Abstract
Obesity and its related factors are known to suppress the secretion of growth hormone (GH). We aimed to evaluate the influence of body mass index (BMI) on the peak GH response to provocative testing in short children without GH deficiency. We conducted a retrospective review of medical records of 88 children (2-15 yr old) whose height was less than 3 percentile for one's age and sex, with normal results (peak GH level > 10 ng/mL) of GH provocative testing with clonidine and dopamine. Peak stimulated GH level, height, weight, pubertal status and serum IGF-1 level were measured. Univariate analysis showed that the BMI standard deviation score (SDS) correlated negatively with the natural log (ln) of the peak stimulated GH level (ln peak GH). BMI SDS did not correlate significantly with sex, age, pubertal status, or ln IGF-1 level. BMI SDS correlated negatively with ln peak GH level induced by clonidine but not by dopamine. In stepwise multivariate regression analysis, BMI SDS was the only significant predictor of ln peak GH level in the combination of tests and the clonidine test, but not in the dopamine test. In children without GH deficiency, BMI SDS correlates negatively with the peak GH level. BMI SDS should be included in the analysis of the results of GH provocation tests, especially tests with clonidine.
The standard method for the diagnosis of growth hormone deficiency (GHD) in children is to produce insufficient responses to two separate GH provocation tests. However, GH provocation tests with various pharmacological agents sometimes produce false-positive results. Some patients diagnosed with GHD in childhood have a normal GH response in adulthood (1, 2). Poor reproducibility of the GH provocation test can be caused by various factors affecting either physiological GH secretion or the stimulated GH response to pharmacological agents (3).
GH secretion increases during puberty. Spontaneous and stimulated peak GH levels are higher in pubertal children than in prepubertal children. Estrogen administration before the stimulating agent augments the GH response (4, 5), and GH secretory status just before the GH provocation test may also affect the results. The GH response to a pharmacological agent may be blunted after endogenous peak of GH level (6). Short-term and long-term nutritional status also influences the results of the GH provocation test (7).
In adults, spontaneous and stimulated peak GH levels are lower in obese people than in normal-weight people, and the degree of obesity correlates negatively with the peak GH level after pharmacological stimulations (8). Spontaneous GH secretion is suppressed in children with a high body mass index (BMI) (5). Recent studies of short children, including those with GHD, have reported that higher BMI was related to a lower peak stimulated GH level (9-11). However, it is not clear whether there is a similar association between BMI and peak GH level in short normal children without GHD. This study aimed to evaluate the influence of BMI on the peak GH response to GH provocative testing in short normal children without GHD.
Clinical data were collected retrospectively from a review of medical records of children who visited the pediatric endocrine clinic at Seoul National University Children's Hospital for short stature between January 2000 and July 2011. Of the 588 children who underwent GH stimulation testing, 308 children were diagnosed as GHD and excluded from the analysis. Seventy two children with neuro-secretory dysfunction and 2 children with IGF-1 insensitivity were also excluded. Children with chronic disease (n = 30), congenital syndrome (n = 31), hypothyroidism (n = 2), and a central nervous system abnormality (n = 20) were excluded. Subjects who had been taking medicines that might influence spontaneous and stimulated GH secretion, such as corticosteroids or antipsychotic drugs, were also excluded (n = 2). Ninety five subjects underwent two GH provocation tests with clonidine and dopamine. Twenty six subjects were tested with a different protocol such as a single test or using different kinds of pharmacologic agents. Of the 95 subjects, 7 children were excluded because their peak GH levels were considered as outliers. Finally, 88 children (2-15 yr old) were included in this study.
To assess GH secretion, clonidine (Clonidine Hydrochloride®, Mylan Pharmaceuticals, Canonsburg, PA, USA, 0.125 mg/m2) and dopamine (Sinemet®, MSD, Whitehouse Station, NJ, USA, 25 mg carbidopa/250 mg levodopa, body weight more than 30 kg, 500 mg of levodopa; 15 kg to 30 kg, 250 mg of levodopa; less than 15 kg, 125 mg of levodopa) were administered orally after overnight fasting without pretreatment with sex steroids. Blood samples were collected 0, 30, 60, 90, and 120 min later to obtain the serum GH concentration for each time point. Data for height, weight, pubertal status, and serum IGF-1 concentration and peak GH level after stimulation were collected from medical records. Pubertal status was assessed with the Tanner stage of breast development for girls and genital development for boys. Bone age was measured using the method described by Greulich and Pyle (12). BMI was calculated from height and weight. BMI and height standard deviation scores (SDS) were calculated using the 2007 Korean National Growth Charts (13).
Serum GH levels were measured using a immunoradiometric assay with an analytical sensitivity of 0.04 µg/L, intra-assay coefficient of variation (CV) of 1.9%-3.9%, and interassay CV of 2.5%-4.1% (DiaSorin Inc., Stillwater, MN, USA). Serum IGF-1 levels were measured using an immunoradiometric assay with an analytical sensitivity of 1.25 µg/L, intra-assay CV of 2.6%-4.4%, and interassay CV of 7.4%-9.1% (IDS Inc., Fountain Hills, AZ, USA).
Statistical analysis was performed using PASW Statistics 18 (SPSS Inc., Chicago, IL, USA). Natural log (ln) transformation was performed for peak GH and IGF-1 levels because these variables were not normally distributed, as determined by the Shapiro-Wilk W test. Univariate analysis was performed using Pearson correlation coefficients. Peak GH levels were compared between the clonidine and dopamine tests using a paired t test. Multivariate stepwise regression modeling was used to identify independent predictors of the peak GH response to the stimuli. Covariates entered into the model included those known or suspected to influence GH secretion such as age, sex, pubertal status, ln IGF-1, and BMI SDS. Significance was defined as P < 0.05. The results are reported as mean ± SD unless stated otherwise.
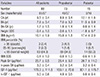
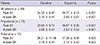
The demographic and laboratory data are summarized in Table 1. The mean age of the 88 children included in our study was 9.5 ± 3.4 yr; 51 (58%) were boys. Seventy-three children (83%) were prepubertal and 15 children (17%) were pubertal (Tanner stage 2-5). Most children (n = 83) were normal weight, three were obese, and two were overweight. The average height SDS was -2.4 ± 1.0. The mean BMI SDS was -0.8 ± 1.0, suggesting a distribution approximating that of BMI for the general population. The mean peak GH level in the two provocation tests with clonidine and dopamine (peak GH_T) was 25.7 ± 9.7 µg/L. The mean peak GH level in the test with clonidine (peak GH_C) was 24.3 ± 10.0 µg/L, which was significantly higher than the mean GH peak in the test with dopamine (peak GH_D) (16.8 ± 9.1 µg/L, P < 0.001) (Table 2).
Univariate analysis showed that BMI SDS correlated negatively with ln peak GH_T (r = -0.226, P = 0.034) and with ln peak GH_C (r=-0.25, P = 0.022), but not with ln peak GH_D (Fig. 1). Height SDS, age, sex, pubertal status (prepubertal vs pubertal), and ln IGF-1 were not significantly associated with ln peak GH_T, ln peak GH_C, or ln peak GH_D. Ln IGF-1 correlated significantly with height SDS (r = 0.38, P < 0.001) but not with BMI SDS.
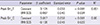
In stepwise multivariate regression analysis including age, sex, pubertal status, BMI SDS, and ln IGF-1 as independent variables and ln peak GH as the dependent variable, BMI SDS was the only significant predictor of ln peak GH_T and ln peak GH_C (Table 3).
After classifying the subjects into prepubertal and pubertal groups, the univariate associations between BMI SDS and ln peak GH_T, ln peak GH_C, and ln peak GH_D were no longer significant within either group. In stepwise multivariate regression analysis including age, sex, height SDS, BMI SDS, and ln IGF-1 as independent variables and ln peak GH as the dependent variable, BMI SDS was not significantly associated with ln peak GH_T, ln peak GH_C, or ln peak GH_D in the prepubertal or pubertal groups.
In this study, we found an inverse relationship between BMI SDS and peak GH level stimulated by clonidine. Although this relationship was not significant in dopamine test, the highest concentration of GH on two provocation tests with clonidine and dopamine was also associated negatively with BMI SDS. The mean and SD of BMI SDS of these subjects were -0.7 and 1.1, respectively, suggesting that the distribution of BMI was nearly normal. Thus, our study demonstrated a significant negative relationship between stimulated peak GH concentration and BMI in short children with normal GH response.
Secretion of GH decreases in obese people, and both spontaneous and stimulated peak GH levels are lower in obese children than in normal-weight children (14). Previous findings and our results suggest that there is an inverse relationship between stimulated peak GH level and BMI not only in obese children but also in normal-weight children. Our results are consistent with those of a previous study of adult men in which higher BMI, even when increased only minimally, was associated with a lower peak GH level after administration of arginine and/or Growth hormone releasing hormone (GHRH) (15).
GH has a lipolytic effect on adipose tissue, and GH-deficient patients generally have abundant fat tissue. The low GH level in obese people or in those with a high BMI may result from a shortened half-life of GH or decreased GH production and secretion (16). The possible causes of decreased GH production and secretion are dysregulation of the GHRH, somatostatin, and ghrelin pathways (17, 18), hyperinsulinemia (19), or increased free fatty acid (FFA) level. In obese patients, inhibition of FFA production by administration of the antilipolytic drug acipimox ameliorated the effect of obesity on GH secretion (19, 20). FFA blocks GH secretion through direct pituitary inhibition or through inhibition of GHRH release and stimulation of somatostatin (21, 22) release from the hypothalamus.
Our results are consistent with previous studies of short children that showed a negative association between BMI and stimulated peak GH level (9-11). However, these studies did not exclude the children with GHD. Analysis including GHD patients could be influenced by high BMI caused by impaired metabolic effect of GH in GHD patients. By contrast, we excluded subjects with obvious GHD to allow us to evaluate the effect of BMI per se on GH secretion tests. In our study, the reciprocal relationship between BMI SDS and ln peak GH was not significant in prepubertal children or in pubertal children. This finding is inconsistent with the results of the studies by Stanley et al. (9) and Loche et al. (10). The former showed a negative relationship in prepubertal children but not in pubertal children, and the latter showed a negative relationship in both groups. This difference may be explained by the small number of subjects and relatively weak association between BMI and peak GH level compared with previous studies because we excluded subjects with GHD.
The GH-stimulating potency varies and depends on the individual pharmacological agent used in the test. In a study of short normal children, peak GH level was higher after administration of clonidine than after insulin or arginine (23). However, another study found no significant difference in peak GH levels with various provocative agents except for GHRH (24). In our study, peak GH_C was significantly higher than peak GH_D. In previous studies, Loche et al. (10) used only clonidine, and Stanley et al. (9) and Lee et al. (11) did not analyze the effect of BMI on peak GH level with each pharmacological agent. We analyzed peak GH level for GH provocation tests with clonidine and dopamine, and for each stimulation test. Interestingly, when we analyzed the clonidine and dopamine test results separately, the negative relationship between ln peak GH and BMI SDS was significant for clonidine but not for dopamine. Clonidine is the most widely used agent in diagnostic tests of GHD in children (22). Clonidine, an α2 adrenergic agonist, increases GH secretion by stimulating GHRH neurons and inhibiting somatostatin neurons (25, 26). Dopamine stimulates both somatostatin neurons and GHRH neurons, although the overall effect of dopamine is to stimulate GH secretion (26). Dopamine receptor type 2 (D2R) exists on both GHRH and somatostatin neurons, and seems to affect these two hypothalamic hormones. GH secretion may also be stimulated directly via D2R on somatotropes (27). The different results of the clonidine and dopamine tests in our study may be explained by the different mechanisms of GH secretion stimulated by these two drugs. Further studies are needed to identify the precise mechanism underlying the stimulation of GH secretion by these agents. The relationship between BMI and peak GH stimulated by other GH-provoking agents should also be investigated.
There are some limitations to our study. First, we could not prove causality because our study was a retrospective cross-sectional study by review of medical records. Second, the number of subjects in our study was relatively small. Third, we used GH provocation tests with only two pharmacological agents, clonidine and dopamine. We cannot explain the mechanism underlying the different results for the clonidine and dopamine tests. It is unknown whether there is an inverse relationship between peak GH level and BMI in normal children after stimulation by pharmacological agents other than clonidine. In previous studies (9-11) and in our study, most of the peak GH level could be attributed to the peak GH release induced by clonidine stimulation. Further studies with larger cohorts and further analysis of individual responses to various pharmacological agents are required.
Despite these limitations we conclude that BMI affects the stimulated GH level in children whose peak GH level is above 10 ng/mL, as well as in children with GHD. The effect of BMI on peak GH level depends on the stimulating agents. These results suggest that the result of GH provocation test could be different according to the kind of pharmacologic agents and subject's BMI. Thus we should take BMI into consideration when interpreting the results of GH provocation tests, especially tests with clonidine.
Figures and Tables
Fig. 1
Univariate correlation between BMI SDS and ln peak GH_T (A), ln peak GH_C (B), and ln peak GH_D (C). Abbreviations: Ln peak GH_T, natural log of peak GH level in two tests with clonidine and dopamine; Ln peak GH_C, natural log of peak GH level in the clonidine test; Ln peak GH_D, natural log of peak GH level in the dopamine test; BMI SDS, body mass index standard deviation score.

References
1. Cacciari E, Tassoni P, Cicognani A, Pirazzoli P, Salardi S, Balsamo A, Cassio A, Zucchini S, Colli C, Tassinari D, et al. Value and limits of pharmacological and physiological tests to diagnose growth hormone (GH) deficiency and predict therapy response: first and second retesting during replacement therapy of patients defined as GH deficient. J Clin Endocrinol Metab. 1994; 79:1663–1669.
2. Maghnie M, Strigazzi C, Tinelli C, Autelli M, Cisternino M, Loche S, Severi F. Growth hormone (GH) deficiency (GHD) of childhood onset: reassessment of GH status and evaluation of the predictive criteria for permanent GHD in young adults. J Clin Endocrinol Metab. 1999; 84:1324–1328.
3. Zadik Z, Chalew SA, Gilula Z, Kowarski AA. Reproducibility of growth hormone testing procedures: a comparison between 24-hour integrated concentration and pharmacological stimulation. J Clin Endocrinol Metab. 1990; 71:1127–1130.
4. Marin G, Domené HM, Barnes KM, Blackwell BJ, Cassorla FG, Cutler GB Jr. The effects of estrogen priming and puberty on the growth hormone response to standardized treadmill exercise and arginine-insulin in normal girls and boys. J Clin Endocrinol Metab. 1994; 79:537–541.
5. Rose SR, Municchi G, Barnes KM, Kamp GA, Uriarte MM, Ross JL, Cassorla F, Cutler GB Jr. Spontaneous growth hormone secretion increases during puberty in normal girls and boys. J Clin Endocrinol Metab. 1991; 73:428–435.
6. Devesa J, Lima L, Lois N, Fraga C, Lechuga MJ, Arce V, Tresguerres JA. Reasons for the variability in growth hormone (GH) responses to GHRH challenge: the endogenous hypothalamic-somatotroph rhythm (HSR). Clin Endocrinol (Oxf). 1989; 30:367–377.
7. Maghnie M, Valtorta A, Moretta A, Larizza D, Preti P, Palladini G, Calcante S, Severi F. Diagnosing growth hormone deficiency: the value of short-term hypocaloric diet. J Clin Endocrinol Metab. 1993; 77:1372–1378.
8. Williams T, Berelowitz M, Joffe SN, Thorner MO, Rivier J, Vale W, Frohman LA. Impaired growth hormone responses to growth hormone-releasing factor in obesity: a pituitary defect reversed with weight reduction. N Engl J Med. 1984; 311:1403–1407.
9. Stanley TL, Levitsky LL, Grinspoon SK, Misra M. Effect of body mass index on peak growth hormone response to provocative testing in children with short stature. J Clin Endocrinol Metab. 2009; 94:4875–4881.
10. Loche S, Guzzetti C, Pilia S, Ibba A, Civolani P, Porcu M, Minerba L, Casini MR. Effect of body mass index on the growth hormone response to clonidine stimulation testing in children with short stature. Clin Endocrinol (Oxf). 2011; 74:726–731.
11. Lee HS, Hwang JS. Influence of body mass index on growth hormone responses to classic provocative tests in children with short stature. Neuroendocrinology. 2011; 93:259–264.
12. Greulich WW, Pyle SI. Radiologic atlas of skeletal development of the hand and wrist. 2nd ed. Standford: University Press;1959.
13. Moon JS, Lee SY, Nam CM, Choi JM, Choe BK, Seo JW, Oh K, Jang MJ, Hwang SS, Yoo MH, et al. 2007 Korean national growth charts: review of developmental process and an outlook. Korean J Pediatr. 2008; 51:1–25.
14. Loche S, Cambiaso P, Carta D, Setzu S, Imbimbo BP, Borrelli P, Pintor C, Cappa M. The growth hormone-releasing activity of hexarelin, a new synthetic hexapeptide, in short normal and obese children and in hypopituitary subjects. J Clin Endocrinol Metab. 1995; 80:674–678.
15. Bonert VS, Elashoff JD, Barnett P, Melmed S. Body mass index determines evoked growth hormone (GH) responsiveness in normal healthy male subjects: diagnostic caveat for adult GH deficiency. J Clin Endocrinol Metab. 2004; 89:3397–3401.
16. Veldhuis JD, Iranmanesh A, Ho KK, Waters MJ, Johnson ML, Lizarralde G. Dual defects in pulsatile growth hormone secretion and clearance subserve the hyposomatotropism of obesity in man. J Clin Endocrinol Metab. 1991; 72:51–59.
17. Pincelli AI, Rigamonti AE, Scacchi M, Cella SG, Cappa M, Cavagnini F, Müller EE. Somatostatin infusion withdrawal: studies in the acute and recovery phase of anorexia nervosa, and in obesity. Eur J Endocrinol. 2003; 148:237–243.
18. Volta C, Bernasconi S, Iughetti L, Ghizzoni L, Rossi M, Costa M, Cozzini A. Growth hormone response to growth hormone-releasing hormone (GHRH), insulin, clonidine and arginine after GHRH pretreatment in obese children: evidence of somatostatin increase? Eur J Endocrinol. 1995; 132:716–721.
19. Misra M, Bredella MA, Tsai P, Mendes N, Miller KK, Klibanski A. Lower growth hormone and higher cortisol are associated with greater visceral adiposity, intramyocellular lipids, and insulin resistance in overweight girls. Am J Physiol Endocrinol Metab. 2008; 295:E385–E392.
20. Scacchi M, Orsini F, Cattaneo A, Grasso A, Filippini B, Pecori Giraldi F, Fatti LM, Moro M, Cavagnini F. The diagnosis of GH deficiency in obese patients: a reappraisal with GHRH plus arginine testing after pharmacological blockade of lipolysis. Eur J Endocrinol. 2010; 163:201–206.
21. Alvarez CV, Mallo F, Burguera B, Cacicedo L, Dieguez C, Casanueva FF. Evidence for a direct pituitary inhibition by free fatty acids of in vivo growth hormone responses to growth hormone-releasing hormone in the rat. Neuroendocrinology. 1991; 53:185–189.
22. Casanueva FF, Villanueva L, Dieguez C, Diaz Y, Cabranes JA, Szoke B, Scanlon MF, Schally AV, Fernandez-Cruz A. Free fatty acids block growth hormone (GH) releasing hormone-stimulated GH secretion in man directly at the pituitary. J Clin Endocrinol Metab. 1987; 65:634–642.
23. Corneli G, Di Somma C, Baldelli R, Rovere S, Gasco V, Croce CG, Grottoli S, Maccario M, Colao A, Lombardi G, et al. The cut-off limits of the GH response to GH-releasing hormone-arginine test related to body mass index. Eur J Endocrinol. 2005; 153:257–254.
24. Ghigo E, Bellone J, Aimaretti G, Bellone S, Loche S, Cappa M, Bartolotta E, Dammacco F, Camanni F. Reliability of provocative tests to assess growth hormone secretory status: study in 472 normally growing children. J Clin Endocrinol Metab. 1996; 81:3323–3327.
25. Gil-Ad I, Laron Z, Koch Y. Effect of acute and chronic administration of clonidine on hypothalamic content of growth hormone-releasing hormone and somatostatin in the rat. J Endocrinol. 1991; 13:381–385.
26. Hanew K, Utsumi A. The role of endogenous GHRH in arginine-, insulin-, clonidine- and l-dopa-induced GH release in normal subjects. Eur J Endocrinol. 2002; 146:197–202.
27. García-Tornadu I, Risso G, Perez-Millan MI, Noain D, Diaz-Torga G, Low MJ, Rubinstein M, Becu-Villalobos D. Neurotransmitter modulation of the GHRH-GH axis. Front Horm Res. 2010; 38:59–69.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download