1. Awad H, Santilli S, Ohr M, Roth A, Yan W, Fernandez S, Roth S, Patel V. The effects of steep trendelenburg positioning on intraocular pressure during robotic radical prostatectomy. Anesth Analg. 2009; 109:473–478.
2. Molloy BL. Implications for postoperative visual loss: steep trendelenburg position and effects on intraocular pressure. AANA J. 2011; 79:115–121.
3. Weber ED, Colyer MH, Lesser RL, Subramanian PS. Posterior ischemic optic neuropathy after minimally invasive prostatectomy. J Neuroophthalmol. 2007; 27:285–287.
4. Vaajanen A, Mervaala E, Oksala O, Vapaatalo H. Is there a relationship between blood pressure and intraocular pressure? An experimental study in hypertensive rats. Curr Eye Res. 2008; 33:325–332.
5. Farag E, Sessler DI, Kovaci B, Wang L, Mascha EJ, Bell G, Kalfas I, Rockwood E, Kurz A. Effects of crystalloid versus colloid and the alpha-2 agonist brimonidine versus placebo on intraocular pressure during prone spine surgery: a factorial randomized trial. Anesthesiology. 2012; 116:807–815.
6. Kaya FN, Yavascaoglu B, Baykara M, Altun GT, Gülhan N, Ata F. Effect of oral gabapentin on the intraocular pressure and haemodynamic responses induced by tracheal intubation. Acta Anaesthesiol Scand. 2008; 52:1076–1080.
7. Pal CK, Ray M, Sen A, Hajra B, Mukherjee D, Ghanta AK. Changes in intraocular pressure following administration of suxamethonium and endotracheal intubation: influence of dexmedetomidine premedication. Indian J Anaesth. 2011; 55:573–577.
8. Lam AK, Douthwaite WA. Does the change of anterior chamber depth or/and episcleral venous pressure cause intraocular pressure change in postural variation? Optom Vis Sci. 1997; 74:664–667.
9. Cantor LB. The evolving pharmacotherapeutic profile of brimonidine, an alpha 2-adrenergic agonist, after four years of continuous use. Expert Opin Pharmacother. 2000; 1:815–834.
10. Friberg TR, Weinreb RN. Ocular manifestations of gravity inversion. JAMA. 1985; 253:1755–1757.
11. Hayreh SS. Ischemic optic neuropathy. Prog Retin Eye Res. 2009; 28:34–62.
12. Macri FJ, Cevario SJ. Clonidine. Arch Ophthalmol. 1978; 96:2111–2113.
13. Vartiainen J, MacDonald E, Urtti A, Rouhiainen H, Virtanen R. Dexmedetomidine-induced ocular hypotension in rabbits with normal or elevated intraocular pressures. Invest Ophthalmol Vis Sci. 1992; 33:2019–2023.
14. Donello JE, Padillo EU, Webster ML, Wheeler LA, Gil DW. alpha(2)-adrenoceptor agonists inhibit vitreal glutamate and aspartate accumulation and preserve retinal function after transient ischemia. J Pharmacol Exp Ther. 2001; 296:216–223.
15. Klein BE, Klein R, Knudtson MD. Intraocular pressure and systemic blood pressure: longitudinal perspective: the Beaver Dam Eye Study. Br J Ophthalmol. 2005; 89:284–287.
16. Mitchell P, Lee AJ, Rochtchina E, Wang JJ. Open-angle glaucoma and systemic hypertension: the blue mountains eye study. J Glaucoma. 2004; 13:319–326.
17. Xu L, Wang H, Wang Y, Jonas JB. Intraocular pressure correlated with arterial blood pressure: the beijing eye study. Am J Ophthalmol. 2007; 144:461–462.
18. Gherghel D, Hosking SL, Orgül S. Autonomic nervous system, circadian rhythms, and primary open-angle glaucoma. Surv Ophthalmol. 2004; 49:491–508.
19. Czarnik T, Gawda R, Kolodziej W, Latka D, Sznajd-Weron K, Weron R. Associations between intracranial pressure, intraocular pressure and mean arterial pressure in patients with traumatic and non-traumatic brain injuries. Injury. 2009; 40:33–39.
20. Ding C, Wang P, Tian N. Effect of general anesthetics on IOP in elevated IOP mouse model. Exp Eye Res. 2011; 92:512–520.
21. Benumof JL, Mazzei W, Roth S, Barach P, Lam AM, Lee LA. Multifactorial etiology of postoperative vision loss. Anesthesiology. 2002; 96:1531–1532.
22. Stambough JL, Dolan D, Werner R, Godfrey E. Ophthalmologic complications associated with prone positioning in spine surgery. J Am Acad Orthop Surg. 2007; 15:156–165.
23. Cheng MA, Todorov A, Tempelhoff R, McHugh T, Crowder CM, Lauryssen C. The effect of prone positioning on intraocular pressure in anesthetized patients. Anesthesiology. 2001; 95:1351–1355.
24. Beneyto P, Barajas MA, Garcia-de-Blas F, Del Cura I, Sanz T, Vello R, Salvador C. Predictive value of tonometry with Tono-pen XL in primary care. Br J Gen Pract. 2007; 57:653–654.
25. Setogawa A. Kawai. Measurement of intraocular pressure by both invasive and noninvasive techniques in rabbits exposed to head-down tilt. Jpn J Physiol. 1998; 48:25–31.
26. Pinkney TD, King AJ, Walter C, Wilson TR, Maxwell-Armstrong C, Acheson AG. Raised intraocular pressure (IOP) and perioperative visual loss in laparoscopic colorectal surgery: a catastrophe waiting to happen? A systematic review of evidence from other surgical specialities. Tech Coloproctol. 2012; 16:331–335.
27. Nickels TJ, Manlapaz MR, Farag E. Perioperative visual loss after spine surgery. World J Orthop. 2014; 5:100–106.
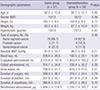
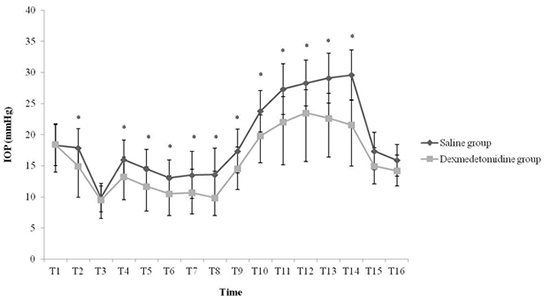
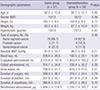
28. Kim NY, Yoo YC, Park H, Choi YD, Kim CY, Bai SJ. The effect of dexmedetomidine on intraocular pressure increase in patients during robot-assisted laparoscopic radical prostatectomy in the steep trendelenburg position. J Endourol. 2015; 29:310–316.