in the peripheral portion, but no enhancement in the central portion, indicating necrotic or cystic changes. Moreover, a diffusion-weighted image showed high signal intensity in the central portion of the lesion, strongly indicating that the lesion could be either a tumor or a brain abscess containing a fluid with high protein concentration. Furthermore, the proton MR spectroscopy performed in the same portion using an echo time of 135 m/s revealed inverted lactate double peaks at 1.3 ppm and peaks formed by choline compounds at 3.2 ppm. This indicated the possibility of a tumor accompanied with necrosis rather than brain abscess.
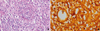
The patient was diagnosed with a brain tumor, and the mass was surgically resected. Temporal craniotomy was performed. The mass was found to be gray and soft, and was attached to the dura of the basal temporal lobe. Since the margin of the mass (size, 1.0×1.0×0.3 cm) was well defined, it was completely resected. Postoperatively, cerebrospinal fluid (CSF) cytology revealed an red blood cell (RBC) count of 0 cells/mm3, a white blood cell (WBC) count of 3 cells/mm3, and glucose and protein levels of 65 and 47.0 mg/dL. In addition, the results of VDRL and FTA-ABS IgG tests were positive. No microorganisms were isolated from the specimen obtained during surgery. Histopathological examination revealed that the central portion of the mass contained a necrotic material infiltrated with eosinophils, and the peripheral region that had become fibrotic contained lymphocytes and plasma cells. High-power view of the mass showed occlusions of small arterioles, and Warthin-Starry staining of this region revealed spirochete infection (Fig. 2).
The patient was finally diagnosed with brain gumma. Based on this diagnosis, water-soluble penicillin G was intravenously administered at a daily dose of 24×106 U for 10 days from postoperative day 10. Thereafter, the headache disappeared, and there were no other neurological deficits. The patient was, therefore, discharged. Two months postoperatively, no tumor mass was observed on follow-up MRI scans (Fig. 1). Six months postoperatively, CSF cytology demonstrated an RBC count of 0 cells/mm3, WBC count of 1 cell/mm3, and glucose and protein levels of 55 and 28.0 mg/dL. The results of the VDRL test changed from positive to negative, and the serum VDRL titer was 1 : 64.
Syphilis is a chronic, systemic infectious disease caused by the spirochete T. pallidum; and it was expected to be eradicated by the use of penicillin of the most effective antibiotics.5 Since 2000s, however, syphilis has been reported to be prevalent among HIV patients in several countries.6,7 Recently, such cases have also been observed in Korea.8 HIV infection and syphilis are mutual risk factors responsible for the increasing incidence of neurosyphilis in HIV patients.9 A broad spectrum of symptoms is manifested in HIV patients with syphilis. Recent studies showed an annual increase in the incidence of HIV infection, therefore, physicians should be attentive to the occurrence of neurosyphilis.
Neurosyphilis has a broad spectrum of clinical manifestations, and it can occur after 1 to 25 years following infection.10 Various manifestations of neurosyphilis are observed, such as asymptomatic, meningovascular, and parenchymal neurosyphilis. Therefore, it can pose a diagnostic challenge to physicians. Neurosyphilis should be treated with a long-term, intravenous infusion of antibiotics. Inadequate or inappropriate treatment can lead to the development of neurological deficits. The clinical suspicion and diagnosis of neurosyphilis are, therefore, mandatory.11
Review of the literature revealed that there are very rare cases of brain gumma due to neurosyphilis. Merrit et al.12 treated 676 neurosyphilis patients for 15 years prior to the development of penicillin. According to these authors, 1 case of brain gumma developed from a cohort of patients. The etiology of brain gumma due to neurosyphilis was presumed to be an excessive response of the cell-mediated immune system to T. pallidum. Histopathologically, this case was characterized by the presence of a circumscribed mass resembling granuloma at the site where lymphocytes or plasma cells infiltrated the brain parenchyma or meninges. This granuloma underwent fibrotic or necrotic transformation over time.13
Spirochetes are rarely identified from tissue samples. In the present case, the spirochetes were detected on histological examination. Under clinical suspicion of cerebral gumma, careful examination is necessary to detect spirochetes; polymerase chain reaction (PCR) for T. pallidum would be useful for definitive diagnosis in cases where diagnosis is difficult.14 Brain gumma commonly develops from the dura and pia mater over the cerebral convexity or at the base of the brain. Single or multiple masses attached to the dura mater can invade brain parenchyma.13 The symptoms of brain gumma are similar to those of other tumors arising from brain parenchyma and are often accompanied by a seizure. The radiological findings of brain gumma are very inconsistent. On CT scans, the lesion was localized at the periphery of brain tissue. The findings of non-contrast-enhanced CT reveal a hypodense area with no mass effect. On contrast-enhanced CT scans, however, brain gumma can be observed to be accompanied with severe edema of adjacent tissue.15 T1-weighted MRI scans show a low-intensity or isointensity mass. T2-weighted MRI scans, however, reveal a homogeneous and high-intensity mass. The adjacent area of the mass shows high intensity on T1-weighted images and a low intensity on T2-weighted images.15,16
Brain gumma occurs commonly in association with the meninges. Accordingly, the location of lesion and the findings of contrast-enhanced imaging are useful in making a presumptive diagnosis of brain gumma.17 In the present case, both brain tumor and brain abscess were highly suspected since the central portion of the lesion was found to be hypointense in the T1-weighted sagittal MR image but hyperintense in the T2- weighted coronal image, with heightened contrast enhancement in the peripheral portion. However, the diffusion-weighted image showed high signal intensity in the central portion of the lesion, strongly indicating a possibility of brain abscess.18 On the other hand, the MR spectroscopic image showed comparatively higher peaks formed by choline compounds, indicating the possibility of a tumor rather than brain abscess. The choline peaks in MR spectroscopic imaging represent the complexes of phosphorylcholine and glycerophosphorylcholine that are found in the membrane, and these complexes play a role in cell membrane synthesis or destruction; choline peaks are thus regarded as markers of cancer. In the present case, the results of diffusion-weighted imaging indicated the presence of abscess, whereas those of MR spectroscopic imaging indicated the presence of a tumor. Further radiological studies on cerebral gumma are required.
Physicians should be able to make a differential diagnosis of gumma of brain parenchyma from toxoplasmosis, lymphoma, and bacterial, mycobacterial, and fungal abscesses. This is particularly important in the case of HIV-positive patients. A serological test or response to empirical treatment can be useful for the differential diagnosis of toxoplasmosis. Although rarely occurs, brain abscesses caused by Nocardia asteroids or Listeria monocytogenes can be responsive to penicillin. A slow response to the treatment and the necessity of long-term use of antibiotics are important clues for differential diagnosis of these cases.
In our present case, the patient was preoperatively suspected of having a brain tumor but was diagnosed with brain gumma, based on brain histopathology and CSF cytology. Previous reports have also described cases of brain gumma being initially diagnosed as brain tumors, but later correctly diagnosed intraoperatively.3,4 There have also been some cases in which a diagnosis was made without histopathological evidence following a suspicion of brain gumma. Suarez et al. suspected the presence of brain gumma, based on the results of VDRL-positive CSF cytology and presence of a high-intensity mass on T2-weighted MRI scans.19 These authors administered a 21-day course of the intravenous infusion of a high-dose, water-soluble penicillin G. Six days after the treatment, they noted a loss of contrast enhancement in the lesion on a T2-weighted image. One month later, when abnormal radiological findings disappeared, they confirmed a diagnosis of brain gumma with no histopathological evidence.19 This suggests that surgery is not always necessary for the diagnosis and treatment of brain gumma. From an empirical perspective, a high-dose penicillin therapy accompanied with MRI findings of a decrease in mass size, would be useful for the diagnosis and treatment of brain gumma in cases where neurosyphilis could be diagnosed based on the CSF examination and MRI, thereby avoiding unnecessary surgeries.
To our best knowledge, this is the first reported case of brain gumma that was diagnosed and treated in Korea after confirming the presence of spirochetes in the brain tissue of a patient who was first suspected of having a brain tumor. Having recognized the recent prevalence of syphilis in HIV patients and the fact that brain gumma can be cured by antibiotics, we suggest that brain gumma should be considered for a differential diagnosis of a brain mass in syphilis patients.
Figures and Tables
Fig. 1
MR images of the patient(A-D). (A) T1-weighted sagittal image shows a round mass-like lesion with isointensity in the peripheral and hypointensity in the central portion of the left temporal lobe (arrow). (B) T2-weighted coronal images show the lesion with isointensity in the peripheral and hyperintensity in the central portion with severe vasogenic edema in the surrounding region. (C) Diffusion-weighted image of the central portion of the lesion shows high signal intensity, which suggests brain abscess or necrotic tumor. (D) Contrast-enhanced, T1-weighted image demonstrates peripheral enhancement of the lesion with no enhancement of the central portion. (E) MR spectroscopic image shows small inverted lactate peaks (doublet peak at 1.3 ppm, white arrow) and slightly higher choline peaks (open arrow). This suggests the presence of a tumor rather than an abscess.

Fig. 2
(A) High-power view of the mass shows small arterioles with lymphocytic and plasma cell infiltration in the adventitia and media, concentric collagenous thickening of the intima, and occlusion of the lumen (×400, H & E stain). (B) In the central area, one thinly coiled microorganism, Treponema pallidum, is observed (×1,000, Warthin-Starry stain).
References
3. Ances BM, Danish SF, Kolson DL, Judy KD, Liebeskind DS. Cerebral gumma mimicking glioblastoma multiforme. Neurocrit Care. 2005. 2:300–302.

4. Pall HS, Williams AC, Stockley RA. Intracranial gumma presenting as a cerebral tumour. J R Soc Med. 1988. 81:603–604.

6. Hopkins RS, Jajosky RA, Hall PA, Adams DA, Connor FJ, Sharp P, et al. Summary of notifiable diseases--United States, 2003. MMWR Morb Mortal Wkly Rep. 2005. 52:1–85.
7. Doherty L, Fenton KA, Jones J, Paine TC, Higgins SP, Williams D, et al. Syphilis: old problem, new strategy. BMJ. 2002. 325:153–156.

8. Jang HC, Cho JH, Park WB, Lee KD, Lee CS, Kim HB, et al. Outbreak of primary and secondary syphilis among HIV sero-positive patients in Korea. Infect Chemother. 2004. 36:366–372.
9. Johns DR, Tierney M, Felsenstein D. Alteration in the natural history of neurosyphilis by concurrent infection with the human immuno deficiency virus. N Engl J Med. 1987. 316:1569–1572.

10. Clark EG, Danbolt N. The Oslo study of the natural history of untreated syphilis; an epidemiologic investigation based on a restudy of the Boeck-Bruusgaard material; a review and appraisal. J Chronic Dis. 1955. 2:311–344.
12. Merritt HH, Adams RD, Solomon HC. Neurosyphilis. 1946. New York: Oxford University Press;62–66.
13. Berger JR, Waskin H, Pall L, Hensley G, Ihmedian I, Post MJ. Syphilitic cerebral gumma with HIV infection. Neurology. 1992. 42:1282–1287.

14. Horowitz HW, Valsamis MP, Wicher V, Abbruscato F, Larsen SA, Wormser GP, et al. Brief report: cerebral syphilitic gumma confirmed by the polymerase chain reaction in a man with human immunodeficiency virus infection. N Engl J Med. 1994. 331:1488–1491.

15. Agrons GA, Han SS, Husson MA, Simeone F. MR imaging of cerebral gumma. AJNR Am J Neuroradiol. 1991. 12:80–81.
16. Vogl T, Dresel S, Lochmüller H, Bergman C, Reimers C, Lissner J. Third cranial nerve palsy caused by gummatous neurosyphilis: MR findings. AJNR Am J Neuroradiol. 1993. 14:1329–1331.
17. Brightbill TC, Ihmeidan IH, Post MJ, Berger JR, Katz DA. Neurosyphilis in HIV-positive and HIV-negative patients: neuroimaging findings. AJNR Am J Neuroradiol. 1995. 16:703–711.
18. Cartes-Zumelzu FW, Stavrou I, Castillo M, Eisenhuber E, Knosp E, Thurnher MM. Diffusion-weighted imaging in the assessment of brain abscesses therapy. AJNR Am J Neuroradiol. 2004. 25:1310–1317.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download