1. Mahajan A, Ho H, Sauer B, Phillips MS, Shami VM, Ellen K, Rehan M, Schmitt TM, Kahaleh M. Temporary placement of fully covered self-expandable metal stents in benign biliary strictures: midterm evaluation (with video). Gastrointest Endosc. 2009; 70:303–309.
2. Chan CH, Telford JJ. Endoscopic management of benign biliary strictures. Gastrointest Endosc Clin N Am. 2012; 22:511–537.
3. van Berkel AM, Cahen DL, van Westerloo DJ, Rauws EA, Huibregtse K, Bruno MJ. Self-expanding metal stents in benign biliary strictures due to chronic pancreatitis. Endoscopy. 2004; 36:381–384.
4. Devière J, Nageshwar Reddy D, Püspök A, Ponchon T, Bruno MJ, Bourke MJ, Neuhaus H, Roy A, González-Huix Lladó F, Barkun AN, et al. Successful management of benign biliary strictures with fully covered self-expanding metal stents. Gastroenterology. 2014; 147:385–395.
5. Kountouras J, Billing BH, Scheuer PJ. Prolonged bile duct obstruction: a new experimental model for cirrhosis in the rat. Br J Exp Pathol. 1984; 65:305–311.
6. Hirazawa K, Oka M, Ogura Y, Miyahara M, Hazama S, Suzuki T. New technique for inducing reversible obstructive jaundice in the rat. Eur Surg Res. 1997; 29:195–201.
7. Ker CG, Wu SC. A simple animal model for inducing and releasing surgical jaundice in rats. Gaoxiong Yi Xue Ke Xue Za Zhi. 1992; 8:520–524.
8. Cho YK, Kim JK, Kim MY, Rhim H, Han JK. Systematic review of randomized trials for hepatocellular carcinoma treated with percutaneous ablation therapies. Hepatology. 2009; 49:453–459.
9. Rustagi T, Jamidar PA. Intraductal radiofrequency ablation for management of malignant biliary obstruction. Dig Dis Sci. 2014; 59:2635–2641.
10. Hu B, Gao DJ, Wu J, Wang TT, Yang XM, Ye X. Intraductal radiofrequency ablation for refractory benign biliary stricture: pilot feasibility study. Dig Endosc. 2014; 26:581–585.
11. Steel AW, Postgate AJ, Khorsandi S, Nicholls J, Jiao L, Vlavianos P, Habib N, Westaby D. Endoscopically applied radiofrequency ablation appears to be safe in the treatment of malignant biliary obstruction. Gastrointest Endosc. 2011; 73:149–153.
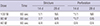
12. Rumalla A, Petersen BT, Baron TH, Burgart LJ, Herman LJ, Wiersema MJ, Gostout CJ. Development of a swine model for benign stenosis of the bile duct by endoscopic application of intraluminal thermal injury. Gastrointest Endosc. 2003; 57:73–77.
13. Nishikawa H, Inuzuka T, Takeda H, Nakajima J, Sakamoto A, Henmi S, Matsuda F, Eso Y, Ishikawa T, Saito S, et al. Percutaneous radiofrequency ablation therapy for hepatocellular carcinoma: a proposed new grading system for the ablative margin and prediction of local tumor progression and its validation. J Gastroenterol. 2011; 46:1418–1426.
14. Shin JH, Baek JH, Ha EJ, Lee JH. Radiofrequency ablation of thyroid nodules: basic principles and clinical application. Int J Endocrinol. 2012; 2012:919650.
15. Judah JR, Draganov PV. Endoscopic therapy of benign biliary strictures. World J Gastroenterol. 2007; 13:3531–3539.
16. Corvera CU, Blumgart LH, Darvishian F, Klimstra DS, DeMatteo R, Fong Y, D’Angelica M, Jarnagin WR. Clinical and pathologic features of proximal biliary strictures masquerading as hilar cholangiocarcinoma. J Am Coll Surg. 2005; 201:862–869.
17. Zhao DF, Chen DZ, Lv JS, Lang R, Jin ZK, Qing H. Establishment of an animal model of biliary ischemic stenosis with clamping in mice. Transplant Proc. 2008; 40:1303–1305.
18. Wang Y, Liang Y, Wang W, Jin R, Cai X. Management of electrothermal injury of common bile duct with a degradable biliary stent: an experimental study in a porcine model. J Gastrointest Surg. 2013; 17:1760–1765.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download