Abstract
Figures and Tables
Fig. 1

Fig. 2

Table 1
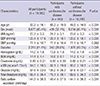
Data expression as mean±standard deviation or numbers with percentage, as appropriate. P values are those of independent t-test or chi-square test. *The amount of daily sodium excretion was estimated using the Tanaka equations based on spot urine sample. BMI, body mass index; BUN, blood urea nitrogen; DBP, diastolic blood pressure; eGFR, estimated glomerular filtration rate; SBP, systolic blood pressure.
Table 2
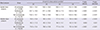
Data expression as mean±standard deviation. P values are those of ANOVA or ANCOVA adjusted for age, sex, BMI, diabetes mellitus, hemoglobin levels, eGFR, and total cholesterol levels. *The amount of urinary sodium excretion was categorized according to the quartile range (Q1-Q4) in each groups. Three cut-points dividing the quartiles are as follows: 119.3, 142.2, and 167.2 in all participants; 123.3, 149.0, and 175.1 in subjects with cardiovascular disease; 119.1, 142.0, and 166.8 in subjects without cardiovascular disease.
Table 3
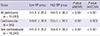
Data expression as mean±standard deviation. P values are those of ANOVA or ANCOVA adjusted for age, sex, BMI, diabetes mellitus, hemoglobin levels, eGFR, and total cholesterol levels. BP, blood pressure; cardiovascular, participants with coronary heart disease or cerebrovascular disease; high BP group, participants with systolic blood pressure at or over 140 mmHg or diastolic blood pressure at or over 90 mmHg; low BP group, participants with systolic blood pressure under 140 mmHg and diastolic blood pressure under 90 mmHg.
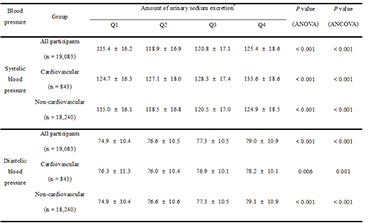
Table 4

Data expression as the odd ratio (95% confidence interval). High blood pressure was defined as either systolic blood pressure above 140 mmHg or diastolic blood pressure above 90 mmHg. Covariates in the multivariate analysis included age, sex, BMI, diabetes mellitus, hemoglobin levels, eGFR, and total cholesterol levels. *The amount of urinary sodium excretion was categorized according to the quartile range (Q1-Q4) in each group. Three cut-points dividing the quartiles are as follows: 119.3, 142.2, and 167.2 in all participants; 123.3, 149.0, and 175.1 in subjects with cardiovascular disease; 119.1, 142.0, and 166.8 in subjects without cardiovascular disease.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download