1. von Ruesten A, Steffen A, Floegel A. Trend in obesity prevalence in European adult cohort populations during follow-up since 1996 and their predictions to 2015. PLoS One. 2011; 6:e27455.
2. World Health Organization. Obesity and Overweight. Geneva: World Health Organization;2015.
3. Kopelman PG. Obesity as a medical problem. Nature. 2000; 404:635–643.
4. Scott KM, Bruffaerts R, Simon GE, Alonso J, Angermeyer M, de Girolamo G, Demyttenaere K, Gasquet I, Haro JM, Karam E, et al. Obesity and mental disorders in the general population: results from the world mental health surveys. Int J Obes. 2008; 32:192–200.
5. Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010; 67:220–229.
6. Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, Kessler RC. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006; 63:824–830.
7. Ohayon MM, Hong SC. Prevalence of major depressive disorder in the general population of South Korea. J Psychiatr Res. 2006; 40:30–36.
8. Palinkas LA, Wingard DL, Barrett-Connor E. Depressive symptoms in overweight and obese older adults: a test of the “jolly fat” hypothesis. J Psychosom Res. 1996; 40:59–66.
9. Li ZB, Ho SY, Chan WM, Ho KS, Li MP, Leung GM, Lam TH. Obesity and depressive symptoms in Chinese elderly. Int J Geriatr Psychiatry. 2004; 19:68–74.
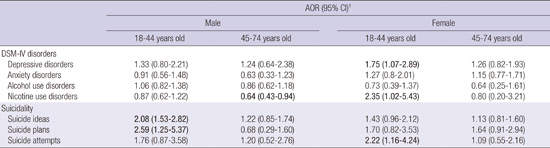
10. Sunwoo YK, Bae JN, Hahm BJ, Lee DW, Park JI, Cho SJ, Lee JY, Kim JY, Chang SM, Jeon HJ, et al. Relationships of mental disorders and weight status in the Korean adult population. J Korean Med Sci. 2011; 26:108–115.
11. Kuriyama S, Koizumi Y, Matsuda-Ohmori K, Seki T, Shimazu T, Hozawa A, Awata S, Tsuji I. Obesity and depressive symptoms in elderly Japanese: the Tsurugaya Project. J Psychosom Res. 2006; 60:229–235.
12. Kim E, Song JH, Hwang JY, Ahn K, Kim J, Koh YH, Park MH, Jo SA. Obesity and depressive symptoms in elderly Koreans: evidence for the “jolly fat” hypothesis from the Ansan Geriatric (AGE) Study. Arch Gerontol Geriatr. 2010; 51:231–234.
13. Puhl RM, Brownell KD. Psychosocial origins of obesity stigma: toward changing a powerful and pervasive bias. Obes Rev. 2003; 4:213–227.
14. Chen EY, Brown M. Obesity stigma in sexual relationships. Obes Res. 2005; 13:1393–1397.
15. Juan W, Xiao-Juan D, Jia-Ji W, Xin-Wang W, Liang X. The associations between health risk behaviors and suicidal ideation and attempts in an urban Chinese sample of adolescents. J Affect Disord. 2010; 126:180–187.
16. Noh JW, Kwon YD, Park J, Kim J. Body mass index and depressive symptoms in middle aged and older adults. BMC Public Health. 2015; 15:310.
17. Cho MJ, Seong SJ, Park JE, Chung IW, Lee YM, Bae A, Ahn JH, Lee DW, Bae JN, Cho SJ, et al. Prevalence and correlates of dsm-iv mental disorders in South Korean adults: the Korean epidemiologic catchment area study 2011. Psychiatry Investig. 2015; 12:164–170.
18. Cho MJ, Hahm BJ, Suh DW, Hong JP, Bae JN, Kim JK, Lee DW, Cho SJ. Development of a Korean version of the composite international diagnostic interview (K-CIDI). J Korean Neuropsychiatr Assoc. 2002; 41:123–137.
19. Hahm BJ. Development of a Korean version of the composite international diagnostic interview (K-CIDI) and assessment of its applicability to a Korean population [dissertation]. Seoul: Seoul National University;2001.
20. Bertolote JM, Fleischmann A, De Leo D, Bolhari J, Botega N, De Silva D, Tran Thi Thanh H, Phillips M, Schlebusch L, Värnik A, et al. Suicide attempts, plans, and ideation in culturally diverse sites: the WHO SUPRE-MISS community survey. Psychol Med. 2005; 35:1457–1465.
21. World Health Organization. Physical Status: the Use of and Interpretation of Anthropometry. Report of a WHO Expert Committee. Geneva: World Health Organization;1995.
22. Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am J Public Health. 2000; 90:251–257.
23. Onyike CU, Crum RM, Lee HB, Lyketsos CG, Eaton WW. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2003; 158:1139–1147.
24. Azarbad L, Gonder-Frederick L. Obesity in women. Psychiatr Clin North Am. 2010; 33:423–440.
25. Pearce MJ, Boergers J, Prinstein MJ. Adolescent obesity, overt and relational peer victimization, and romantic relationships. Obes Res. 2002; 10:386–393.
26. Hällström T, Noppa H. Obesity in women in relation to mental illness, social factors and personality traits. J Psychosom Res. 1981; 25:75–82.
27. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363:157–163.
28. World Health Organization Western Pacific Region. International Association for the Study of Obesity. International Obesity Task Force. The Asia?Pacific Perspective: Redefining Obesity and Its Treatment. Sydney: Health Communications Australia Pty Ltd.;2000.
29. John U, Meyer C, Rumpf HJ, Hapke U. Relationships of psychiatric disorders with overweight and obesity in an adult general population. Obes Res. 2005; 13:101–109.
30. Dare S, Mackay DF, Pell JP. Relationship between smoking and obesity: a cross-sectional study of 499,504 middle-aged adults in the UK general population. PLoS One. 2015; 10:e0123579.
31. Grunberg NE, Bowen DJ, Morse DE. Effects of nicotine on body weight and food consumption in rats. Psychopharmacology (Berl). 1984; 83:93–98.
32. Filozof C, Fernández Pinilla MC, Fernández-Cruz A. Smoking cessation and weight gain. Obes Rev. 2004; 5:95–103.
33. Linde JA, Jeffery RW, Levy RL, Sherwood NE, Utter J, Pronk NP, Boyle RG. Binge eating disorder, weight control self-efficacy, and depression in overweight men and women. Int J Obes Relat Metab Disord. 2004; 28:418–425.
34. Fulkerson JA, French SA. Cigarette smoking for weight loss or control among adolescents: gender and racial/ethnic differences. J Adolesc Health. 2003; 32:306–313.
35. Organisation for Economic Co-operation and Development. Health at a Glance 2015: OECD Indicators. Paris: OECD Publishing;2015.
36. Morris S. The impact of obesity on employment. Labour Econ. 2007; 14:413–433.
37. Chang SS, Stuckler D, Yip P, Gunnell D. Impact of 2008 global economic crisis on suicide: time trend study in 54 countries. BMJ. 2013; 347:f5239.
38. Lee J. There Are a Lot More Jobless South Koreans than You Think. New York, NY: Bloomberg Business;2015.
39. Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988-1994. J Am Diet Assoc. 2001; 101:28–34.
40. Niedhammer I, Bugel I, Bonenfant S, Goldberg M, Leclerc A. Validity of self-reported weight and height in the French GAZEL cohort. Int J Obes Relat Metab Disord. 2000; 24:1111–1118.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download