MATERIALS AND METHODS
In July 2009, the KSA Legislation Committee database was constructed to evaluate adverse anesthetic outcomes obtained from the case files of expert consultation referrals to the KSA. A detailed description of the data collection process has been reported previously (
3,
4). Briefly, each member of the KSA Legislation Committee reviewed a referred case file (typically, medical records, testimony records of involved personnel, and/or autopsy reports, if performed). Then, the reviewer completed a standardized data collection form plus a narrative summary for each case in which the sequence of events and nature of injury could be determined, together with an expert consultation service.
Since the first entry of a case file into the database in July 2009, 182 cases had been collected as of June 2014. Of them, simple academic consultation cases with inadequate detail and non-anesthetic cases, including those arising in pain clinics, were excluded. Although 128 cases were eligible for analysis, 23 cases were then excluded because of repeated consultation requests in the same case. Finally, in total, 105 cases were included in the analysis.
In each case, the standardized data set included information about patient characteristics, types of surgical procedure and hospital, anesthesia characteristics (type of anesthesia, anesthesia provider, drugs used, intraoperative monitoring, and intra-procedural oxygen supply), timing and sequence of damaging events, complications, and the presence of relevant medical records (pre-anesthetic evaluation record and anesthesia record).
Adverse outcomes were classified as 'damaging events' and 'complications'. A 'damaging event' refers to the primary mechanism causing the injury and a 'complication' refers to the ultimate injury itself (
2).
Damaging events were grouped into broad categories based on the physiological system or anesthesia technique implicated in the injury (
3,
4): respiratory events, cardiovascular events, nervous events, allergic or adverse drug reactions, equipment problems, hepatic events, renal events, endocrine events, thermal events, infectious events, or others. For further analyses, these 11 categories were subcategorized into more specific causative mechanisms, most of which are self-explanatory.
Complications were grouped into four categories; temporary, permanent/minor, permanent/major, and death. While severe brain damage, quadriplegia, or paraplegia with lifelong care or fatal prognosis were considered to be 'permanent/major' injuries, remaining permanent injuries were considered to be 'permanent/minor'
Finally, each reviewer made a judgment as to the standard of care and preventability of adverse outcomes, based on reasonable and prudent practice at the time of the event. The appropriateness of anesthesia care was graded on a 9-point numerical rating scale (NRS) with 1-3 for 'avoidable', 4-6 for 'possibly avoidable', and 7-9 for 'probably unavoidable'. This scale was made by the mix-up of 9-point NRS and 3-class coding system of preventability, which is known to have an acceptable inter-rater reliability (
5,
6).
Ethics statement
This study was exempted from institutional review board approval because no human subject was studied and no patient health information was reviewed directly.
RESULTS
Of 105 cases included in the final analysis, 69 (65.7%) were referred from police departments, and 34 (32.4%) from civil or criminal courts. The remaining two cases were referred directly from members of the KSA.
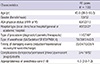
Table 1 presents an overview of all cases that have been referred during the 5-yr study period. Most patients were under the age of 60 yr (87/105, 82.9%) and were classified as ASA physical status I or II (95/105, 90.5%). Although cases related to general anesthesia were the most common, sedation cases were similarly prevalent, accounting for 37.1% of all cases.
In 82 cases (78.1% of all cases), death resulted. Of 16 cases with permanent/major injuries, 13 resulted in severe hypoxic brain damage, two became paraplegic after spinal or epidural anesthesia, and one developed hemiplegia after general anesthesia due to a cerebral hemorrhage (
Table 1,
2). Of 4 cases with permanent/minor injuries, one resulted in urinary dysfunction after epidural anesthesia, another disclosed femoral nerve injury after general anesthesia, and two others disclosed incomplete brachial plexus injury after axillary block. Temporary injuries (n=3) consisted of a sexual harassment during propofol plus ketamine sedation, a recovered case of disseminated intravascular coagulation after liposuction under propofol sedation, and a minor traffic accident after propofol sedation due to hypoglycemia.
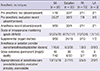
The appropriateness of anesthesia care, graded using a 9-point NRS, was not high in a considerable number of cases (
Table 1). Indeed, in 45 cases (42.9%), the resulting injuries were determined to be 'avoidable' if an appropriate standard of care had been used (
Table 2). In-depth analysis found that the proportion of 'avoidable' injuries was much higher in patient with ASA physical status I or II than in those with ASA physical status III or VI (45.3% [43/95] vs. 20.0% [2/10]).
Analysis of cases according to anesthetic technique revealed that, with the exception of 4 cases, both general anesthesia and sedation cases resulted in grave complications (i.e., permanent/major injuries or death). However, in contrast to the general anesthesia cases, most sedation cases (27/39, 69.2%) showed deviations from the appropriate standard of care (i.e., were determined to be 'avoidable'). In sedation cases, no pre-procedural testing was performed at all in 32 of 39 patients (82.1%). Pre-anesthetic evaluation records and anesthesia records were absent in 92.3% and 89.7% of the sedation cases, respectively. A significant lack of vigilance during procedures was found in the sedation cases; six patients had virtually no monitoring, and 24 patients did not receive supplemental oxygen (
Table 2). Most sedation (36/39, 92.3%) was provided simultaneously by the non-anesthesiologist(s) who performed the surgical/diagnostic procedure(s). Propofol-based regimens were used in the vast majority of sedation cases (35/39, 89.7%); propofol was used alone (n=20) or in combination with midazolam, ketamine, or remifentanil (n=15;
Fig. 1).
There were two cases relating to nurse anesthesia (
Table 2). Specifically, one patient who underwent epidural anesthesia disclosed cauda equina syndrome and had a persistent voiding difficulty despite surgical intervention. The other patient became paraplegic after cesarean section under general anesthesia, in which the causative mechanism was uncertain (injury due to incorrect patient position vs. surgical injury).
Table 3 presents the damaging events in cases with permanent (minor or major) injuries and death. Of these, a 'respiratory events' was the most common damaging event. Respiratory events resulted in 46 of the deaths (56.1% of all deaths). The three most common forms of respiratory events were hypoxia secondary to airway obstruction or respiratory depression (n=31), difficult intubation (n=8), and aspiration (n=5).
The sec common damaging event was a 'cardiovascular events', which accounted for 29.3% of all deaths. In the subgroup 'cardiovascular damaging events', almost half the cases (12/26, 46.2%) were due to acute myocardial infarction, all of which resulted in death.
Analysis of all cases according to physician specialty revealed that orthopedics (24 cases, 22.9%) was the most common department, and plastic surgery (18 cases, 17.1%) and general surgery (18 cases, 17.1%) were the next two (
Fig. 2).
DISCUSSION
Expert consultation, as analyzed in this study, is quite different from medical expert witnesses or testimony in that the former should not be coerced into participation of conclusions. Consultation only involves answering questions raised by referrals through a review of the information pertaining to the medical dispute. On receiving each expert consultation referral, the KSA Legislation Committee has clarified that the consultants cannot become involved in the legal interpretation of medical malpractice, and the case file will be used for academic purposes after protecting patient confidentiality.
The magnitude of injuries in our database appeared to be considerably high than those of the ASA-CCP database; 90.5% of the cases were for injuries resulting in death (n=82) or severe brain damage (n=13) in the KSA database vs. 39.0% in the ASA-CCP database (
2). The reasons for this may result from variations in medical and legal practice. It is evident that the medico-legal burden of procedures in medicine has been increasing steadily in Korea (
7).
Worse outcomes did not correlate with preoperative physical status, patient age, or the invasiveness of the procedures. In the present study, the majority of cases involved patients under the age of 60 yr (82.9%), those with ASA physical status I or II (90.5%), and minor surgeries or diagnostic procedures such as gastroscopy (75 cases, 71.4%). Because the inherent risk of such cases is essentially low, these findings primarily reflect increased dissatisfaction of patients or their relatives about adverse outcomes (occurrence of adverse outcomes despite a previously healthy condition or the 'simple' surgical procedure(s) performed). Additionally, it may be, in part, attributable to our findings that adherence to the standard of care is deliberately ignored in 'simple' surgical procedures in apparently healthy patients.
Hypoxia secondary to airway obstruction or respiratory depression was a leading causative mechanism. In common with our first report (
3), the present analysis identified 'respiratory events' as the leading damaging event (53.3% of all cases), all of which resulted in permanent/major injuries or death. Specifically, the largest subclass of respiratory events was hypoxia secondary to airway obstruction ('can't breathe' situation) or respiratory depression ('won't breathe' situation). Most of these cases occurred during non-anesthesiologist administered sedation (n=24). Of these cases, propofol was used alone or in combination with other sedatives, except in three cases.
Such a prevalence of non-anesthesiologist-administered sedation cases may lead to the high proportion of plastic surgical cases in our case files, which is obviously different from the previous report of Kwon (
8). In that study, plastic surgical cases accounted for 3.6% of all surgical anesthesia dispute cases, although the evaluation period (November 1994-October 2002) was different from this study. Such a difference may be primarily due to a combination of an increase in the number of the denominator (overall plastic surgical cases) and the climate of an undervalued risk of sedation in local clinics or hospitals.
Although target levels of sedation have been defined, the actual level of sedation in individual patients may easily fluctuate. In particular, at similar depths of sedation, propofol is more likely than midazolam to cause airway obstruction or respiration depression (
9). In this regard, the KSA, similar to ASA (
10) and the European Society of Anesthesiologists (
9), has supported the Food and Drug Administration regulation that propofol is restricted solely to personnel trained in general anesthesia. However, other societies of endoscopists (
11), plastic surgeons (
12), and emergency medicine doctors (
13) have proposed that non-anesthesiologists are capable of administering propofol after the completion of specialized training. Although the use of anesthesia personnel to deliver sedation for average-risk patients remains controversial, all published practice guidelines, regardless of clinical specialty, commonly recommend that sedation must be performed by an independent trained medical person not involved in the procedure (
9,
10,
11,
12,
13). However, our results showed that in 92.3% of sedation cases (36/39), sedation was provided simultaneously by non-anesthesiologist(s) who performed the surgical/diagnostic procedure(s). Thus, from a medico-legal perspective, adherence to this single item of the guidelines alone (i.e., sedation by an independent trained medical person including a qualified nurse) can help clinicians avoid many medico-legal pitfalls.
The sec largest subclass of respiratory events was difficult tracheal intubation (14.3% of all respiratory events). Of these, there were two cases of an anticipated difficult airway (cervical fracture and ankylosing spondylitis with morbid obesity), in which the first strategy was persistent attempts at laryngoscopic intubation without any preparation for a difficult airway. None of the difficult intubation cases reflected the use of a supraglottic airway such as a laryngeal mask airway for providing rescue ventilation in difficult airway management (
14). In five cases, an emergency tracheostomy was finally attempted, but was unsuccessful, thereby resulting in death. In cases of difficult airway, repeated attempts at laryngoscopic intubation can lead to a 'cannot intubate and cannot ventilate' situation, as well as airway and hemodynamic complications (
15). Thus, familiarity with difficult airway practice guideline (
14) and the skills required to anticipate and manage a difficult airway are essential for every clinician who performs anesthesia or sedation. One closed claims study (
16) found that after publication of the guidelines, difficult airway claims associated with death or brain damage during induction decreased from 62% to 35%.
Aspiration was considered the primary damaging event in five cases, of which three cases did not follow the standard preoperative fasting time. During the last decade, policy and practice regarding 'nothing by mouth' (NPO) status before elective surgery have been relaxed, especially with regard to clear fluids. However, it is notable that the latest ASA guidelines (
17) maintain a NPO time of more than 6-8 hr for solids before elective surgery, and this has been accepted rigidly in our courts.
During the perioperative period of major non-cardiac surgery, the incidence of myocardial infarction has been reported to be 1%-3% (
18). In the present analysis, acute myocardial infarction was the most common cardiovascular event (12 cases, 44.4% of cardiovascular events), all of which resulted in death. Of them, nine patients showed a new onset of acute myocardial infarction during or after the surgical procedures.
The symptoms of myocardial ischemia are rare or often silent, making the detection of inducible myocardial ischemia, very difficult. However, in-depth analysis of our cases revealed disproportionate gender (male dominance: 8 men, 4 women) and age (median: 50.0 yr; interquartile range: 39.0-58.0 yr) distributions. Thus, in male patients aged ≥40 yr, more attention may be necessary to identify atherosclerotic risk factors in preoperative history taking and the physical examination, as recommended in the latest American College of Cardiology/American Heart Association guidelines for perioperative cardiovascular evaluations (
19). Korean National Health Insurance claim data also indicated that males and patients aged ≥45 yr represented 69.9% and 93.0% of newly hospitalized patients with acute myocardial infarction in 2010, respectively (
20). Because myocardial infarction can be brought on by ischemic imbalance other than coronary artery disease alone, the risk for myocardial infarction can be further reduced by avoiding myocardial supply/demand mismatch conditions (e.g., inadequate pain control, hypoxemia, anemia, or severe hemodynamic alterations).
Our analysis identified two cases of nurse anesthesia. Unlike the Certified Registered Nurse Anesthetists (CRNAs) system in the United States (
21), nurse anesthesia is legally prohibited in Korea. Of course, the nurses can assist clinicians' anesthetic practice in the limited area, which is legally deemed the nursing practice. Although the Korean government has still maintained nurse-anesthetists since 1973, recent precedent of the Supreme Court clearly stated that even nurse-anesthetist cannot perform anesthetic practice licensed to the doctors, and it is also a violation of medical law, even performed in the direction of the supervised doctor.
Several noticeable findings in the cases were involved with anesthesiologists. In contrast to the cases related to non-anesthesiologists, most cases involved with anesthesiologists (49/61, 80.3%) was associated with general anesthesia. In 27 cases, adverse events occurred in the postanesthesia care unit or ward. Legally, the responsibility for anesthesia providers holds until the regaining of consciousness in normal patients, not simply the restoration of normal respiration. Especially, it is notable that in 3 cases, adverse respiratory events developed after anesthesiologists had left the hospital in office-based anesthesia setting.
Though the cases involved with anesthesiologists had a similar incidence of death to those related to non-anesthesiologists (78.7% vs. 81.0%), both groups showed a different distribution of damaging events: increased prevalence of cardiovascular events in the cases involved with anesthesiologists (20/61 [32.8%] vs. 6/42 [14.3%]). This result may be mainly attributed the findings that anesthesiologists were involved in higher ASA patients undergoing more complex surgical procedures. However, this result highlights the importance of surveillance for cardiovascular events, especially in the anesthesia community.
Compared with the closed-claims analysis of the ASA-CCP, the KSA Legislation Committee database enables us to identify recent changes in anesthetic injury trends. Closed claims analyses are limited by a long time lag (approximately 3-6 yr in Korea) between the adverse event and the closure of the claim, when it becomes available for further study.
Nonetheless, this study has some limitations in interpretation. First, only the injury cases that were referred to the KSA can be investigated; the actual numbers and nature of all other injuries remain unknown. In the United Kingdom, only 1.5%-3% of patients who experience possibly negligent care actually file a malpractice claim (
22). This may introduce a bias towards the inclusion of cases involving more severe injuries in our database. Sec, clear cause and effect conclusions cannot be drawn from our analysis due to inherent defects such as the retrospective nature, absence of denominator data, and no use of a standardized protocol for diagnosis or management. In particular, as mentioned in a previous report (
3), some data for several cases seemed doubtful in terms of authenticity. Regarding the narrative statements from the healthcare personnel involved, they tended to lack impartiality. Lastly, some criticisms may be raised about our evaluation scale for the appropriateness of anesthesia care (i.e., three nominal classes with an individual 3-point NRS score) in that it was independently rated by different reviewers. However, the consistency with which appropriateness of care can be judged by different reviewers has been demonstrated previously (
5,
6). Actually, there are not enough authoritative guidelines currently in existence to cover the range of issues involved in medical malpractice cases. Previous study (
23) suggested that there were only enough guidelines to provide useful guidance in about 20% of malpractice cases.
In conclusion, the present analysis using the KSA database of anesthesia-related medical disputes demonstrated several 'typical' injury profiles: an apparent lack of vigilance in less invasive procedures in apparently healthy patients, hypoxia secondary to airway obstruction or respiratory depression in a poorly controlled sedation environment, a 'cannot intubate and cannot ventilate' situation as a result of non-compliance with the guidelines for difficult airway management, and high proportion and mortality of perioperative acute myocardial infarction.
In almost half of the cases, the resulting injuries were determined to be 'avoidable' if an appropriate standard of care had been followed. Therefore, patient safety and obviation of malpractice litigation can be increased by a clear understanding of these typical injury profiles and strict adherence to established practical guidelines; careful pre-procedural evaluation, adequate level of intra-procedural monitoring, and proactive responses to adverse occurrences.






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download