1. Klein JO. Otitis media. Clin Infect Dis. 1994; 19:823–833.
2. Roberts JE, Rosenfeld RM, Zeisel SA. Otitis media and speech and language: a meta-analysis of prospective studies. Pediatrics. 2004; 113:e238–e248.
3. Nittrouer S, Burton LT. The role of early language experience in the development of speech perception and phonological processing abilities: evidence from 5-year-olds with histories of otitis media with effusion and low socioeconomic status. J Commun Disord. 2005; 38:29–63.
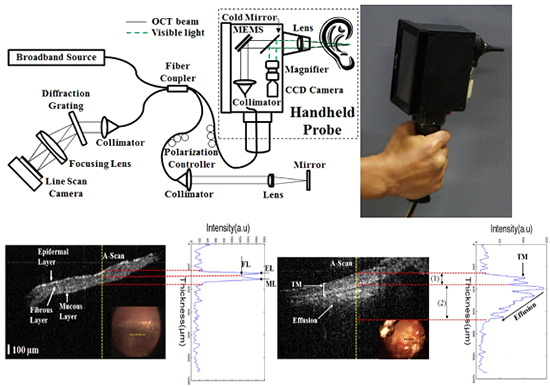
4. Nguyen CT, Jung W, Kim J, Chaney EJ, Novak M, Stewart CN, Boppart SA. Noninvasive in vivo optical detection of biofilm in the human middle ear. Proc Natl Acad Sci U S A. 2012; 109:9529–9534.
5. Nguyen CT, Tu H, Chaney EJ, Stewart CN, Boppart SA. Non-invasive optical interferometry for the assessment of biofilm growth in the middle ear. Biomed Opt Express. 2010; 1:1104–1116.
6. Jung W, Kim J, Jeon M, Chaney EJ, Stewart CN, Boppart SA. Handheld optical coherence tomography scanner for primary care diagnostics. IEEE Trans Biomed Eng. 2011; 58:741–744.
7. Huang D, Swanson EA, Lin CP, Schuman JS, Stinson WG, Chang W, Hee MR, Flotte T, Gregory K, Puliafito CA, et al. Optical coherence tomography. Science. 1991; 254:1178–1181.
8. Bouma BE, Tearney GJ. Handbook of optical coherence tomography. New York: Marcel Dekker;2002.
9. Boppart SA. Optical coherence tomography - Principles applications and advances. Minerva Biotecnologica. 2004; 16:211–237.
10. Tao YK, Zhao M, Izatt JA. High-speed complex conjugate resolved retinal spectral domain optical coherence tomography using sinusoidal phase modulation. Opt Lett. 2007; 32:2918–2920.
11. Kim J, Sohn BS. Real-time retinal imaging with a parallel optical coherence tomography using a CMOS smart array detector. J Korean Phys Soc. 2007; 51:1787–1791.
12. Wong BJ, Jackson RP, Guo S, Ridgway JM, Mahmood U, Su J, Shibuya TY, Crumley RL, Gu M, Armstrong WB, et al. In vivo optical coherence tomography of the human larynx: normative and benign pathology in 82 patients. Laryngoscope. 2005; 115:1904–1911.
13. Djalilian HR, Ridgway J, Tam M, Sepehr A, Chen Z, Wong BJ. Imaging the human tympanic membrane using optical coherence tomography in vivo. Otol Neurotol. 2008; 29:1091–1094.
14. Djalilian HR, Rubinstein M, Wu EC, Naemi K, Zardouz S, Karimi K, Wong BJ. Optical coherence tomography of cholesteatoma. Otol Neurotol. 2010; 31:932–935.
15. Wong BJ, Zhao Y, Yamaguchi M, Nassif N, Chen Z, De Boer JF. Imaging the internal structure of the rat cochlea using optical coherence tomography at 0.827 µm and 1.3 µm. Otolaryngol Head Neck Surg. 2004; 130:334–338.
16. Wong BJ, de Boer JF, Park BH, Chen Z, Nelson JS. Optical coherence tomography of the rat cochlea. J Biomed Opt. 2000; 5:367–370.
17. Choudhury N, Song G, Chen F, Matthews S, Tschinkel T, Zheng J, Jacques SL, Nuttall AL. Low coherence interferometry of the cochlear partition. Hear Res. 2006; 220:1–9.
18. Pau HW, Lankenau E, Just T, Behrend D, Hüttmann G. Optical coherence tomography as an orientation guide in cochlear implant surgery? Acta Otolaryngol. 2007; 127:907–913.
19. Gao SS, Xia A, Yuan T, Raphael PD, Shelton RL, Applegate BE, Oghalai JS. Quantitative imaging of cochlear soft tissues in wild-type and hearing-impaired transgenic mice by spectral domain optical coherence tomography. Opt Express. 2011; 19:15415–15428.
20. Cho NH, Jang JH, Jung W, Kim J. In vivo imaging of middle-ear and inner-ear microstructures of a mouse guided by SD-OCT combined with a surgical microscope. Opt Express. 2014; 22:8985–8995.
21. Cho NH, Jung U, Kwon HI, Jeong H, Kim J. Development of SD-OCT for imaging the in vivo human tympanic membrane. J Opt Soc Korea. 2011; 15:74–77.
22. Gao SS, Raphael PD, Wang R, Park J, Xia A, Applegate BE, Oghalai JS. In vivo vibrometry inside the apex of the mouse cochlea using spectral domain optical coherence tomography. Biomed Opt Express. 2013; 4:230–240.
23. Chang EW, Cheng JT, Röösli C, Kobler JB, Rosowski JJ, Yun SH. Simultaneous 3D imaging of sound-induced motions of the tympanic membrane and middle ear ossicles. Hear Res. 2013; 304:49–56.
24. Jeon M, Kim J, Jung U, Lee C, Jung W, Boppart SA. Full-range k-domain linearization in spectral-domain optical coherence tomography. Appl Opt. 2011; 50:1158–1163.
25. Lim DJ. Structure and function of the tympanic membrane: a review. Acta Otorhinolaryngol Belg. 1995; 49:101–115.
26. Pitris C, Saunders KT, Fujimoto JG, Brezinski ME. High-resolution imaging of the middle ear with optical coherence tomography: a feasibility study. Arch Otolaryngol Head Neck Surg. 2001; 127:637–642.
27. Heermann R, Hauger C, Issing PR, Lenarz T. Application of Optical Coherence Tomography (OCT) in middle ear surgery. Laryngorhinootologie. 2002; 81:400–405.










 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download