Abstract
Objective
Materials and Methods
Results
Acknowledgments
References
Fig. 1
Myocardial strain measurement by feature tracking method in 43-year-old female patient with acute myocarditis.
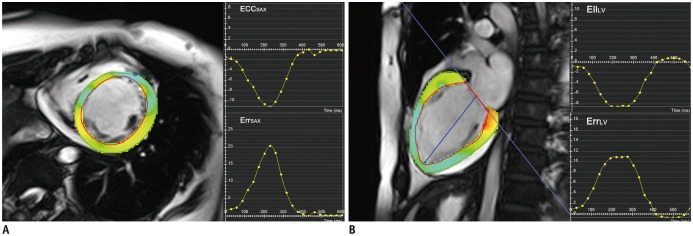
Fig. 2
Receiver operating characteristic curve for prediction of MACE.
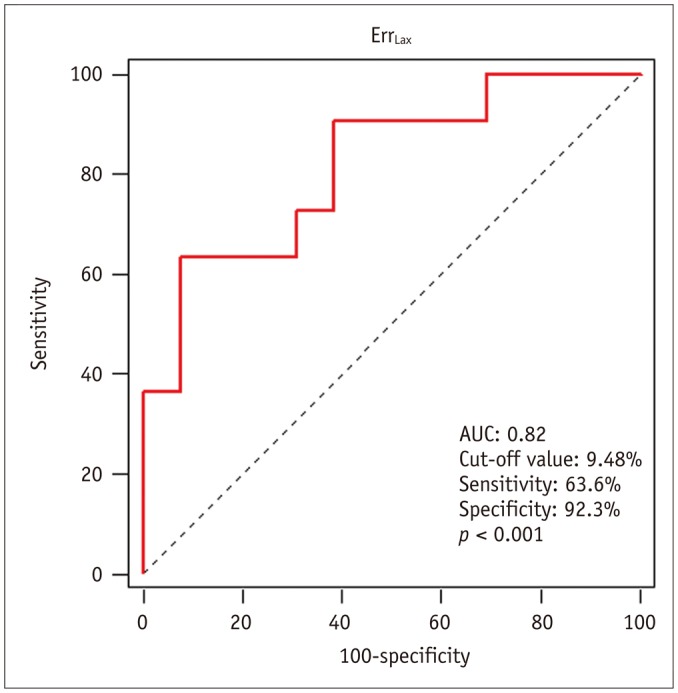
Fig. 3
MACE according to ErrLax or presence of LGE.
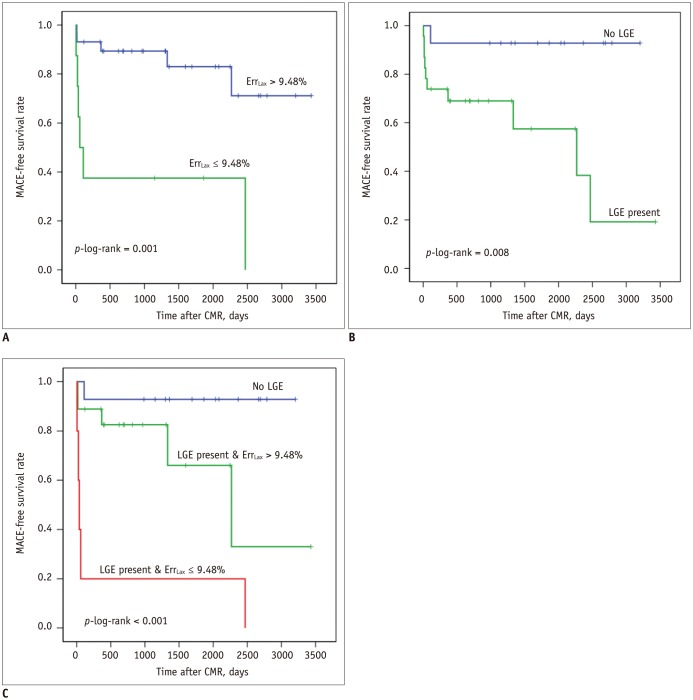
Fig. 4
Receiver operating characteristic curve for prediction of incomplete left ventricular functional recovery.
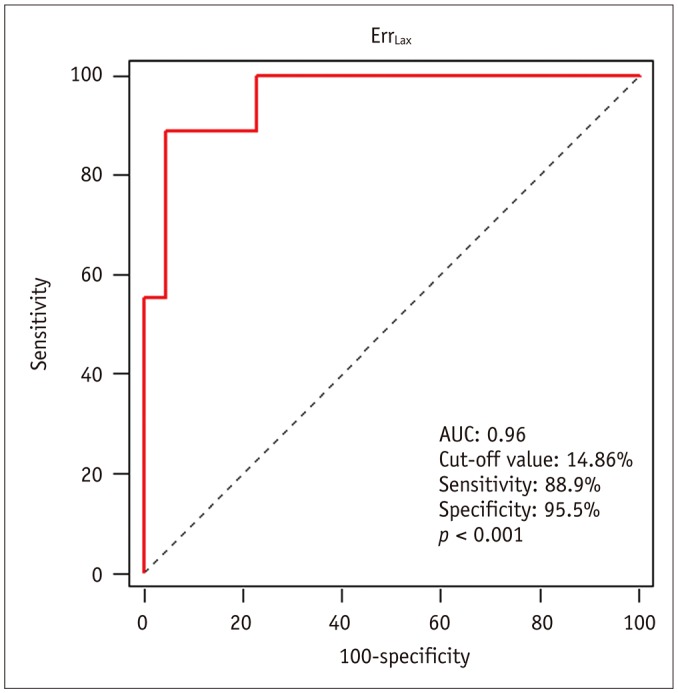
Table 1
Baseline Characteristics of Patients
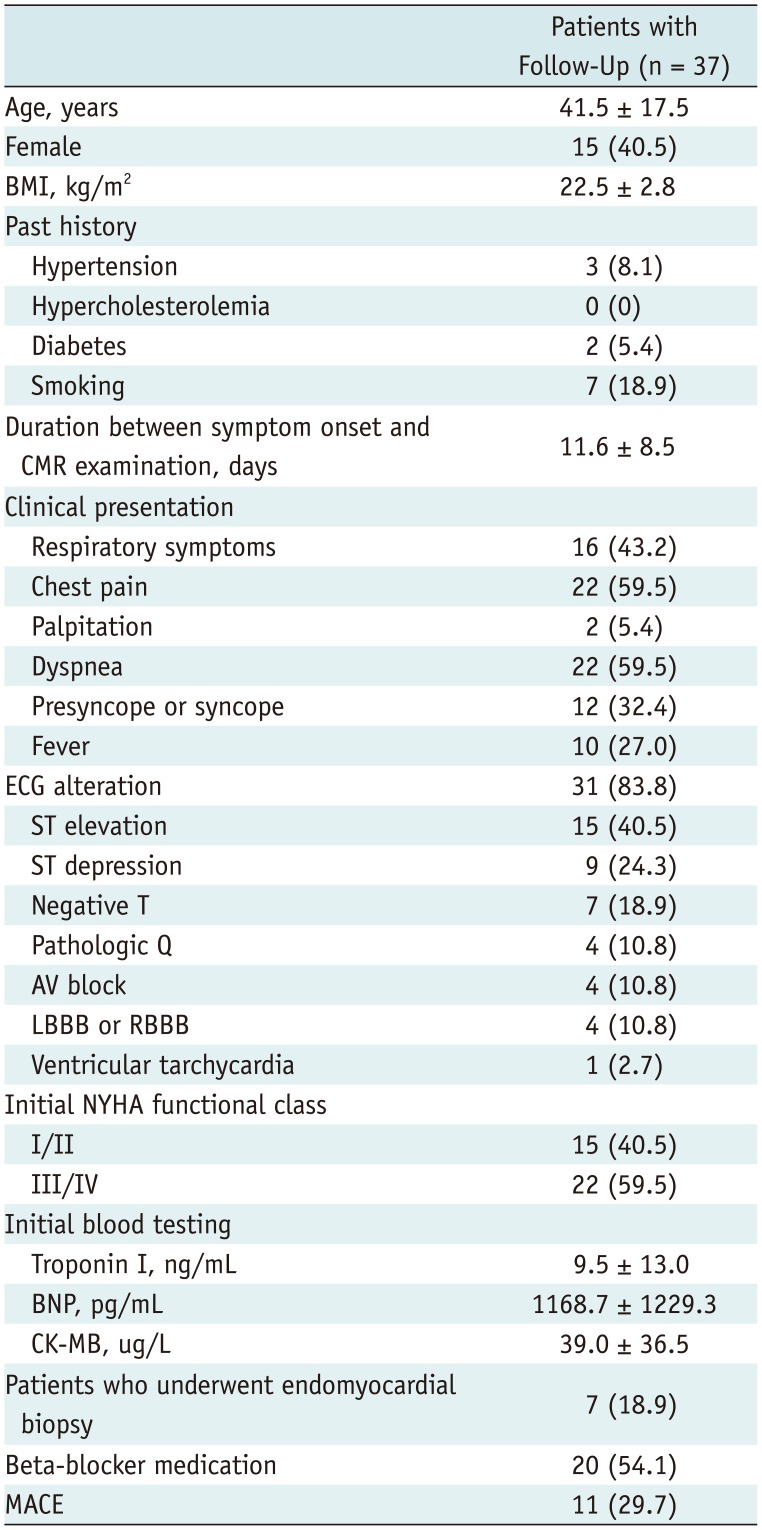
Data are provided as n (%) or mean ± SD. AV = atrioventricular, BMI = body mass index, BNP = brain natriuretic peptide, CK-MB = creatine kinase MB, CMR = cardiovascular magnetic resonance, ECG = electrocardiography, LBBB = left bundle branch block, MACE = major adverse cardiovascular events, NYHA = New York Heart Association, RBBB = right bundle branch block
Table 2
CMR Findings of Patients with Acute Myocarditis and Normal Subjects
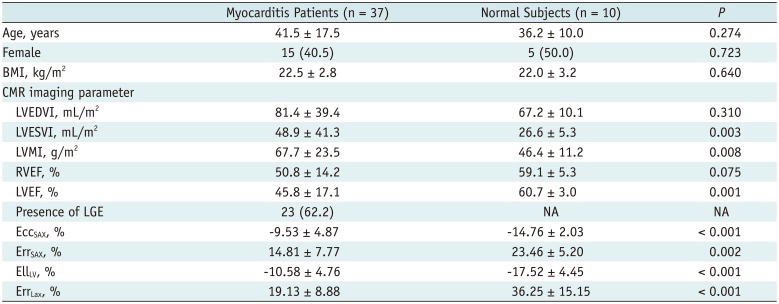
Values are n (%) or means ± SD. BMI = body mass index, CMR = cardiovascular magnetic resonance, EccSAX = LV circumferential strain measured from short-axis cine views, EllLV = LV longitudinal strain measured from long-axis cine views, ErrLax = LV radial strain measured from long-axis cine views, ErrSAX = LV radial strain measured from short-axis cine views, LGE = late gadolinium enhancement, LV = left ventricle, LVEDVI = left ventricular end-diastolic volume index, LVEF = left ventricular ejection fraction, LVESVI = left ventricular end-systolic volume index, LVMI = left ventricular mass index, NA = not applicable, RVEF = right ventricular ejection fraction
Table 3
Comparison of Myocardial Stain Parameters between Myocarditis Patients without and with Preserved EF and Normal Subjects
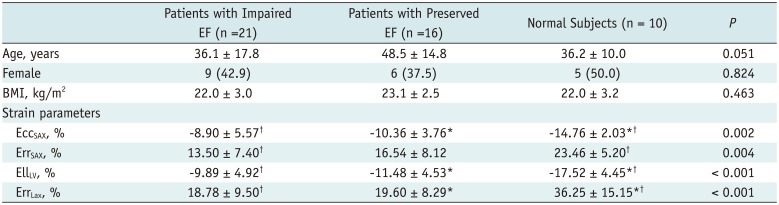
Values are n (%) or means ± SD. *Significantly different between myocarditis patients with preserved EF and normal subjects, †Significantly different between myocarditis patients with impaired EF and normal subjects. BMI = body mass index, EccSAX = LV circumferential strain measured from short-axis cine views, EF = ejection fraction, EllLV = LV longitudinal strain measured from long-axis cine views, ErrLax = LV radial strain measured from long-axis cine views, ErrSAX = LV radial strain measured from short-axis cine views, LV = left ventricle
Table 4
Intra-Observer and Inter-Observer Reproducibility According to Intra-Class Correlation for Strain Quantification on CMR
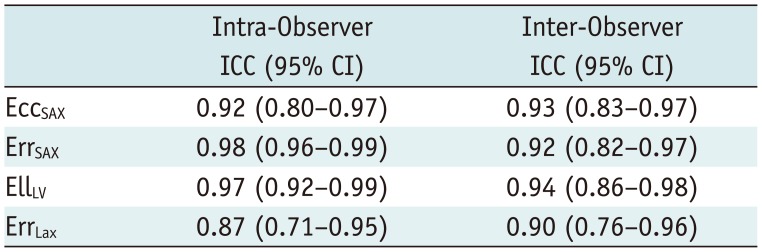
CI = confidence interval, CMR = cardiovascular magnetic resonance, EccSAX = LV circumferential strain measured from short-axis cine views, EllLV = LV longitudinal strain measured from long-axis cine views, ErrLax = LV radial strain measured from long-axis cine views, ErrSAX = LV radial strain measured from short-axis cine views, ICC = intra-class correlation coefficient, LV = left ventricle
Table 5
Univariate Cox Regression Analysis: MACE
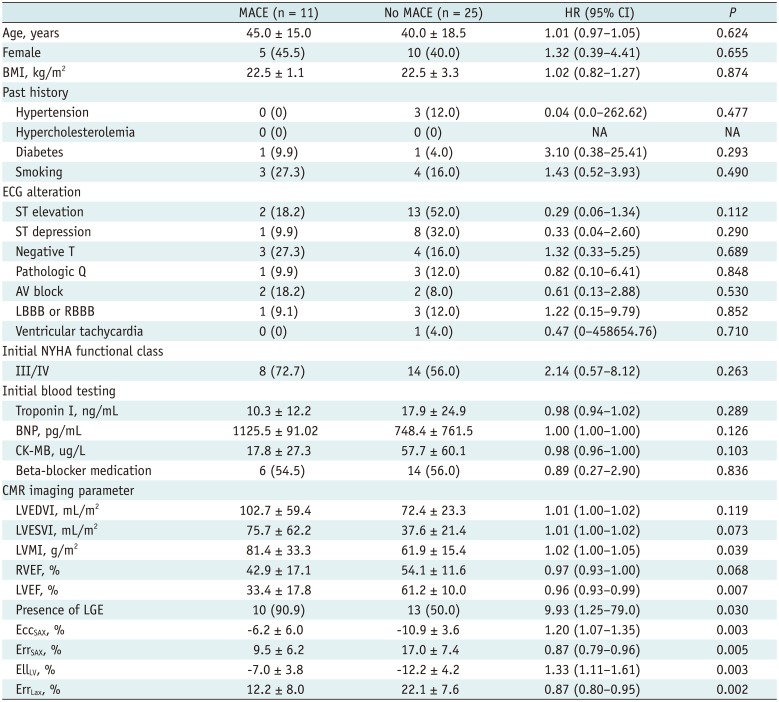
Values are n (%) or mean ± SD. AV = atrioventricular, BMI = body mass index, BNP = brain natriuretic peptide, CI = confidence interval, CK-MB = creatine kinase MB, CMR = cardiovascular magnetic resonance, EccSAX = LV circumferential strain measured from short-axis cine views, ECG = electrocardiography, EllLV = LV longitudinal strain measured from long-axis cine views, ErrLax = LV radial strain measured from long-axis cine views, ErrSAX = LV radial strain measured from short-axis cine views, HR = hazard ratio, LBBB = left bundle branch block, LGE = late gadolinium enhancement, LV = left ventricle, LVEDVI = LV end-diastolic volume index, LVEF = LV ejection fraction, LVESVI = LV end-systolic volume index, LVMI = LV mass index, MACE = major adverse cardiovascular events, NA = not applicable, NYHA = New York Heart Association, RBBB = right bundle branch block, RVEF = right ventricular ejection fraction
Table 6
Univariate Analysis: Incomplete Left Ventricular Functional Recovery
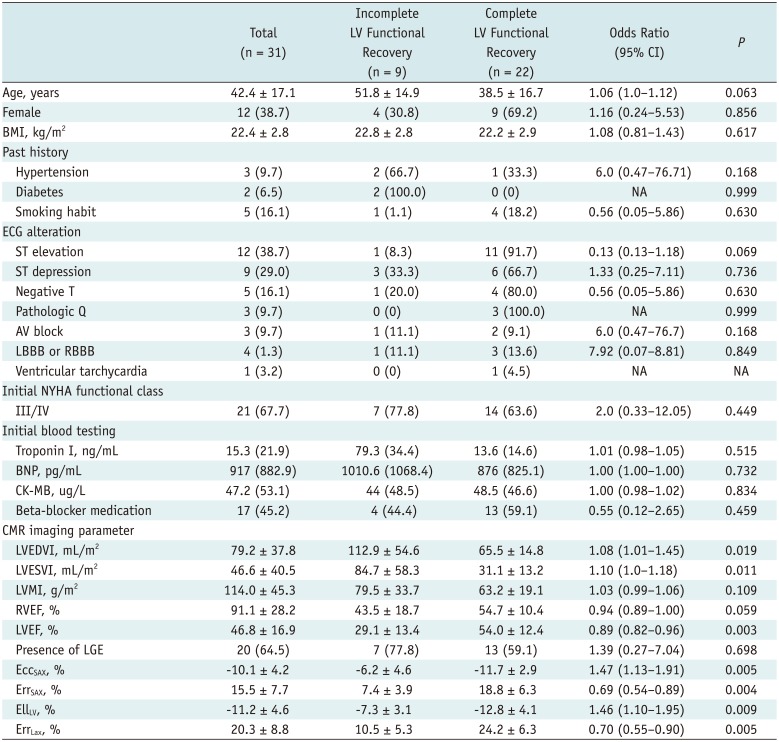
Values are n (%) or means ± SD. AV = atrioventricular, BMI = body mass index, BNP = brain natriuretic peptide, CK-MB = creatine kinase MB, CMR = cardiovascular magnetic resonance, EccSAX = LV circumferential strain measured from short-axis cine views, ECG = electrocardiography, EllLV = LV longitudinal strain measured from long-axis cine views, ErrLax = LV radial strain measured from long-axis cine views, ErrSAX = LV radial strain measured from short-axis cine views, LBBB = left bundle branch block, LGE = late gadolinium enhancement, LV = left ventricle, LVEDVI = LV end-diastolic volume index, LVEF = LV ejection fraction, LVESVI = LV end-systolic volume index, LVMI = LV mass index, MACE = major adverse cardiovascular events, NA = not applicable, NYHA = New York Heart Association, RBBB = right bundle branch block, RVEF = right ventricular ejection fraction




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download