Abstract
Recent advances in childhood cancer treatment have increased survival rates to 80%. Two out of three survivors experience late effects (LEs). From a group of 241 survivors previously described, 193 were followed at the long-term follow-up clinic (LTFC) of Severance Hospital in Korea; the presence of LEs was confirmed by oncologists. We reported the change in LEs during 3 yr of follow-up. The median follow-up from diagnosis was 10.4 yr (5.1-26.2 yr). Among 193 survivors, the percentage of patients with at least one LE increased from 63.2% at the initial visit to 75.1% at the most recent visit (P = 0.011). The proportion of patients having multiple LEs and grade 2 or higher LEs increased from the initial visit (P = 0.001 respectively). Forty-eight non-responders to the LTFC were older and had less frequent and severe LEs than responders at initial visit (all P < 0.05). In multivariate analysis, younger age at diagnosis, older age at initial visit, a diagnosis of a brain tumor or lymphoma, and use of radiotherapy were significant risk factors for LEs (all P < 0.05). Adverse changes in LEs were seen among the survivors, regardless of most clinical risk factors. They need to receive comprehensive, long-term follow up.
Recent advances in the diagnosis, treatment, and supportive care of childhood cancers have increased the survival rate up to 80% (1). As more survivors of childhood cancers reach adulthood, chronic toxic effects from treatment-the so called "late effects (LEs)"-are also increasing in frequency (2, 3). In the United States, there are about 270,000 survivors of childhood cancers, and about one of every 640 young adults (20-39 yr of age) is a childhood cancer survivor. In general, two out of three of survivors experience at least one late effect (2).
The range of LEs is quite broad and can involve endocrine (including gonadal and growth), cardiovascular, pulmonary, and renal systems, or result in neurocognitive abnormalities (4, 5). Increasing concerns about chronic health conditions and health status, including quality of life, have prompted a call for guidelines for long-term follow-up of survivors of childhood cancers in various regions of the world, and multidisciplinary approach is being performed (6, 7).
There are many published reports on LEs and health status (i.e., general and mental health status). While most of the studies were focused on a single LE or a single disease entity, some large scale studies on overall health status were recently conducted in Western countries (2, 8-10). Due to the large number of childhood cancer survivors, many studies have used public health data or questionnaires instead of confirming LEs by physicians.
We have previously published a report on the overall health conditions of childhood cancer survivors seen at a long-term follow-up clinic (LTFC), the first one to be established in Korea (11). Here we report the follow-up data for these survivors. The purpose of this study was to determine the characteristic changes in LEs in the same cohort of survivors and to present insights for development of well-coordinated, follow-up protocols for survivors.
In January 2005, an LTFC for childhood cancer survivors was established in Severance Hospital, Yonsei University Health System (YUHS) in Seoul, Korea. A childhood cancer survivor was defined as a person who survived for at least 2 yr after completion of cancer therapy. Members of a society of childhood cancer survivors treated at Severance Hospital were invited to the LTFC. This study included 241 childhood cancer survivors who were included in our previous report on the health status of survivors. All patients were diagnosed before the age of 18 yr and were treated at Severance Hospital between 1980 and 2007. Other inclusion and exclusion criteria for survivor recruitment are described in the previous study (11). While follow-up on a regular basis was recommended for all 241 survivors, only 193 survivors were being followed at the clinic as of February 25, 2011.
Medical records were reviewed to determine treatment history and health risks for each survivor. Many published long-term follow-up guidelines for the survivors were adopted and modified by YUHS to develop a follow-up protocol, taking into consideration the expertise, effectiveness, and regional reimbursement environments of Korea (12-14). Detailed operation of our LTFC is described in the previous report (11).
In the previous study, late effects were defined as adverse events experienced by survivors at least 2 yr after completion of therapy. The severity of each LE was graded according to the Common Terminology Criteria for Adverse Events v3.0 (CTCAE).
Based on other reports, the grades were considered as continuous variables in order to compare the severity of LEs between risk groups (15, 16).
Late effects were analyzed in three ways: the number of LEs, the mean severity of LEs, and the sum of LEs grades (sum). Since LEs were classified by both individual organs and body systems, to avoid counting an LE more than once, the number of LEs represents the number of affected body systems (online supplemental Table S1). The mean severity is the arithmetic mean of the severity grades. The sum of grades of LEs takes the sum of all LE grades in each survivor and it reflects both the number and severity of LEs that each survivor has.
Health conditions were compared between 48 survivors who were lost to follow-up (non-responders) and the 193 survivors (responders) who were followed. The significance of the number, mean severity, and sum of LEs was tested by chi-square test, Student t-test, paired t-test, and one-way analysis of variance (ANOVA). A correlation analysis (Pearson's coefficient) was also conducted. Non-parametric variables were tested using the Mann-Whitney test. A multiple linear regression analysis was performed to examine the association between clinical risk factors and the number, mean severity, or sum of LEs.
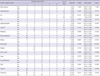
For the 193 survivors (responders), the mean sum of grades at the most recent visit was increased compared with the initial visit (2.6 ± 0.2 vs 1.7 ± 0.1, respectively, P < 0.001; Table 1). Late effects were observed in 75.1% of responders at the recent visit, which was higher than at the initial visit (63.2%, P = 0.011). Five LEs were observed in 3.6% of responders at a recent visit, compared with only one (0.5%) of all survivors at initial visit. Among responders, 53.3% had grade 2 or higher LEs, compared with 26.4% at initial visit (P = 0.001). There was one death (grade 5) among responders, due to dilated cardiomyopathy related with anthracyclines.
In the responder group, 62.2% were male, and 37.8% were female (online supplemental Table S2). The median age at diagnosis was 4.4 yr (range, 0.0-16.8 yr) for responders and 5.0 yr (range, 0.2-16.8 yr) for non-responders (P = 0.628). Age at initial visit and current age were all higher in the non-responder group compared with the responder group (all P = 0.001). The median time elapsed since completion of treatment was also higher in non-responders than in responders (P < 0.001).
In the responder group (n = 193), 36.8% (n = 71) had leukemia and 15.5% (n = 30) had lymphoma. The distribution of malignancies and treatment modalities were not significantly different between the two groups (P = 0.655 and P = 0.088, respectively). The proportion of survivors who had undergone a hematopoietic stem cell transplant (HSCT) was significantly higher in the responder group compared with the non-responder group (20.7% [40/193] vs 4.2% [2/48], P = 0.007).
The sum at the initial visit was significantly lower in non-responders than in responders (1.0 ± 0.2 vs 1.7 ± 0.1, respectively, P = 0.01, online supplemental Table S3). The percentage of survivors who presented with LEs was lower in non-responders compared with responders (45.8% vs 63.2%, respectively, P = 0.028). Twenty-one (10.9%) survivors in the responder group had three or more LEs compared with only two (5.2%) survivors in the non-responder group (P = 0.048). A lower proportion of survivors (20.9%) in non-responder group had grade 2 or higher LEs in comparison with the responder group (37.8%, P = 0.016).
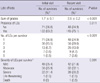
The most common LEs observed at recent visit were related to the endocrine system (Table 2). Of all responders, 43% (83/193) had endocrine LEs, including thyroid (n = 42), growth (n = 33), sexual (n = 42), and metabolic (n = 12) effects. For grade 3 or higher LEs, endocrine (n = 20, 10.4%), and neurologic (n = 9) abnormalities were the most common at recent visit.
In the paired analysis for findings from initial and follow-up visits, increases in both the percentage and the mean severity of specific LEs were seen for many of the body systems. Endocrine-associated LEs increased from 31.6% to 43.0% (P = 0.021) with an increase in mean severity from 0.54 ± 0.06 to 0.74 ± 0.08 (P = 0.002). Musculoskeletal-associated and neurologic LEs increased in number and severity during the follow-up. No significant changes in percentage or severity of LEs were observed in bone marrow or in cardiovascular, auditory, ocular, pulmonary, or renal systems.
Among responders, two patients relapsed. One patient diagnosed with acute lymphoblastic leukemia at the age of 4.8 yr; relapsed at 10 yr. The other patient had non-Hodgkin's lymphoma at 5.7 yr, and developed leukemic transformation at 10.4 yr.
Three patients developed secondary malignancies. One patient with non-Hodgkin's lymphoma was diagnosed with pancreatic neuroendocrine tumor 20.3 yr after the first cancer diagnosis. A patient with acute lymphoblastic leukemia developed glioblastoma multiforme 8.9 yr later. The last patient, with a malignant fibrous histiocytoma, was found to have glioblastoma multiforme 8.6 yr later.
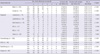
The number of LEs increased in both males and females (P < 0.001). The number of LEs increased regardless of the initial diagnosis, except for neuroblastoma (Table 3). All brain tumor survivors (n = 19) experienced LEs. The percentage of survivors with multiple LEs was higher among brain tumor survivors (52.6% to 84.2%, P < 0.001). Wilms tumor survivors experienced the lowest percentage of LEs (52.4% [11/21]) based on diagnosis.
The number of LEs increased in all treatment groups (i.e., chemotherapy, radiotherapy, and surgery). Survivors treated with radiotherapy had the highest number of LEs, and this number markedly increased during follow-up (P < 0.001).
Increases were seen in the severity and the sum of LEs from initial to recent visit in both male and female survivors (Fig. 1). When assessed by diagnostic groups, all but Wilms tumor and neuroblastoma survivors showed increases in severity and sum of LEs. Brain tumor survivors scored the highest severity and sum at recent visit (2.7 ± 0.1 and 6.3 ± 0.6, respectively). In these patients, both the severity and sum increased during follow-up (P = 0.016 and P < 0.001). For Wilms tumor and neuroblastoma, neither the mean severity nor sum significantly increased from initial to recent visit. Wilms tumor survivors also had the lowest mean severity and sum among diagnostic groups at recent visit.
Mean severity and sum increased in all treatment groups. However, for HSCT survivors, the increase in mean severity from initial to recent visit did not reach statistical significance (P = 0.086). Survivors treated with radiotherapy presented with the highest severity and sum of LEs.
The number, severity, and sum of LEs all increased from initial to recent visit in all age groups (Fig. 2): age at diagnosis (< 2, 2 - 6 and > 6 yr), age at initial visit (> 9, 9-16, > 16 yr), and the number of yr after completion of therapy (< 5, 5-10, > 15 yr). When groups were compared by age at diagnosis, the number, severity, and sum of LEs were all significantly higher in the older age at diagnosis group (> 6 yr).
The number of LEs at follow-up was higher in the older 'age at initial visit' group. However, there were no significant differences in severity and sum for each 'age at initial visit' group at recent LTFC visit. The number, severity, and sum of LEs at follow-up were not significantly different when 'years after completion of therapy' groups were compared.
Age was not significantly associated with change in the number of LEs (Table 4). For diagnostic groups, both brain tumor and lymphoma had a significant effect on the change in number of LEs. Radiotherapy was the only significant treatment factor affecting the change of number of LEs (P = 0.001) as well as the change in grade severity (P = 0.004).
Age at diagnosis and age at first visit were both significant risk factors for changes in sum (Beta -0.649, P = 0.007, Beta 0.642, P = 0.028, respectively). The number of years after completion of therapy showed marginal effects on the change in sum of LEs (Beta -0.423, P = 0.056). When analyzed by diagnostic groups, brain tumor and lymphoma were significant factors for sum (all P = 0.001). Among treatment modalities, only radiotherapy was a significant factor affecting sum (P = 0.001). Wilms tumor was the only diagnosis to have favorable changes in the severity and sum, but the effects were not significant (Beta -0.030, P = 0.773; Beta -0.105, P = 0.346, respectively).
Although LEs in cancer survivors are a well-known health issue, comprehensive follow-up data are limited. Survivors who actively participate in an LTFC follow-up usually expect to be monitored to allow for early detection of complications and cancer recurrences (17). However, comprehensive long-term follow-up is frequently difficult to perform because of limited local resources and expertise. It has been shown that there is a discrepancy between patient self-reports, medical records, and findings on clinical examinations (8, 18).
Our present study was based on 2008 to 2011 follow-up data from an LTFC which opened in 2005. The LTFC provided survivors with continuous and detailed consulting regarding their health, and each patient was examined by an oncologist to assess LEs. As a result, the participation rate in our study was high-about 80%--from our initial report. Survivor participation rate is primarily dependent on patient satisfaction with consulting at an LTFC, and most studies report that over 50% of survivors are lost to follow-up (19-21). High participation rate in this study, along with consulting for survivors' health issues and detailed examination of factors affecting LEs are main strengths of our study.
Most of the survivors experienced additional LEs or had an exacerbation of existing LEs during follow-up. The percentage of survivors with LEs increased from 59.8% at initial visit to 75.1% at final visit. The percentages were similar to other reports: 62.4% in the United States and 74.5% in the Netherlands (2, 8). Increase in the number of LEs can mainly be attributed to survivors' health conditions and follow-up duration. However, selection bias is also a factor. Some survivors refused to participate in the LTFC despite recommendations for LTFC. Although risk factors (e.g., diagnosis and treatment modality) in non-responders were not significantly different than responders, non-responders were older at initial visit than responders. Non-responders also had more time elapsed since the completion of treatment. The mean age at initial visit was 17.4 yr and more than 12.1 yr had passed since they completed their treatment. As these patients grew older and more time passed since completion, the concern or worry about cancer recurrence or LEs lessened (22). In addition, adult survivors can independently decide whether to participate in an LTFC follow-up unlike younger survivors for whom parents play a vital role in caring and monitoring (23).
The number and severity of LEs at initial visit were lower in non-responders than in responders. Non-responders could have been in better general health than other survivors, leading to low participation rate and selection bias (22). According to data from the Childhood Cancer Survivor Study (CCSS), survivors who were followed were significantly more likely to have a chronic health condition compared to those not participating (69.1% in LTFU clinic vs 48.7% with no follow-up) (22). Another reason survivors refuse participate may be to avoid additional emotional trauma by discussing childhood cancer experiences (24). Despite these potential biases, it is important to emphasize that most survivors who were followed at the LTFC showed an increase in the number and severity of LEs. This finding is consistent with other studies on changes of LEs during follow-up (2, 25). Thus, regular follow-up at an LTFC is recommended not only for survivors at risk but also for those who have entered adulthood and are relatively healthier than other survivors.
Both the percentage of patients with LEs and the mean severity of LEs increased during the follow-up for most of the body systems. Particularly, endocrine (including growth or sexual/pubertal effects), musculoskeletal, and neurologic abnormalities became more frequent and severe. Endocrine abnormalities are the most common LEs likely, because survivors of childhood cancers were in the stage of active growth and development of second sexual characteristics during treatment for cancers (2, 8, 11, 26).
Our study found that the number, mean severity, and sum of LEs all were increased, regardless of most clinical factors. The number of LEs, mean severity, and sum were the highest in brain tumor survivors and the lowest among Wilms tumor survivors. These findings were consistent with previous reports (2, 10, 11, 27). On the other hands, it is striking that the risk of death was still higher among these survivors than the general population when they were followed continuously (28). Therefore, survivors of Wilms tumor should also undergo comprehensive follow-up at an LTFC.
Lymphoma was also found to be a significant factor for change in the sum and the number of LEs by multivariate analysis. It has been previously reported that lymphoma is a risk factor for developing cardiovascular LEs, secondary cancers or pulmonary abnormalities (29).
In general, the number, severity and sum of LEs increased by age at diagnosis, age at initial visit, and years since completion of treatment. This means that care at an LTFC should be provided to most of survivors, regardless of age. It should also be emphasized that LEs related to development involving endocrine, musculoskeletal, and neurologic systems are most likely to occur. Therefore, adolescents and young adult survivors should be carefully followed.
For the change in sum, all age groups were significant in multivariate analysis. Patients of younger age at the time of diagnosis were at greater risk of showing adverse changes in LEs during follow-up (Beta -0.649, P = 0.007). Older age at the first visit to the LTFC was found to be a risk of developing LEs in the future (Beta 0.642, P = 0.028). Although the significance was marginal, the risk of developing LEs decreased as survivors aged and more time passed since completing treatment (Beta -0.423, P = 0.056). According to these findings, survivors diagnosed at young age should be regularly and frequently followed. If survivors' first visits are at an older age, they should initially be examined more frequently. The first visit at older age implies that survivors might have lost the opportunity for early LE detection and timely treatment.
Cancer survivorship program is the emerging field in oncology. In the Western countries, the survivorship care protocols have been published and used. Many cancer centers have long-term follow-up clinics for childhood cancer survivors (30). In Asia-Pacific regions including Korea, the survivorship programs are under development. We published the first comprehensive report on the childhood cancer survivors in Korea in 2009 and the nationwide study activities for cancer survivors just have started (11, 30, 31).
Our study has some unique points. Late effects in survivors were confirmed in person by oncologists, and the cohort was comprehensively followed for 3 yr. We could also characterize non-responders to follow-up at the LTFC. Finally, this follow-up report is the first evaluating patients in Asia; similar data are still insufficient worldwide. A major limitation of this study is the small sample size. We tried to overcome this limitation by performing comprehensive follow-ups of the survivors.
In conclusion, LEs are common in childhood cancer survivors. Regardless of most clinical risk factors, the number and severity of LEs tend to increase over time. Survivors of childhood cancer need careful and comprehensive follow-up in order to identify and manage LEs.
Figures and Tables
Fig. 1
Severity and sum of grades of late effects in childhood cancer survivors by demographic and clinical factors. (A) Demographics and treatment factors, (B) Diagnosis. *Significantly different between initial and recent follow-up data (P < 0.05). HSCT, hematopoietic stem cell transplantation; NB, neuroblastoma; RT, radiotherapy; WT, Wilms tumor.

Fig. 2
Number, severity and sum of grades of late effects in childhood cancer survivors by age. (A) Age at diagnosis (yr), (B) Age at initial visit (yr), (C) Years after treatment completion (yr). Number, severity and sum of grades in each age group were all significantly different between initial and follow-up visits. *Data significantly different between two recent visits for each age group (using analysis of variance and post hoc testing by least significant difference [P < 0.05]).

Table 2
Change in number, proportion and severity of late effects by system from initial to recent visit
References
1. McGregor LM, Metzger ML, Sanders R, Santana VM. Pediatric cancers in the new millennium: dramatic progress, new challenges. Oncology (Williston Park). 2007. 21:809–820.
2. Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows AT, Friedman DL, Marina N, Hobbie W, Kadan-Lottick NS, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006. 355:1572–1582.
3. Skinner R, Wallace WH, Levitt GA. UK Children's Cancer Study Group Late Effects Group. Long-term follow-up of people who have survived cancer during childhood. Lancet Oncol. 2006. 7:489–498.
4. Dickerman JD. The late effects of childhood cancer therapy. Pediatrics. 2007. 119:554–568.
5. Bongers ME, Francken AB, Rouwé C, Kamps WA, Postma A. Reduction of adult height in childhood acute lymphoblastic leukemia survivors after prophylactic cranial irradiation. Pediatr Blood Cancer. 2005. 45:139–143.
6. Aslett H, Levitt G, Richardson A, Gibson F. A review of long-term follow-up for survivors of childhood cancer. Eur J Cancer. 2007. 43:1781–1790.
7. Landier W, Wallace WH, Hudson MM. Long-term follow-up of pediatric cancer survivors: education, surveillance, and screening. Pediatr Blood Cancer. 2006. 46:149–158.
8. Geenen MM, Cardous-Ubbink MC, Kremer LC, van den Bos C, van der Pal HJ, Heinen RC, Jaspers MW, Koning CC, Oldenburger F, Langeveld NE, et al. Medical assessment of adverse health outcomes in long-term survivors of childhood cancer. JAMA. 2007. 297:2705–2715.
9. Eakin EG, Youlden DR, Baade PD, Lawler SP, Reeves MM, Heyworth JS, Fritschi L. Health status of long-term cancer survivors: results from an Australian population-based sample. Cancer Epidemiol Biomarkers Prev. 2006. 15:1969–1976.
10. Reulen RC, Winter DL, Lancashire ER, Zeegers MP, Jenney ME, Walters SJ, Jenkinson C, Hawkins MM. Health-status of adult survivors of childhood cancer: a large-scale population-based study from the British Childhood Cancer Survivor Study. Int J Cancer. 2007. 121:633–640.
11. Han JW, Kwon SY, Won SC, Shin YJ, Ko JH, Lyu CJ. Comprehensive clinical follow-up of late effects in childhood cancer survivors shows the need for early and well-timed intervention. Ann Oncol. 2009. 20:1170–1177.
12. Children's Oncology Group. Long-term follow-up guidelines for survivors of childhood, adolescent, and young adult cancers. accessed on 25 September 2012. Available at http://www.childrensoncologygroup.org/disc/le/pdf/LTFUGuidelines.pdf.
13. Scottish Intercollegiate Guidelines Network. Long term follow up of survivors of childhood cancer: a national clinical guideline. accessed on 25 September 2012. Available at http://www.sign.ac.uk/pdf/sign76.pdf.
14. Skinner R, Wallace WH, Levitt GA. Therapy based long-term follow up: practice statement United Kingdom Children's Cancer Study Group. accessed on 25 September 2012. Available at http://www.cclg.org.uk/library/19/PracticeStatement/LTFUfull.pdf.
15. Blazar BR, Weisdorf DJ, Defor T, Goldman A, Braun T, Silver S, Ferrara JL. Phase 1/2 randomized, placebo-control trial of palifermin to prevent graft-versus-host disease (GVHD) after allogeneic hematopoietic stem cell transplantation (HSCT). Blood. 2006. 108:3216–3222.
16. Arbuckle RB, Huber SL, Zacker C. The consequences of diarrhea occurring during chemotherapy for colorectal cancer: a retrospective study. Oncologist. 2000. 5:250–259.
17. Frew G, Smith A, Zutshi B, Young N, Aggarwal A, Jones P, Kockelbergh R, Richards M, Maher EJ. Results of a quantitative survey to explore both perceptions of the purposes of follow-up and preferences for methods of follow-up delivery among service users, primary care practitioners and specialist clinicians after cancer treatment. Clin Oncol (R Coll Radiol). 2010. 22:874–884.
18. Taylor N, Absolom K, Michel G, Urquhart T, Gerrard M, Jenkins A, Lee V, Vora A, Eiser C. Comparison of self-reported late effects with medical records among survivors of childhood cancer. Eur J Cancer. 2010. 46:1069–1078.
19. Michel G, Greenfield DM, Absolom K, Ross RJ, Davies H, Eiser C. Late Effects Group Sheffield. Follow-up care after childhood cancer: survivors' expectations and preferences for care. Eur J Cancer. 2009. 45:1616–1623.
20. Oeffinger KC, Mertens AC, Hudson MM, Gurney JG, Casillas J, Chen H, Whitton J, Yeazel M, Yasui Y, Robison LL. Health care of young adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Ann Fam Med. 2004. 2:61–70.
21. Taylor A, Hawkins M, Griffiths A, Davies H, Douglas C, Jenney M, Wallace WH, Levitt G. Long-term follow-up of survivors of childhood cancer in the UK. Pediatr Blood Cancer. 2004. 42:161–168.
22. Ness KK, Leisenring W, Goodman P, Kawashima T, Mertens AC, Oeffinger KC, Armstrong GT, Robison LL. Assessment of selection bias in clinic-based populations of childhood cancer survivors: a report from the childhood cancer survivor study. Pediatr Blood Cancer. 2009. 52:379–386.
23. James K, Keegan-Wells D, Hinds PS, Kelly KP, Bond D, Hall B, Mahan R, Moore IM, Roll L, Speckhart B. The care of my child with cancer: parents' perceptions of caregiving demands. J Pediatr Oncol Nurs. 2002. 19:218–228.
24. Casillas J, Kahn KL, Doose M, Landier W, Bhatia S, Hernandez J, Zeltzer LK. Padres Contra El Cáncer. Transitioning childhood cancer survivors to adult-centered healthcare: insights from parents, adolescent, and young adult survivors. Psychooncology. 2010. 19:982–990.
25. Lorenzi MF, Xie L, Rogers PC, Pritchard S, Goddard K, McBride ML. Hospital-related morbidity among childhood cancer survivors in British Columbia, Canada: report of the childhood, adolescent, young adult cancer survivors (CAYACS) program. Int J Cancer. 2011. 128:1624–1631.
26. Nandagopal R, Laverdière C, Mulrooney D, Hudson MM, Meacham L. Endocrine late effects of childhood cancer therapy: a report from the Children's Oncology Group. Horm Res. 2008. 69:65–74.
27. Anderson NE. Late complications in childhood central nervous system tumour survivors. Curr Opin Neurol. 2003. 16:677–683.
28. Termuhlen AM, Tersak JM, Liu Q, Yasui Y, Stovall M, Weathers R, Deutsch M, Sklar CA, Oeffinger KC, Armstrong G, et al. Twenty-five year follow-up of childhood Wilms tumor: a report from the Childhood Cancer Survivor Study. Pediatr Blood Cancer. 2011. 57:1210–1216.
29. Ng AK, LaCasce A, Travis LB. Long-term complications of lymphoma and its treatment. J Clin Oncol. 2011. 29:1885–1892.
30. Ghim TT. Time to establish multidisciplinary childhood cancer survivorship programs in Korea. Korean J Hematol. 2010. 45:84–87.
31. Park HJ. Long-term follow-up study and long-term care of childhood cancer survivors. Korean J Pediatr. 2010. 53:465–470.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download