INTRODUCTION
The growing overweight and obese population has become a major health issue in United States, and obesity has reached epidemic proportions.
1,
2 In Korea, the 3rd National Health and Nutrition Survey
3 in 2005 reported that overall prevalence of obesity among adults, which is defined as having a body mass index (BMI) ≥ 25.0 kg/m
2, was 31.7% (35.2% in men and 28.3% in women), and that it had increased (overall 29.6%, 31.2% in men and 27.9% in women) when compared to the survey from 2001. Overweight individuals have increased risk of developing hypertension, type 2 diabetes, hypercholesterolemia, cancers, and dying prematurely, which calls for urgent intervention to curve the continuous increase of obese population.
4 In practice, 5 to 10% weight loss in obese patients improves their cardiovascular risk profiles
5-
7 and can reduce the future incidence of type 2 diabetes.
8-
10
Traditional Korean meals consist of steamed rice, soup, and a variety of side dishes including vegetables, mushrooms, seaweeds, legumes, soybean curd, fish, seafood, and chicken. However, modern Asians, including Koreans, are increasing their consumption of fast food, refined rice products, trans-fats, meats containing saturated fat, and other unhealthy foods.
11 Modern Koreans are also less physically active than their ancestors. Changes in their staple diet and reduced physical activity
12 may be contributing to the trend of increasing obesity prevalence. Therefore, consumption of steamed rice, Korea's staple food, should be reduced and foods lower in saturated fat and high in protein should be included in the traditional diet. For this reason, we have developed the Protein-Rich Oriental Diet (PRO Diet), a modified protein-enriched diet program that encourages the consumption of low-saturated fat, high-protein oriental foods cooked with legumes, soybean curd, soy milk, mushrooms, nuts, seafood, fish, chicken breast, lean meat, and vegetables, while refraining from foods that are high in simple sugars, refined starches and saturated fats, without calorie calculation. Furthermore, there are no previous studies using PRO Diet application in the field of community-based obesity control programs. In this aspect, we applied the PRO Diet to a preliminary 12-week community-based obesity control program at two different centers located in Gyeonggi Province. The aim of this study, therefore, was to evaluate the efficacy, safety and availability of the community-based obesity control PRO Diet program.
MATERIALS AND METHODS
Study design
Two public health centers in Dongducheon and Ansan were financially sponsored by the Gyeonggi Province Office for the 12-week community-based obesity control program (Slim Gyeonggi Project) from May to December of 2007. We applied the structured PRO Diet to all the participants for 12 weeks and evaluated its efficacy based on anthropometric changes, cardiovascular risk factors, safety and availability in a community-based obesity control program compared to the conventional diet program carried out in the public health center of Ansan in 2006. We recruited participants via local television, advertisement, newspapers. All the participants entering this 12-week PRO Diet program gave informed consent for their results and data to be used for research and publication. Participants regularly visited the public health center of their choice at intervals of one or two weeks for a total of 12 weeks. Participants were instructed by registered nurses, nutritionists, and exercise trainers on behavior modification, nutrition, and exercise throughout the 12-week program at one of the public health centers. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research. The Institutional Review Board of Ajou University Hospital in Suwon, South Korea, approved this study.
Subjects
Inclusion criteria were: BMI ≥ 25.0 kg/m2; age: 20-64 years old; waist circumference: men ≥ 90 cm, women ≥ 85 cm; exercise: at least 30 minutes, 4 times a week of aerobic exercise. Exclusion criteria were: uncontrolled type 2 diabetes, hypertension, habitual alcohol consumption, cancer, past stroke and renal disease. A total of 515 obese subjects (men 55, women 460, mean age of 41.9 ± 9.8) participated in this program voluntarily. Three-hundred and two subjects who completed at least four weeks of the program were classified into the intention to treat (ITT) group. Among them, 34.3% (177 subjects, 24 men, 153 women, mean age: 44.2 ± 9.3 year-old) completed the 12 week program, which were defined as per protocol (PP) group. One hundred and eight subjects participated in the conventional diet program at the public health center of Ansan in 2006. Among them, 78 subjects (12 men, 66 women, mean age: 44.7 ± 6.2) completed the 12 week program.
Program details
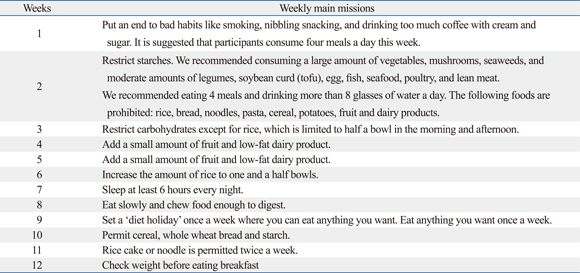
In this study, we applied a special diet program called the PRO Diet which was originally designed by Dr. YW Park. The PRO Diet aims to reduce consumption of refined starches (cooked rice, noodles, white bread) and to encourage the consumption of high protein. Additionally, the PRO Diet encourages the intake of "favorable" carbohydrates with a low glycemic index (GI) and "favorable" fats with high unsaturated fatty acids, while avoiding "unfavorable" carbohydrates with high GI and "unfavorable" fats such as high saturated fatty acids or trans fats. Furthermore, the participants were provided with the following weekly assignments for the 12-week program: see
appendix.
Web-based education and tips were also provided through a website (
www.prodiet.co.kr). In addition, we collected the data of the 78 subjects who followed the 12-week conventional diet program at the public health center of Ansan (South Korea), which was carried out in 2006, and compared anthropometry and nutritional changes between the conventional diet and PRO Diet in PP groups. The conventional diet program stated that all the subjects were educated to increase their daily activity, practice and type of exercise, which they liked, for at least 30 minutes per day, more than three or four times a week, and that each individual underwent an initial nutrition assessment by a registered dietician who educated the subjects about eating a low-calorie diet that would produce a 400-500 kcal daily energy deficit. Furthermore, a behavior modification program encouraged them to increase energy expenditure while reducing intake, with an emphasis on long-term behavior change. However, because there was limited data available on the conventional program carried out by the health promotion department of the public health center and only anthropometric changes were measured, we were unable to have full comparison between the two programs, and were missing such details as macronutrient changes.
Measurements
The height and body weight of the participants were measured while they wore light clothing without shoes. Weight was measured to the nearest 0.1 kg, and height was measured to the nearest centimeter. BMI was calculated as the weight divided by height squared (BMI, kg/m2). Trained nurses measured waist circumference between the lower rib and the iliac crest, as well as the blood pressure after the participants had been at rest for at least 15 minutes (TM-2655P; PMS Instruments, Higashi-Ikebukuro, Toshima-ku, Tokyo, Japan), and checked their nutritional status every 4 weeks. The body composition of each participant was analyzed using the Body Impedance Analysis (In body 7.0, Biospace Co, Seoul, Republic of Korea). Additionally, all subjects underwent a blood test [standard enzymatic measurements of total cholesterol, high-density lipoprotein cholesterol, triglycerides and fasting glucose in fresh serum samples (TBA-200FR, Toshiba, Tokyo, Japan)] at the beginning and end of the 12-week program. We also analyzed changes in macronutrient intake, using a three day recall food diary, with the CAN-Pro 3.0 nutrition analyzer (Seoul, Korea).
Statistics
We conducted ITT (subjects who had completed at least 4 weeks of the program) and PP (subjects who had completed all 12 weeks of the program) analysis to evaluate the results of this study by a paired t-test after 12 weeks. An independent t-test was also used to evaluate the changes between the PRO-Diet and conventional diet program groups after the 12-week program as well as a baseline comparison. All significant values were defined by p < 0.05 as determined by SPSS version 11.5 (SPSS Inc., Chicago, IL, USA).
RESULTS
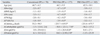
The mean BMI of the PRO Diet program participants was 28.1 ± 3.6 kg/m
2, and their waist circumference was 92.4 ± 7.8 cm; those of conventional diet program participants were 29.4 ± 2.4 kg/m
2 and 97.0 ± 7.4 cm, respectively (
Table 1). Comparisons of anthropometry and nutritional changes between the two programs showed that the PRO Diet (PP group) was more effective than the conventional program in terms of body weight, BMI, waist circumference, fat mass, and fat % mass reduction (conventional program vs. PRO Diet; weight, - 2.3 kg vs. - 4.7 kg,
p < 0.001; BMI, - 1.1 kg/m
2 vs. - 1.9 kg/m
2,
p < 0.001; waist circumference, - 3.3 cm vs. - 6.8 cm,
p < 0.001; fat mass, - 2.0 kg vs. - 4.2 kg,
p < 0.001; fat % mass, - 1.8% vs. - 3.9%,
p < 0.001). Furthermore, total calorie and carbohydrate intake showed significant reductions in PRO Diet. In the ITT group of PRO Diet, body weight was reduced by 3.9 ± 1.3 kg, BMI by 1.6 ± 0.5 kg/m
2, and waist circumference was reduced by 5.4 ± 1.7 cm. Fat mass (- 3.6 kg) and fat % mass (- 3.2%) were also reduced (
Table 2). In the PP group of PRO Diet, secular anthropometric measures also showed significant reduction after 12 weeks of intervention (
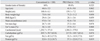
Fig. 1). Both PRO Diet and the conventional program resulted in decreases in systolic and diastolic blood pressure, total cholesterol and triglyceride levels, and in increases in high-density lipoprotein. However, only triglyceride levels were significantly lower in the PRO Diet as compared to the conventional diet program (
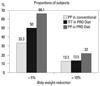
Table 3). The proportions of participants who lost more than 5% and 10% of initial body weight in the ITT group of PRO Diet were 50% and 13.5%, respectively, whereas the proportions in the PP group of PRO Diet were 66.1% and 22%, respectively. In the PP group of conventional program, the percentages of participants who lost more than 5% and 10% of their initial body weight were 33.3% and 13.3%, respectively (
Fig. 2). The overall satisfaction index in the PP group of PRO Diet was over 90%, and there was no report of adverse events (data not shown).
DISCUSSION
In this study, we applied the PRO Diet to conduct a community-based obesity control program for 12 weeks. 177 subjects (34.3%) among 515 participants completed the 12 weeks program despite a lack of rewards or enforcement. The 12-week PRO Diet group experienced greater weight loss than the conventional diet group (Weight loss: - 4.7 vs. - 2.4 kg; BMI: - 1.9 vs. - 1.1 kg/m2; Waist Circumference: - 6.7 vs. - 3.3 cm), suggesting that the PRO Diet is relatively easy for Koreans to practice without professional intervention and showing that the PRO Diet itself was an effective tool for conducting a community-based obesity management program.
There are some diet programs for obese individuals that are low in carbohydrates and high in protein. A meta-analysis
13 of five trials with 447 participants and a recent 1-year trial
14 involving 311 obese women suggest that a low-carbohydrate diet is a feasible alternative to a low-fat diet to lose weight, and may also have favorable metabolic effects. Another study
15 evaluated a low-carbohydrate, high-protein, high-fat (Atkins) diet and a low-calorie, high-carbohydrate, low-fat diet (conventional diet), and found that the low-carbohydrate diet resulted in more weight loss than the conventional diet after the first six months, but the differences were not significant after 1-year. Furthermore, adherence was poor and attrition was high for both diets. Diets that are lower in carbohydrates and higher in protein and fat are not associated with increased risk of coronary heart disease in women.
16 As for protein consumption, a relatively high percentage of energy intake comes from protein. 20% higher protein intake during the weight maintenance phase after the initial weight loss results in a 50% lower weight regain consisting of only fat-free mass, which is linked to increased satiety and decreased energy efficiency.
17 A recent study
18 suggested that energy expenditure is higher when protein is derived from animal proteins rather than plant proteins. However, existing data indicates that a diet using plant-derived proteins may also lead to a considerable weight loss, and that a high-soy-protein and low-fat diet can improve the body composition of overweight and obese people by helping them lose fat while preserving muscle mass.
19 In addition to these findings, a major concern exists regarding using diets that contain animal products for maintaining higher protein content, because of the association of cholesterol and saturated fatty acids with cardiovascular disease. This possible disadvantage could be eliminated by using plant-derived proteins that may have the added benefits of fibers and photochemicals. However, longer-term studies are lacking, and common limitations of dietary trials include high attrition rates (15-50% within a year), small sample size, short duration, lack of adherence assessment, and unequal intervention intensities.
20-
22
A retrospective database analysis
23 of a community-based weight management program for weight loss and modification of cardiovascular risk factors during a 6-month intervention showed an average weight loss of 7.3% (- 9.6 kg) in men and 4.7% (- 4.6 kg) in women. In this program, the guidelines applied were those established by the National Institutes of Health (NIH) and included in the Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults
24 and position statements from the American Dietetic Association and the American College of Sports Medicine.
25,
26 Practically, they applied a low calorie diet, meaning calorie restriction to -1,200 to 1,800 calories daily as appropriate to the individual. Another study, aiming to evaluate the effect of a community-based program on coronary risk reduction, showed that well-designed community-based intervention programs could improve lifestyle choices and health habits.
27 Therefore, the effects of this 12-week PRO Diet on weight loss, BMI and waist circumference were comparable to other previous community-based obesity management programs.
The effect of PRO Diet on cardiovascular risk factors was a significant reduction in blood pressure and triglyceride levels. High-density lipoprotein (HDL) was increased, but this difference was not significant. Blood pressure and triglycerides are components of metabolic syndrome. Many studies
23,
28 have shown that community-based intervention programs could affect metabolic parameters such as blood pressure, triglycerides, low-density lipoprotein, and HDL concentration. The favorable effects on lipids (with a low-carbohydrate diet) and on glycemic control (with the Mediterranean diet) suggest that personal preferences and metabolic considerations may be used to tailor individualized dietary interventions.
29
In Korea, as the economy continues to grow, consumption of processed foods including simple sugars, refined carbohydrates, and trans fats has been increasing, resulting in a tremendous prevalence of obesity. As far as we are aware, obesity is the result of an improper diet, lack of exercise, and sedentary behavior; obese subjects experience difficulty in gaining control of their environment and poor habits. Among others, diet is considered to be the most difficult modifiable factor, as it is not easy to reduce the amount of food, especially carbohydrates. Steamed rice is a staple food for Koreans. In the past, Koreans consumed unrefined rice with a variety of vegetables, cereals, legumes, and fruits. Modern Koreans still eat refined white rice according to the traditional custom, but along with many processed foods, including simple sugars and refined carbohydrates. In order to reduce body weight, obese Koreans should reduce their consumption of carbohydrates, especially simple sugars and refined carbohydrates. Concurrently, Koreans' favorite proteinaceous foods, such as legumes, soy-bean curd, soy milk, mushrooms, nuts, seafood, fish, chicken breast and lean meat, should be encouraged. This is the core nutritional concept of PRO Diet. This diet may appear similar to other very low-carbohydrate diets (such as Atkins), but PRO Diet recommends a diet low in saturated fat, high in oriental protein foods as described above, and avoiding simple sugars and refined starches. PRO Diet also encourages the consumption of a variety of vegetables, mushrooms, seaweeds, and low-GI carbohydrates without considering the total calorie count. In the case of total calorie reduction, it is possible for appetite to increase as basal metabolic rate decreases; therefore, we educate the participants not to decrease total calories, but to increase protein consumption while decreasing total carbohydrates. Furthermore, if the participants avoid simple sugars, and exchange refined carbohydrates, trans-fats, and saturated animal fat for complex carbohydrates, plant fat, unsaturated fish fat or other protein-enriched oriental healthy food, it is quite likely that calculating calories will no longer be necessary. The main concept of PRO Diet is that by following its principles, the total number of calories will be naturally reduced. Indeed, the present PP group showed significantly reduced total calories and carbohydrate consumption even though they were told not to do so. Following the guidelines of the PRO Diet program, we educated participants to increase daily protein consumption; however, consumption of protein increased but not significantly after 12 weeks of intervention. We are not sure why protein consumption did not increase significantly even when the participants were instructed to do so, suggesting that it is very difficult to intentionally increase protein consumption in modern city daily life. In the early stages of the PRO Diet protocol, which consists of a low carbohydrate diet, most of the participants might have gotten used to reduced carbohydrates, rather than increasing the protein content. Thus, they would rather have reduced overall calorie intake via low carbohydrate than high protein consumption. This may imply that a low carbohydrate diet is effective as a short-term obesity intervention program.
PRO Diet includes not only a nutritional program, but also behavioral modification and exercise intervention. In order to encourage behavioral modification, obese subjects were asked to visit their local public health center every week or two to obtain information about diet and exercise as well as tips on how to overcome the bad habits that led to their weight gain. In addition to direct education on behavioral modification, which the participants received from trained nurses, we used also mobile phones to send short weekly messages to all of the service subjects enrolled, and encouraged them to use our web site to obtain more information on obesity, nutrition and exercise. Our previous study of a community-based obesity control program
30 showed that the mobile phone short message service only slightly modified the participants' behavior; nevertheless, it may still have helped somewhat to control the subjects' body weight.
There are some limitations to our study. One is the relatively short duration of the intervention and the high attrition rate, which may have derived from the lack of rewards and compulsion for participation in the program. Another limitation is the small number of subjects and the absence of a proper control group, other than the previous conventional diet program, in order to evaluate the effects of the PRO Diet. As for protein consumption, although we instructed subjects to increase their daily protein intake, these results were not significantly different. Furthermore, there was a lack of variety in age, income level or socioeconomic status of the participants. Nevertheless, this is the first clinical application trial of the PRO Diet in a community-based obesity control program in public health centers in Korea. Community-based obesity control programs are usually used by middle-aged men and women, especially women, and for this reason most public health programs for obesity control are geared towards middle-aged women. Additional long-term and large population-based application of PRO Diet is needed in order to evaluate its long-term efficacy, tolerability and safety, and to determine its effect on weight maintenance as compared to other diet programs.
In conclusion, the PRO Diet, as recommended by the community-based obesity control program, is a well-tolerated and effective tool for weight management. The low carbohydrate component of the PRO Diet was effective in reducing body weight. PRO Diet is not only a nutritional program, but also contains many methods for proper behavior modification. Therefore, PRO Diet, if properly applied to the public health business, may contribute to a decrease in the prevalence of obesity in Korea.






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download