1. Waldemar AC. The high-risk infant. In : Kliegman RM, Stanton BF, St. Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 19th ed. Philadelphia: Elsevier Saunders;2011. p. 552–564.
2. Waldemar AC. Nervous system disorders. In : Kliegman RM, Stanton BF, St. Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 19th ed. Philadelphia: Elsevier Saunders;2011. p. 565–574.
3. Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJ. Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. JAMA. 2002; 288:728–737.
4. Lindsay NM, Healy GN, Colditz PB, Lingwood BE. Use of the Ages and Stages Questionnaire to predict outcome after hypoxic-ischaemic encephalopathy in the neonate. J Paediatr Child Health. 2008; 44:590–595.
5. Park HW, Yoon HK, Han SB, Lee BS, Sung IY, Kim KS, Kim EA. Brain MRI measurements at a term-equivalent age and their relationship to neurodevelopmental outcomes. AJNR Am J Neuroradiol. 2014; 35:599–603.
6. Eikenes L, Løhaugen GC, Brubakk AM, Skranes J, Håberg AK. Young adults born preterm with very low birth weight demonstrate widespread white matter alterations on brain DTI. Neuroimage. 2011; 54:1774–1785.
7. Spittle AJ, Orton J, Doyle LW, Boyd R. Early developmental intervention programs post hospital discharge to prevent motor and cognitive impairments in preterm infants. Cochrane Database Syst Rev. 2007; CD005495.
8. Bayley N. Bayley scales of infant and toddler development. 2nd ed. San Antonio (TX): The Psychological Corporation;1993.
9. Moore T, Johnson S, Haider S, Hennessy E, Marlow N. Relationship between test scores using the second and third editions of the Bayley scales in extremely preterm children. J Pediatr. 2012; 160:553–558.
10. Vohr BR, Stephens BE, Higgins RD, Bann CM, Hintz SR, Das A, Newman JE, Peralta-Carcelen M, Yolton K, Dusick AM, et al. Are outcomes of extremely preterm infants improving? Impact of Bayley assessment on outcomes. J Pediatr. 2012; 161:222–228.e3.
11. Bricker D, Squires J, Mounts L. Ages and Stages Questionnaire: a parent-completed, child monitoring system. Baltimore (MD): Paul H. Brookes;1995. p. 156.
12. Bricker D, Squires J, Mounts L, Potter LW, Nickel R, Twombly E, Farrell J. Seoul Community Rehabilitation Center. Ages and stages questionnaires: a parent-completed, child-monitoring system. 1st Engl. ed. Seoul: Seoul Community Rehabilitation Center;2000.
13. Heo KH, Squires J, Lee SY, Lee JS. Korean ages and stages questionnaires/a parent completed development screening tool. Seoul: Seoul community rehabilitation center;2006.
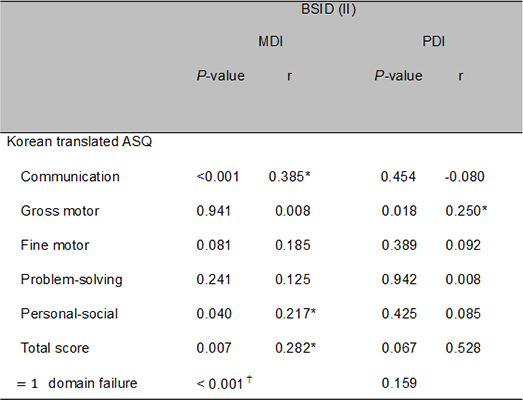
14. Kim YJ, Lee JY, Sohn JA, Lee EH, Lee JA, Choi CW, Kim EK, Kim HS, Kim BI, Choi JH. A validity study of the Korean Ages and stages questionnaires: screening for developmental delay in preterm infant. J Korean Soc Neonatol. 2010; 17:217–223.
15. Kim EY, Sung IK. The Ages and stages questionnaire: screening for developmental delay in the setting of a pediatric outpatient clinic. Korean J Pediatr. 2007; 50:1061–1066.
16. Kim MS, Kim JK. Assessment of children with developmental delay: Korean-ages & stages questionnaires (K-ASQ) and Bayley scales of infant development test II(BSID-II). J Korean Child Neurol Soc. 2010; 18:49–57.
17. Council on Children with Disabilities. Section on Developmental Behavioral Pediatrics. Bright Futures Steering Committee. Medical Home Initiatives for Children with Special Needs Project Advisory Committee. Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics. 2006; 118:405–420.
18. International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005; 123:991–999.
19. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978; 92:529–534.
20. Doyle LW. Victorian Infant Collaborative Study Group. Evaluation of neonatal intensive care for extremely low birth weight infants in Victoria over two decades: I. Effectiveness. Pediatrics. 2004; 113:505–509.
21. Doyle LW. Victorian Infant Collaborative Study Group. Evaluation of neonatal intensive care for extremely low birth weight infants in Victoria over two decades: II. Efficiency. Pediatrics. 2004; 113:510–514.
22. Vohr BR, Msall ME. Neuropsychological and functional outcomes of very low birth weight infants. Semin Perinatol. 1997; 21:202–220.
23. Aarnoudse-Moens CS, Weisglas-Kuperus N, van Goudoever JB, Oosterlaan J. Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics. 2009; 124:717–728.
24. Stephens BE, Liu J, Lester B, Lagasse L, Shankaran S, Bada H, Bauer C, Das A, Higgins R. Neurobehavioral assessment predicts motor outcome in preterm infants. J Pediatr. 2010; 156:366–371.
25. Bricker D, Squires J. Ages and stages questionnaires (ASQ): a parent completed child monitoring system. 2nd ed. Baltimore (MD): Paul H Brookes;1999. p. 157.
26. Azzopardi DV, Strohm B, Edwards AD, Dyet L, Halliday HL, Juszczak E, Kapellou O, Levene M, Marlow N, Porter E, et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N Engl J Med. 2009; 361:1349–1358.
27. Bae YH. A preliminary study for standardization of the Korean Bayley scales of infant development-II. Ulsan: University of Ulsan;2001. 12–47. Dissertation.
28. Park HW, Cho BH, Choe HJ. The standardization of Korean Bayley scales of infant development (K-BSID-II): a pilot study. Korean J Dev Psychol. 2003; 16:121–134.
29. Park HW, Kwak KJ, Park KB. The development of Korean version of Wechsler preschool and primary scale of intelligence (WPPSI): the standardization study (1). Korean J Dev Psychol. 1996; 9:60–70.
30. Johnson A. Disability and perinatal care. Pediatrics. 1995; 95:272–274.
31. Squires J, Bricker D, Potter L. Revision of a parent-completed development screening tool: ages and stages questionnaires. J Pediatr Psychol. 1997; 22:313–328.
34. Ga HY, Kwon JY. A comparison of the Korean-ages and stages questionnaires and Denver developmental delay screening test. Ann Rehabil Med. 2011; 35:369–374.
35. Simard MN, Luu TM, Gosselin J. Concurrent validity of ages and stages questionnaires in preterm infants. Pediatrics. 2012; 130:e108–e114.
36. Glascoe FP. Screening for developmental and behavioral problems. Ment Retard Dev Disabil Res Rev. 2005; 11:173–179.
37. Heo KH, Squires J, Yovanoff P. Cross-cultural adaptation of a pre-school screening instrument: comparison of Korean and US populations. J Intellect Disabil Res. 2008; 52:195–206.
39. Skellern CY, Rogers Y, O'Callaghan MJ. A parent-completed developmental questionnaire: follow up of ex-premature infants. J Paediatr Child Health. 2001; 37:125–129.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download