Abstract
Objective
To seek for the ultrasound (US) findings of partially cystic thyroid nodules that are associated with malignancy.
Materials and Methods
We reviewed the US characteristics of 22 surgically confirmed partially cystic papillary carcinomas, and compared them with those of 80 benign partially cystic nodules. The review cases were selected in a random order from a total of 1029 partially cystic nodules that were diagnosed with an US-guided fine needle aspiration biopsy over a period of 8 years (June 2003 to October 2010) at our institution.
Results
In partially cystic thyroid nodules, a taller-than-wide shape (100%, p < 0.001) and spiculated or microlobulated margin (58.3%, p = 0.003) were significantly associated with malignancy. In terms of internal solid portion of the nodule, eccentric configuration (68.0%, p < 0.001), non-smooth margin (81.3%, p < 0.001), hypoechogenecity (30.0%, p < 0.042), and microcalcification (89.5%, p < 0.001) were more frequently demonstrated in malignant nodules than benign ones.
Partially cystic nodules are nodules that have both solid and cystic components, and comprise of 18% to 35% of surgical specimens (1, 2). Since most partially cystic thyroid nodules are the result of a degenerative process, arising from underlying benign lesions, such as nodular hyperplasia, the management of partially cystic thyroid nodules is often undervalued. However, thyroid carcinomas can also show a cystic change (10-28% of papillary thyroid carcinomas), often related to size (3, 4). The rate of malignancy for partially cystic thyroid nodules was 5.2% in a recent study (5). Thus far, there is little information regarding the ultrasound (US) findings of partially cystic nodules, associated with malignancy. Lee et al. (6) reported that more than 50% of solid portions, eccentric solid portions, and microcalcifications are associated with an increased risk of malignancy. Kim et al. (5) reported that an eccentric solid portion with an acute angle, microcalcifications, and macrolobulation or irregular free margin can significantly increase the risk of malignancy.
Current guidelines in Korea (7) only consider the size (> 1 cm) as a criterion for fine needle aspiration (FNA), regardless of the cystic portion. Similar revised guidelines from the American Thyroid Association (8) consider 1.5-2.0 cm (in nodules with any suspicious US features) or 2.0 cm (in nodules without any suspicious US features) as the threshold size for FNA of partially cystic nodules. On the other hand, the guidelines of the American Association of Clinical Endocrinologists/Associazione Medici Endocrinologi/European Thyroid Association recommend FNA for nodules larger than 1.0 cm that are solid and hypoechoic nodules (9). There were no comments concerning the US features, which suggest malignancy in partially cystic nodules. We compared the US findings of partially cystic papillary carcinomas to those of benign nodules.
We reviewed the surgical excision data of our hospital from June 2003 to October 2010, and enrolled 22 patients (15 women and 7 men ranging in ages from 17 to 70 years, mean 50.8 years) diagnosed with papillary thyroid carcinomas with partially cystic feature in the US images. Next, we randomly selected 80 of 1029 patients for the control group, using the random sampling function of a software package {PASW Statistics 18 (Statistical Package for the Social Sciences [SPSS] lnc., Chicago, IL, USA)}. These patients were diagnosed with benign partially cystic thyroid nodules, at both initial and repeat FNA, during the same period. The control group consisted of 64 women and 16 men, ranging in ages from 33 to 73 years (mean 52.3 years), and the cytological diagnosis of nodules were as follows: nodular hyperplasia (n = 69), colloid with benign follicular cells (n = 7), and benign follicular lesion (n = 4).
The US and US-guided FNA were performed by board-certified two radiologists with 6 and 7 years of experience in thyroid imaging. LOGIQ 9 (GE medical systems, Milwaukee, WI, USA) high-frequency 13-MHz linear transducers were used. The cytology was interpreted by cytopathologists and a specimen was "adequate" if there was a minimum of six groupings of well-preserved thyroid cells, each consisting of at least 10 cells per group.
Partially cystic nodules were defined by the presence of any anechoic components in US, except completely anechoic nodules. All US images of partially cystic nodules were retrospectively evaluated by two board-certified radiologists in consensus, both of whom have 6 and 7 years of experience in thyroid imaging. The images were placed on a picture archiving and communication system workstation (Infinitt Technology, Seoul, Korea), and were presented at random for surgical pathology.
Each nodule was evaluated for the following US findings of entire nodule: size (the longest diameter), internal content (predominantly solid vs. predominantly cystic vs. spongiform), shape (ovoid to round vs. taller-than-wide vs. irregular), and margin (smooth vs. spiculated or microlobulated vs. ill-defined). US examination of internal solid portion included configuration (eccentric vs. non eccentric) (Figs. 1, 2), margin (smooth vs. non-smooth), echogenecity (markedly hypoechoic vs. hypoechoic vs. isoechoic vs. hyperechoic), and calcification (microcalcifications vs. macrocalcifications vs. rim calcifications vs. none). We described the margin (of entire nodule), shape, echogenecity, and calcification, using terminology recommended in 2011 by the Korean Society of Thyroid Radiology (7). A spongiform internal content also followed that group's definition (7) as the aggregation of multiple microcystic components in more than 50% of the volume of the nodule, resulting in a honeycomb or "puff pastry" appearance.
An eccentric configuration had an internal solid portion, which was not located in the center, and was abutted on only one side of the cyst wall. A non-eccentric configuration was defined as all partially cystic thyroid nodules other than the eccentric configuration, including spongiform nodules. The margin of the internal solid portion is a description that has not been commonly used previously and is defined as the interface between the cystic component and the solid component (Fig. 3). In the aforementioned standardized terminology (7), an ill-defined margin of the entire nodule is defined by the inability to differentiate the tumor from that of the normal parenchyma. We classified the margin of internal solid portion, as smooth or non-smooth.
The χ2 test or Fisher's exact test was used to compare the quantitative variables, while the Student's t test and Mann-Whitney U test were used to evaluate the size, as well as the longest diameter.
A two-tailed p value of < 0.05 indicated a significant statistical difference. Statistical analysis was performed by using PASW Statistics 18 (SPSS lnc., Chicago, IL, USA).
Malignancy in partially cystic nodule can be characterized by a taller-than-wide shape (100%, p < 0.001) and spiculated or microlobulated margin (58.3%, p = 0.003) of the entire nodule. Further findings of internal solid portion included an eccentric configuration (68.0%, p < 0.001), non-smooth margin (81.3%, p < 0.001), hypoechogenecity (30.0%, p = 0.042) and microcalcifications (89.5%, p < 0.001). Predominantly, solid nodules were not significantly associated with malignancy.
The characteristics of a benign nodule included spongiform internal content (100%, p = 0.036), ovoid to round shape (83%, p = 0.001), and smooth margin (84.3%, p < 0.001) in the entire nodule, while the internal solid portion included a non eccentric configuration (93.5%, p < 0.001), smooth margin (89.5%, p < 0.001), isoechogenecity (89.6%, p = 0.010), and lacking calcifications (96.1%, p < 0.001). The US features of all 102 cases, including those without significant differences, are summarized in Table 1.
There are few reports, which compares the US findings between malignant and benign partially cystic nodules. Our study is notable for analyzing the US findings of both the entire nodule and its internal solid portion, following the standardized terminology recommended by the Korean Society of Thyroid Radiology (7). However, we did need to re-categorize the internal content. The statistically significant US findings of the entire nodule for the depiction of malignancy were a taller-than-wide shape and spiculated or microlobulated margin. The statistically significant US findings of the internal solid portion were an eccentric configuration, non-smooth margin, hypoechogenecity, and microcalcifications. These findings do not differ greatly from the previously suggested US criteria (7), indicating those criteria that are applicable to partially cystic nodules. However, we discovered that the marked hypoechogenecity of a nodule did not differ significantly, unlike the previous research (8, 10-12). This may be due to the easier sonic transmission through the cystic component of a partially cystic nodule, compared to a solid one as suggested by Kim et al. (5).
Compared with two recent studies (5, 6) regarding partially cystic nodules, we confirmed that the eccentric configuration and microcalcifications of internal solid portion, in partially cystic nodules, were significantly more frequent in malignant partially cystic nodules. This result is supported by a previous report (13), describing the malignant cells as more likely to be located in the intracystic pedunculated mass and/or the pericystic region than in the cyst wall (Figs. 3, 4). In other words, malignant partially cystic nodules are more likely to be an intracystic mass, protruding from the wall than the diffuse lesion, which is circumferentially located within the cystic wall that would result in a concentric configuration. A recent study (5) that subdivided the eccentric configuration into either an acute angle or a blunt angle to the adjacent cyst wall found that only the cases with an acute angle were associated with malignancy. In our study, if the margin of internal solid portion was smooth, the partially cystic nodule was more likely to be benign, in accordance with a previous study (5). However, we subdivided the margin of the internal solid portion based upon whether it was smooth or not. That characteristic, the lack of smoothness of the margin of the partially cystic nodule, was indicative with statistical significance of malignancy. Our finding can be explained by the histologic tendency of malignancy to grow unevenly and infiltratively without pseudocapsule formation (14). Most notably, the proportion of solid components of partially cystic thyroid nodules cannot predict a malignancy. Thus, radiologists should not overlook predominantly cystic nodules (Figs. 4, 5).
The limitations of this study are as follows: the number of malignant cases included in this study (n = 22) was relatively small. The diagnoses of benign nodules were based on cytologic, rather than pathologic findings, because their diagnoses from FNA were not considered indications for surgery. Since this study was not a prospective study that included all partially cystic nodules as candidates of FNA, a selection bias was inevitable. We assumed an echogenic spot as either microcalcification or macrocalcification, depending on its visualized size. However, each of these echogenic spots was not confirmed pathologically. Finally, we tried to consider all tiny echogenic spots, except for comet-tail artifacts, as microcalcifications, because after surgery, they were mostly confirmed pathologically.
In conclusion, the US findings of internal cystic portion are important in partially cystic thyroid nodules. A non-smooth margin, eccentric configuration, hypoechogenecity, and microcalcifications are the US findings of the internal solid portion, which can suggest malignancy. These findings are useful for accurate differential diagnosis of malignant partially cystic thyroid nodules.
Figures and Tables
Fig. 1
Longitudinal ultrasound image of papillary thyroid carcinoma in 53-year-old woman shows predominantly cystic nodule. Entire nodule has smooth margin. Internal protruding eccentric solid position contains multiple punctuate round echogenic foci suggesting microcalcifications.
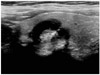
Fig. 2
Example of non-eccentric configuration of internal solid portion.
Transverse (A) and longitudinal (B) US images show partially cystic nodule with isoechoic internal solid portion in 57-year-old woman. Entire nodule has ill-defined margin (arrows). Nodular hyperplasia was diagnosed by US-guided fine needle aspiration. US = ultrasound

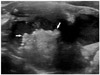
Fig. 3
Transverse ultrasound image of predominantly cystic nodule in 69-year-old woman. Eccentric solid position protruded internally and contained multiple microcalcifications. Note difference between smooth margin of entire nodule (arrows) and non-smooth margin of internal solid portion (arrowheads). Papillary thyroid carcinoma was diagnosed by fine needle aspiration and surgery.

Fig. 4
Longitudinal ultrasound image of predominantly cystic nodule in 66-year-old woman shows eccentric configuration. Note difference between smooth margin of entire nodule (arrows) and non-smooth margin of internal solid portion (arrowheads). This lesion was surgically confirmed as papillary thyroid carcinoma despite substantial cystic portion.
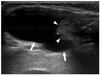
Fig. 5
Transverse ultrasound image of predominantly cystic nodule in 63-year-old woman shows eccentric configuration of internal solid portion with multiple microcalcifications. Note non-smooth margin of internal solid portion (arrows). This lesion was surgically confirmed as papillary thyroid carcinoma despite substantial cystic portion.
References
1. McHenry CR, Slusarczyk SJ, Khiyami A. Recommendations for management of cystic thyroid disease. Surgery. 1999. 126:1167–1171. discussion 1171-1172.
2. Khoo ML, Asa SL, Witterick IJ, Freeman JL. Thyroid calcification and its association with thyroid carcinoma. Head Neck. 2002. 24:651–655.
3. do Rosário PW, Fagundes TA, Maia FF. Ultrasonographic features of papillary thyroid carcinoma. J Ultrasound Med. 2004. 23:572.
4. Peccin S, de Castsro JA, Furlanetto TW, Furtado AP, Brasil BA, Czepielewski MA. Ultrasonography: is it useful in the diagnosis of cancer in thyroid nodules? J Endocrinol Invest. 2002. 25:39–43.
5. Kim DW, Lee EJ, In HS, Kim SJ. Sonographic differentiation of partially cystic thyroid nodules: a prospective study. AJNR Am J Neuroradiol. 2010. 31:1961–1966.
6. Lee MJ, Kim EK, Kwak JY, Kim MJ. Partially cystic thyroid nodules on ultrasound: probability of malignancy and sonographic differentiation. Thyroid. 2009. 19:341–346.
7. Moon WJ, Baek JH, Jung SL, Kim DW, Kim EK, Kim JY, et al. Ultrasonography and the ultrasound-based management of thyroid nodules: consensus statement and recommendations. Korean J Radiol. 2011. 12:1–14.
8. Kim SH, Kim BS, Jung SL, Lee JW, Yang PS, Kang BJ, et al. Ultrasonographic findings of medullary thyroid carcinoma: a comparison with papillary thyroid carcinoma. Korean J Radiol. 2009. 10:101–105.
9. Gharib H, Papini E, Paschke R, Duick DS, Valcavi R, Hegedüs L, et al. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and EuropeanThyroid Association Medical Guidelines for Clinical Practice for the Diagnosis and Management of Thyroid Nodules. Endocr Pract. 2010. 16:Suppl 1. 1–43.
10. Kim EK, Park CS, Chung WY, Oh KK, Kim DI, Lee JT, et al. New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am J Roentgenol. 2002. 178:687–691.
11. Moon WJ, Jung SL, Lee JH, Na DG, Baek JH, Lee YH, et al. Benign and malignant thyroid nodules: US differentiation--multicenter retrospective study. Radiology. 2008. 247:762–770.
12. Lee YH, Kim DW, In HS, Park JS, Kim SH, Eom JW, et al. Differentiation between benign and malignant solid thyroid nodules using an US classification system. Korean J Radiol. 2011. 12:559–567.
13. Hiromura T, Nojima T, Morita Y, Choji K, Nakada K, Tsukamoto E, et al. Cystic papillary carcinoma of the thyroid--sonographic-pathologic correlation. Nihon Igaku Hoshasen Gakkai Zasshi. 1990. 50:40–47.
14. Oertel YC, Oertel JE. Wartofsky L, Nostrand D, editors. Papillary Carcinoma: Cytology and Pathology. Thyroid Cancer. 2006. Totowa: Humana Press;263–270.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download