Abstract
Purpose
To identify the incidence of new vertebral compression fractures in women after kyphoplasty and to analyze influential factors in these patients.
Materials and Methods
One hundred and eleven consecutive female patients with osteoporotic vertebral compression fractures (VCFs) underwent kyphoplasty at 137 levels. These patients were followed for 15.2 months postoperatively. For the survey of new vertebral compression fractures, medical records and x-rays were reviewed, and telephone interviews were conducted with all patients.
Results
During that time 20 (18%) patients developed new VCFs. The rate of occurrence of new VCFs in one year was 15.5% using a Kaplan-Meier curve. Body mass index (BMI), symptom duration and kyphoplasty level were the statistically significant factors between the patient groups both with and without new VCFs after kyphoplasty. In the comparison between the adjacent and remote new VCF groups, the adjacent new VCF group showed a larger amount of polymethyl methacrylate (PMMA) use during kyphoplasty (p < 0.05). Before kyphoplasty, 9.9% of the patients had been prescribed medication for osteoporosis, and 93.7% of the patients started or continued medication after kyphoplasty. The development of new VCFs was affected by the number of vertebrae involved in the kyphoplasty. However, the lower incidence rate (15.5%) of new compression fractures might be due to a greater percentage (93.7% in our study) of patients taking anti-osteoporotic medication before and/or after kyphoplasty.
Conclusion
When kyphoplasty is planned for the management of patients with osteoporotic VCFs, the application of a small amount of PMMA can be considered in order to lower the risk of new fractures in adjacent vertebrae. The postoperative use of anti- osteoporotic medication is recommended for the prevention of new VCFs.
Osteoporotic vertebral compression fracture (VCF) is a significant cause of morbidity and mortality among elderly patients.1,2 Traditionally, osteoporotic VCF has been treated with bed rest, analgesics, braces, and physical therapy. However, bed rest is a known predisposing factor for further bone loss, resulting in an increased tendency for additional osteoporotic fractures.3 Multiple co-morbidities such as depression, poor nutritional status, decreased appetite, and decreased pulmonary function have been reported in patients with osteoporotic fractures, and some have even reported that conservative treatments can cause significant morbidity and mortality in these patients.4-7 Kyphoplasty is now a therapeutic option for patients in whom medical management has not been successful or who are at risk of complications secondary to immobilization. The procedure is minimally invasive and can improve vertebral height and stabilize osteoporotic VCFs.7-12
One of the main concerns in kyphoplasty is that new fractures can develop at non-treated levels following augmentation with bone cement. It remains unclear whether new vertebral body fractures are simply the result of the natural progression of osteoporosis or if they should be regarded as a consequence of augmentation with bone cement.13-16
Therefore, the purpose of this study was to quantify new VCFs in patients who had undergone kyphoplasty and to analyze any influential factors that could affect them.
A total of 111 female patients (137 vertebrae) who had undergone kyphoplasty for osteoporotic compression fractures between March 2002 and June 2005 were reviewed retrospectively. Since osteoporosis is known to occur predominantly in women, only female patients were selected for this study. Of the patients who required multiple interventions, those with compression fractures secondary to osteoporosis were selected for our retrospective analysis. We excluded patients who had undergone kyphoplasty due to metastatic diseases or multiple myeloma. The minimum follow-up period after kyphoplasty was six months. In order to investigate any influencing factors that could have affected new vertebral body fracture, we reviewed the factors of age, sex, body mass index (BMI), primary diagnosis, bone mineral density of the lumbar spine (especially on the bodies of L1, L2, L3, and L4; Hologic, MA, USA), the time interval between the date of the onset of pain and the date of kyphoplasty (symptom duration), old and recent vertebral compression levels, the amount of polymethyl methacrylate (PMMA) injected per vertebral body, the level of new vertebral body fractures, pre- or post-operative medications for osteoporosis, and time from the initial kyphoplasty to the development of new fractures.
All patients had magnetic resonance imaging (MRI) prior to kyphoplasty. The MRI criteria that suggested acute compression fractures included low signal intensity of the bone marrow within the vertebral body on T1-weighted images and high signal intensity on gadolinium-enhanced images.17
Kyphoplasty had been performed only in patients who had intractable pain despite non-operative treatment over a duration of two weeks. The only exceptions were those over the age of 85 years or those in whom non-operative care might exacerbate the underlying disease due to the long period of bed rest.
The surgical technique for kyphoplasty is described elsewhere.9,10 After the operation, patients were encouraged to resume all of their normal daily activities without restrictions. Patients with fractures in the lumbar spine were instructed to wear a lumbar corset when out of bed. Most patients were prescribed medication for osteoporosis.
New fractures after kyphoplasty can occur, and these were diagnosed when the following criteria were met:
1)An acute increase in pain after kyphoplasty with identifiable back pain at the corresponding anatomical level.
2)Radiologically, marrow replacement with edema on MRI or an increased uptake on Tc-99m methylene diphosphate whole-body bone scan.
1)No acute back pain after kyphoplasty.
2)Evidence of a loss of vertebral body height on a lateral radiograph when compared with a previous lateral radiograph taken before initial kyphoplasty.
3)Vertebral body deformity ratio less than the cut-off value for osteoporotic vertebral fracture in the morphometric data criteria for Korean women.18
Additionally, telephone interviews were performed with 106 out of the 111 patients to search for patients with new VCFs that may have been initially missed. Each patient was questioned on current back pain and any hospital visits due to back pain after kyphoplasty. Those who answered affirmatively to either of the two questions were asked to revisit the institution. Among them, 20 patients returned with the complaint of postoperative back pain before or during the telephone interview and took a follow-up roentgenogram. The remaining five patients could not participate in the telephone interview because they had already expired. However, they all had been followed-up for over six months after kyphoplasty and did not complain of increased back pain.
The student t-test was used to compare the patient group experiencing new VCF after kyphoplasty with the patient group not experiencing new VCF after kyphoplasty. A Pearson's correlation analysis was used for the evaluation of relationships among the total compression fracture level before kyphoplasty, age, BMI, and lumbar spine bone mineral density. A Wilcoxon rank sum test was applied for the comparison between adjacent and remote new VCF groups. Additionally, a Kaplan-Meier survival curve was constructed to predict the ratio of new compression fractures. The SAS 8.1 program (SAS Institute, Cary, NC, USA) was used for the statistical analysis (significance level = 0.05).
One hundred and eleven female patients underwent kyphoplasty during the study period. These patients had a total of 137 spinal levels managed with kyphoplasty due to osteoporotic VCF. The mean age of female patients was 74.9 years (range, 56-92 years). The mean symptom duration was 30.3 days (range, 1-240 days). Aside from two cases of steroid-induced osteoporosis, all patients had primary osteoporosis. Bone mineral density analysis of the lumbar spine was performed in 70 patients (63%). The mean T-score in preoperative lumbar spine bone mineral density was -2.93 (0.660mg/cm2). Eleven patients (9.9%) had been prescribed medication for osteoporosis before kyphoplasty, and 104 patients (93.7%) started or continued medication after kyphoplasty. Most of the patients were prescribed bisphosphonate. Raloxifen and calcitonin were also prescribed in 12% of the patients (10% received raloxifen and 2% were taking calcitonin). The average follow-up period was 15.2 months (range, 6-39 months), and an old compression fracture was noted in 165 vertebral bodies (52 cases). The average amount of PMMA injected per vertebral body was 4.3cc (range, 0.5-9cc). The number of vertebral bodies managed with kyphoplasty was one in 89 cases (80.2%), two in 18 cases (16.2%), and three in 4 cases (3.6%).
L1 was the most common site of initially-treated fracture. Initial compression fractures and new compression fractures commonly developed at the thoraco-lumbar junction (Table 1).
Out of the 111 total female patients (137 vertebrae) treated with kyphoplasty for osteoporotic compression fracture, 20 patients (18%) and 23 vertebrae (16.8%) developed new compression fractures. Among them, 14 patients (12.6%) suffered from painful new compression fractures and the other 6 patients (5.4%) had subclinical new compression fractures without pain (Table 2). Six patients with painful compression fractures underwent a second kyphoplasty while the remaining eight patients declined the procedure (Table 2). The incidence of new compression fracture per procedure was 16.8% (23 out of 137 vertebrae).
Out of 23 vertebrae with newly-developed fractures after kyphoplasty, 8 were superiorly adjacent and 5 were inferiorly adjacent to the initial compressed vertebra that underwent kyphoplasty. The rest were remotely located from the initial vertebra with the compression fracture. The onset of pain for patients with a new fracture varied ranging from 1 to 32 months after the initial kyphoplasty (Table 2).
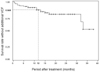
A Kaplan-Meier Survival Curve shows the disease-free survival rate over time without new fractures for patients with compression fractures (Fig. 1). The figure shows a sudden decline in the disease-free survival rate 30 months after a new compression fracture, which could be due to the two patients who had re-fractures 30 months after the new compression fracture and also because most of the patients were lost during the follow-up period of over 30 months. However, the disease-free survival rate was significantly high with a gentle decrease during the first 30 months and with an estimated mean one-year survival rate of 84.5%.
In comparison between the group with additional compression fractures and the other group without additional fractures, BMI, symptom duration and the level of kyphoplasty were the statistically significant factors (p < 0.05) (Table 3). The amount of PMMA was the statistically significant factor between the superior and inferior adjacent new compression fracture group and the remote new compression fracture group. According to the comparison of the adjacent new compression fracture and the remote new compression fracture groups, the adjacent new compression fracture group showed a larger amount of PMMA (Table 4).
There was no complication attributed directly to the procedure except for one case of pedicular cement leakage. The patient underwent decompression with removal of the leaked cement due to skin irritation.
There have been many reports regarding the effect of kyphoplasty in osteoporotic compression fracture.4,8-12 It has been controversial whether new compression fractures are simply the result of the natural progression of osteoporosis or if they should be regarded as the consequence of stiffness by augmentation with bone cement.13-16,19-21
Villarraga et al.21 reported on a biomechanical study using a multilevel spinal unit model that could be adjusted for stress and strain. It was found that the stress and strain of spinal levels adjacent to a kyphoplasty-treated level were minimal, and that the stress and strain levels found in the treated levels were less than the injury tolerance limits of cancellous and cortical bone. Ananthakrishnan et al.19 reported that kyphoplasty allowed the disc to generate higher nuclear pressures but that the pressure did not increase above the level of the intact state. Kayanja et al.22 also reported that cement augmentation of a fractured vertebral segment reduced stiffness while increasing both superior and inferior adjacent cortical strain.
These mechanical studies suggest that new compression fractures after kyphoplastic intervention are likely the result of the progression of osteoporosis and not due to the intervention itself.
We initially designed this study to find the incidence of new vertebral compression fracture after kyphoplasty in women and to decipher the factors influencing the incidence rate.
Several studies have reported relatively low rates of new vertebral compression fractures ranging from 12% to 15.1%,7,11,23 except a study reporting their rate as high as 26%.14 In our study, about one third of the patients with new compression fractures were clinically asymptomatic (Table 2), presuming that the estimated rate of new compression fractures would probably be greater than that of those who are symptomatic and who revisit the hospital due to postoperative pain. Our research showed an 18% occurrence of new compression fractures in women with no follow-up loss.
Lindsay et al.16 reported a 19.2% prevalence of new compression fractures during a one-year follow-up period in postmenopausal females with newly-developed vertebral compression fractures. Our research yielded a comparable result with 15.5% of new compression fractures in postoperative patients after one year of follow-up (Fig. 1). In addition, the survival curve showed a relatively gentle decrease over time after compression fracture, meaning that the incidence of additional compression fracture was not concentrated at a certain period of time, especially during the early period after kyphoplasty, in contrast to the result of Fribourg et al.14
Our research showed that BMI was a significant factor in the comparison between the patient group with additional compression fractures and the other group without (Table 3). Ravn et al.24 reported that a low BMI was an important risk factor for increased bone loss in postmenopausal women. In addition to the BMI, symptom duration and the number of kyphoplasty procedures were statistically significant in a comparison of the two groups. It seems plausible that a greater number of kyphoplasty procedures were performed in the group with additional compression fractures, and this could have affected the development of additional compression fractures to some extent. However, the rate (15.5%) of one-year additional compression fractures by our data was not as high as the rate (19.2%) due to natural progression reported by Lindsay et al.,16 meaning that there might be some other factors that were involved in lowering the incidence rate in our study. The low incidence rate might be attributed to the fact that most of the patients, except the two patients with steroid-induced osteoporosis, were primarily osteoporotic, and a great portion (as high as 93.7%) of the patients started or continued to take anti-osteoporotic medication after kyphoplasty. Other factors such as racial differences in bone quality should also be considered as possible influences.
The amount of bone cement was irrelevant to the development of new VCFs.
However, in the comparison of the adjacent new compression fracture and the remote new compression fracture groups, the adjacent new compression fracture group showed a larger amount of PMMA had been used during kyphoplasty (Table 4). When adjacent compression fractures occur, especially in the wedge type of fracture, the spine can be disabled due to the abrupt increase in kyphosis during which morphologic deformity develops: this is less likely with remote VCFs. Therefore, during kyphoplasty, if decrement of new VCF in adjacent vertebra through use of small amount of bone cement can be considered significant.
In this study, analysis was based on female osteoporosis patients alone without a control group (conservatively managed group). Therefore, our analysis was limited.
In conclusion, the development of new compression fractures after kyphoplasty was affected by the number of vertebrae involved in the procedure. However, our study yielded a relatively lower one-year incidence rate (15.5%) of new compression fractures than the rate (19.2%) due to natural osteoporosis progression. The lower incidence rate might be due to a greater percentage (93.7% in our study) of patients taking anti-osteoporotic medication before and/or after kyphoplasty. Thus, when facing kyphoplasty for patients with osteoporotic compression fractures, spine surgeons should consider postoperative use of anti-osteoporotic medication for the prevention of additional compression fractures. In addition, the use of the least amount of bone cement is irrelevant to the frequency of new fractures in remote vertebrae but may be considered for decreasing the risk of new fractures in adjacent vertebrae.
Figures and Tables
Fig. 1
A Kaplan-Meier Product-Limit Survival Curve depicting the disease-free survival rate without additional fracture for patients with compression fractures over time. The mean one-year survival rate is 84.5%.
References
1. Cook DJ, Guyatt GH, Adachi JD, Clifton J, Griffith LE, Epstein RS, et al. Quality of life issues in women with vertebral fractures due to osteoporosis. Arthritis Rheum. 1993. 36:750–756.

2. Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999. 159:1215–1220.
3. Takata S, Yasui N. Disuse osteoporosis. J Med Invest. 2001. 48:147–156.
4. Feltes C, Fountas KN, Machinis T, Nikolakakos LG, Dimopoulos V, Davydov R, et al. Immediate and early postoperative pain relief after kyphoplasty without significant restoration of vertebral body height in acute osteoporotic vertebral fractures. Neurosurg Focus. 2005. 18:e5.

5. Gold DT. The clinical impact of vertebral fractures: quality of life in women with osteoporosis. Bone. 1996. 18(3 Suppl):185S–189S.

6. Leech JA, Dulberg C, Kellie S, Pattee L, Gay J. Relationship of lung function to severity of osteoporosis In women. Am Rev Respir Dis. 1990. 141:68–71.

7. Rhyne A, Banit D, Laxer E, Odum S, Nussman D. Kyphoplasty: report of eighty-two thoracolumbar osteoporotic vertebral fractures. J Orthop Trauma. 2004. 18:294–299.

8. Crandall D, Slaughter D, Hankins PJ, Moore C, Jerman J. Acute versus chronic vertebral compression fractures treated with kyphoplasty: early results. Spine J. 2004. 4:418–424.

9. Garfin SR, Yuan HA, Reiley MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. 2001. 26:1511–1515.
10. Lieberman IH, Dudeney S, Reinhardt MK, Bell G. Initial outcome and efficacy of "kyphoplasty" in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001. 26:1631–1638.

11. Majd ME, Farley S, Holt RT. Preliminary outcomes and efficacy of the first 360 consecutive kyphoplasties for the treatment of painful osteoporotic vertebral compression fractures. Spine J. 2005. 5:244–255.

12. Phillips FM, Ho E, Campbell-Hupp M, McNally T, Todd Wetzel F, Gupta P. Early radiographic and clinical results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Spine. 2003. 28:2260–2267.

13. Donovan MA, Khandji AG, Siris E. Multiple adjacent vertebral fractures after kyphoplasty in a patient with steroid-induced osteoporosis. J Bone Miner Res. 2004. 19:712–713.

14. Fribourg D, Tang C, Sra P, Delamarter R, Bae H. Incidence of subsequent vertebral fracture after kyphoplasty. Spine. 2004. 29:2270–2277.

15. Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000. 15:721–739.

16. Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB, et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001. 285:320–323.

17. Do HM. Magnetic resonance imaging in the evaluation of patients for percutaneous vertebroplasty. Top Magn Reson Imaging. 2000. 11:235–244.

18. Jahng JS, Moon SH. Correlation of the bone mineral density with morphometric dimensions and characteristics of osteoporotic vertebral fracture. J Korean Orthop Assoc. 1998. 33:375–384.

19. Ananthakrishnan D, Berven S, Deviren V, Cheng K, Lotz JC, Xu Z, et al. The effect on anterior column loading due to different vertebral augmentation techniques. Clin Biomech (Bristol, Avon). 2005. 20:25–31.

20. Belkoff SM, Mathis JM, Fenton DC, Scribner RM, Reiley ME, Talmadge K. An ex vivo biomechanical evaluation of an inflatable bone tamp used in the treatment of compression fracture. Spine. 2001. 26:151–156.

21. Villarraga ML, Bellezza AJ, Harrigan TP, Cripton PA, Kurtz SM, Edidin AA. The biomechanical effects of kyphoplasty on treated and adjacent nontreated vertebral bodies. J Spinal Disord Tech. 2005. 18:84–91.

22. Kayanja MM, Togawa D, Lieberman IH. Biomechanical changes after the augmentation of experimental osteoporotic vertebral compression fractures in the cadaveric thoracic spine. Spine J. 2005. 5:55–63.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download