1. Hahn WH, Chang JY, Chang YS, Shim KS, Bae CW. Recent trends in neonatal mortality in very low birth weight Korean infants: in comparison with Japan and the USA. J Korean Med Sci. 2011; 26:467–473.
2. Bae CW. The history of neonatology in Korea. J Korean Med Assoc. 2016; 59:490–497.
3. Chang YS, Park HY, Park WS. The Korean Neonatal Network: an overview. J Korean Med Sci. 2015; 30:Suppl 1. S3–S11.
4. Korean Neonatal Network. Korean Neonatal Network 2013 KNN newsletter [Internet]. accessed on 10 March 2017. Available at
http://www.knn.or.kr/index.jsp.
5. Park DK, Kil CH, Bae CW. Neonatal statistics of Korea in 2002: collective results of live-births, and neonatal mortality rates from 62 hospitals. J Korean Soc Neonatol. 2004; 11:122–129.
6. Hahn WH, Chang JY, Bae CW. Birth statistics and mortality rates for neonatal intensive care units in Korea during 2007: collective results from 57 hospitals. J Korean Soc Neonatol. 2009; 16:36–47.
7. Chang YS. The Survey on the Actual Conditions of Neonatal Intensive Care Units and Analysis of Survival Rate of High-risk Newborn Infants. Seoul: Korea Health Promotion Institute;2010.
8. The Executive Committee of Korean Neonatal Network. Korean Neonatal Network Annual Report 2013. Cheongju: Korea Centers for Disease Control and Prevention;2014.
9. The Executive Committee of Korean Neonatal Network. Korean Neonatal Network Annual Report 2014. Cheongju: Korea Centers for Disease Control and Prevention;2015.
10. The Executive Committee of Korean Neonatal Network. Korean Neonatal Network Annual Report 2015. Sejong: Korea Centers for Disease Control and Prevention;2016.
11. Lee BS, Moon WH, Park EA. Real-time data display system of the Korean Neonatal Network. J Korean Med Sci. 2015; 30:Suppl 1. S12–S18.
12. Choi CW, Park MS. Data management and site-visit monitoring of the multi-center registry in the Korean Neonatal Network. J Korean Med Sci. 2015; 30:Suppl 1. S19–S24.
13. Shah PS, Lee SK, Lui K, Sjörs G, Mori R, Reichman B, Håkansson S, Feliciano LS, Modi N, Adams M, et al. The International Network for Evaluating Outcomes of very low birth weight, very preterm neonates (iNeo): a protocol for collaborative comparisons of international health services for quality improvement in neonatal care. BMC Pediatr. 2014; 14:110.
14. Shah PS, Lui K, Sjörs G, Mirea L, Reichman B, Adams M, Modi N, Darlow BA, Kusuda S, San Feliciano L, et al. Neonatal outcomes of very low birth weight and very preterm neonates: an international comparison. J Pediatr. 2016; 177:144–152.e6.
15. Cust AE, Darlow BA, Donoghue DA; Australian and New Zealand Neonatal Network (ANZNN). Outcomes for high risk New Zealand newborn infants in 1998–1999: a population based, national study. Arch Dis Child Fetal Neonatal Ed. 2003; 88:F15–F22.
16. Lee SK, McMillan DD, Ohlsson A, Pendray M, Synnes A, Whyte R, Chien LY, Sale J. Variations in practice and outcomes in the Canadian NICU network: 1996–1997. Pediatrics. 2000; 106:1070–1079.
17. Bader D, Kugelman A, Boyko V, Levitzki O, Lerner-Geva L, Riskin A, Reichman B; Israel Neonatal Network. Risk factors and estimation tool for death among extremely premature infants: a national study. Pediatrics. 2010; 125:696–703.
18. Kusuda S, Fujimura M, Sakuma I, Aotani H, Kabe K, Itani Y, Ichiba H, Matsunami K, Nishida H; Neonatal Research Network, Japan. Morbidity and mortality of infants with very low birth weight in Japan: center variation. Pediatrics. 2006; 118:e1130–e1138.
19. Moro M, Pérez-Rodriguez J, Figueras-Aloy J, Fernández C, Doménech E, Jiménez R, Pérez-Sheriff V, Quero J, Roques V. Grupo SEN1500. Predischarge morbidities in extremely and very low-birth-weight infants in Spanish neonatal units. Am J Perinatol. 2009; 26:335–343.
20. EXPRESS Group. Fellman V, Hellström-Westas L, Norman M, Westgren M, Källén K, Lagercrantz H, Marsál K, Serenius F, Wennergren M. One-year survival of extremely preterm infants after active perinatal care in Sweden. JAMA. 2009; 301:2225–2233.
21. Rüegger C, Hegglin M, Adams M, Bucher HU; Swiss Neonatal Network. Population based trends in mortality, morbidity and treatment for very preterm- and very low birth weight infants over 12 years. BMC Pediatr. 2012; 12:17.
22. Wong HS, Santhakumaran S, Statnikov Y, Gray D, Watkinson M, Modi N; UK Neonatal Collaborative. Retinopathy of prematurity in English neonatal units: a national population-based analysis using NHS operational data. Arch Dis Child Fetal Neonatal Ed. 2014; 99:F196–F202.
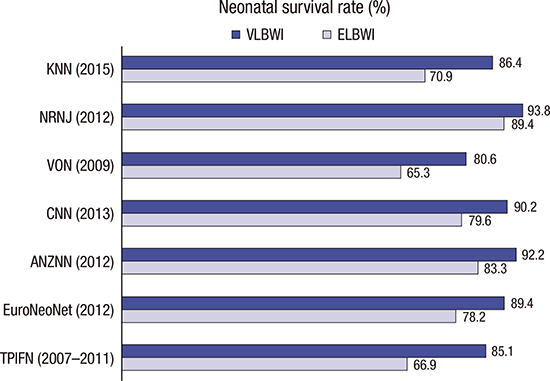
23. Shim JW, Jin HS, Bae CW. Changes in survival rate for very-low-birth-weight infants in Korea: comparison with other countries. J Korean Med Sci. 2015; 30:Suppl 1. S25–S34.
25. Horbar JD, Carpenter JH, Badger GJ, Kenny MJ, Soll RF, Morrow KA, Buzas JS. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics. 2012; 129:1019–1026.
29. Su YY, Wang SH, Chou HC, Chen CY, Hsieh WS, Tsao PN, Tsou KI; Taiwan Premature Infant Follow-up Network. Morbidity and mortality of very low birth weight infants in Taiwan-changes in 15 years: a population based study. J Formos Med Assoc. 2016; 115:1039–1045.
30. Kim HS. Evaluation of Performance and Efficacy in Operation of Neonatal Intensive Care Unit. Seoul: Seoul National University Hospital;2012.
31. Chang YS. Future of neonatology in Korea: the way forward. J Korean Med Assoc. 2016; 59:506–513.
32. Tyson JE, Parikh NA, Langer J, Green C, Higgins RD; National Institute of Child Health and Human Development Neonatal Research Network. Intensive care for extreme prematurity--moving beyond gestational age. N Engl J Med. 2008; 358:1672–1681.
33. Field DJ, Dorling JS, Manktelow BN, Draper ES. Survival of extremely premature babies in a geographically defined population: prospective cohort study of 1994–9 compared with 2000–5. BMJ. 2008; 336:1221–1223.
34. Larroque B, Bréart G, Kaminski M, Dehan M, André M, Burguet A, Grandjean H, Ledésert B, Lévêque C, Maillard F, et al. Survival of very preterm infants: Epipage, a population based cohort study. Arch Dis Child Fetal Neonatal Ed. 2004; 89:F139–F144.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download