Abstract
With rapid population aging, the socioeconomic burden caused by dementia care is snowballing. Although a few community-based studies of Alzheimer's disease (AD) have been performed in Korea, there has never been a nationwide hospital-based study thereof. We aimed to identify the demographics and clinical characteristics of mild-to-moderate AD patients from the Clinical Research Center for Dementia of Korea (CREDOS) registry. A total of 1,786 patients were consecutively included from September 2005 to June 2010. Each patient underwent comprehensive neurological examination, interview for caregivers, laboratory investigations, neuropsychological tests, and brain MRI. The mean age was 74.0 yr and the female percentage 67.0%. The mean period of education was 7.1 yr and the frequency of early-onset AD (< 65 yr old) was 18.8%. Among the vascular risk factors, hypertension (48.9%) and diabetes mellitus (22.3%) were the most frequent. The mean score of the Korean version of Mini-Mental State Examination (K-MMSE) was 19.2 and the mean sum of box scores of Clinical Dementia Rating (CDR-SB) 5.1. Based on the well-structured, nationwide, and hospital-based registry, this study provides the unique clinical characteristics of AD and emphasizes the importance of vascular factors in AD in Korea.
Alzheimer's disease (AD) is the most common cause of dementia and accounts for 60%-70% of all dementias. The prevalence of AD in population usually increases with age, especially over the age of 65. Korea is among the countries with the most rapidly aging population. With the increasing elderly population in Korea, the number of dementia patients is estimated to reach nearly a million by 2027, according to the report of the Ministry of Health, Welfare, and Family Affairs (1). Therefore, the socioeconomic burden of AD is expected to soar in the coming decades and this will have an impact on the policy guidelines for health and welfare. So far, however, there has been no systemized nationwide hospital-based clinical and epidemiologic study undertaken for AD in the country.
There have been several, regional and nationwide, community-based studies of AD available in Korea (2-4). According to the results of these studies, age-standardized prevalence was 6%-8% for dementia and a particular gender (i.e. female) together with low level of education proved to be important risk factors for dementia. However, previous researches mainly focused on the prevalence of dementia which led to inevitable limitations in the demographic data, while the results of neuroimaging studies, including computed tomography (CT) or magnetic resonance imaging (MRI) scans, were not shown in detail. In addition, they lacked practical information from the hospital-based registry.
Furthermore, the cultural and historical background of the Korean people is quite unique. Firstly, the Confuscian culture has influenced the lifestyle of Koreans for a long time since the Chosun Dynasty, the last kingdom of Korea dating back to the early fifteenth century. It was an era when women were prohibited from receiving formal education and engaging in social activities. Secondly, in the aftermath of the Korean War (1950-1953), the war-torn country suffered financial poverty among other postwar crises. Because of these historical backgrounds, the mean level of education of the elderly in Korea is presumed to be low. In addition, the recent pervasive westernized lifestyle of the average Korean daily lives is likely to increase cardiovascular or cerebrovascular burden. Considering these peculiar situations, a comprehensive epidemiologic study of AD in Korea is mandatory in order to understand the present status of dementia and to draw up an effective policy for the future.
To meet this need, the Clinical Research for Dementia of South Korea (CREDOS), a clinical research group consisting of neurologists and psychiatrists specializing in dementia, has been funded by the the Ministry of Health, Welfare, and Family Affairs since 2005. The centers included in the CREDOS have started a longitudinal registry study (CREDOS study) to build up a hospital-based registry of dementia patients. In this study we examined a large set of patients who have been diagnosed with mild-to-moderate AD from the total CREDOS registry. The aim of our study is to identify unique demographic and clinical characteristics of mild-to-moderate AD patients in Korea.
From September 2005 to June 2010, patients with mild-to-moderate AD visiting the clinics for memory disorders at 31 different CREDOS participating centers were consecutively included. A total of 1,786 patients were selected based on the following inclusion and exclusion criteria. These patients, who were mostly from the out-patient clinics, and in part from the in-patient clinics, were either self-referred or referred from primary clinics. All the patients met the probable AD criteria proposed by the National Institute of Neurological and Communicative Disorders and Stroke and AD and Related Disorders Association (NINCDS-ADRDA) (5) as well as Diagnostic and Statistical Manual of Mental Disorders, Fourth edition (DSM-IV) (6). Some patients met both of the full diagnostic criteria for AD and subcortical vascular dementia (SVaD), which meant mixed cases. We considered these patients as having AD with white matter changes. The severity of dementia was assessed by Clinical Dementia Rating (CDR) (7), and "mild-to-moderate" dementia was defined as CDR 0.5, 1, or 2. Each patient underwent comprehensive medical and neurological examinations. Caregivers were interviewed in-depth by neurologists or psychiatrists, and neuropsychologists. Patients who had clinical evidence of stroke were excluded. All the patients underwent brain MRI and the patients with "severe" (described later) white matter intensities were also excluded, as were patients with structural lesions such as territorial infarction, intracranial hemorrhage, brain tumor, and hydrocephalus. Those with current or past neurological or psychiatric illnesses such as schizophrenia, epilepsy, brain tumor, encephalitis, and severe head trauma were ruled out. We left it to the physician's judgment whether the subjects have depressive disorders or depressive symptoms. If the physician thought it was necessary to consult a psychiatrist, he or she could do so, although not every participant went along with the interview with the psychiatrists. In this registry, all the Axis I psychiatric disorders were excluded. Subjects with physical illnesses or disorders that could interfere with the clinical study such as hearing or vision loss, aphasia, severe cardiac disorders, severe respiratory illnesses, uncontrolled diabetes, hypertension, malignancy, and hepatic or renal disorders were excluded. However, those with histories of well-treated epilepsy or syphilis or malignancies which had not recurred for a long time were included.
We used the Dementia Evaluation Package developed by the CREDOS composed of the Clinical Evaluation Form and the Caregiver Questionnaire Form. The Clinical Evaluation Form included; 1) history of cognitive decline from the caregiver (the onset time was based on the time stated by the caregiver), 2) Korean version of Mini-Mental State Examination (K-MMSE) (8), 3) CDR (7), 4) Global Deterioration Scale (GDS) (9), 5) Hachinski ischemia scale (HIS), 6) neurological examinations, and 7) Geriatric depression scale (GDS-d) (10). The Caregiver Questionnaire Form included; 1) basic demographic data of the patient and caregiver, 2) lifestyle and family history, 3) past medical history including vascular risk factors such as hypertension, diabetes, heart disease, hyperlipidemia, previous stroke history, alcohol, and smoking. Vascular risk factors were regarded as positive either if the patient had previously been diagnosed with associated disease or if he or she was currently under medical treatment for the disease. Smoking history was considered to be positive for both past and current smokers. However, current smokers were only included in statistical analysis. The Caregiver Questionnaire Form also included; 4) Korean Dementia Screening Questionnaire (KDSQ) (11), 5) Barthel activities of daily living (ADL) index, 6) Seoul instrumental ADL (S-IADL) (12) and 7) Korean version of Neuropsychiatric Inventory (K-NPI) (13) (We evaluated the total NPI score and the frequencies of positive NPI items). All the patients underwent laboratory tests including complete blood counts (CBC), chemistry and electrolytes, lipid profile, urinalysis, venereal disease research laboratory (VDRL), thyroid function test, vitamin B12/folate, fibrinogen, and homocysteine. As the previous CREDOS study described, APOE genotype was determined by polymerase chain reaction (PCR) (14). MRI was also performed in all patients, as described later. At the beginning of this registry, the symposium was held in order to standardize diagnostic assessment and to ascertain inter-center and intra-center reliability. In the middle of the registry, neurologists, psychiatrists, research nurses, and psychologists had a regular meeting in order to check the quality of data every 3rd Saturday.
We examined a standardized neuropsycholgical battery, the Seoul Neuropsyhcological Screening Battery (SNSB) (15) in all patients. The SNSB contains tests for verbal and visual memory, visuoconstructive function, frontal/executive function, attention, language, praxis, and four elements of Gerstmann syndrome. Age-, sex-, and education-specific norms for each test based on 447 normal subjects were available. The scores of scorable cognitive tests were classified as abnormal when they were below the 16th percentiles of the norms. If any task in the descriptive items was found to be abnormal by a neuropsychologist, the domain was categorized as "abnormal". We also obtained the total score of SNSB by a method identical to that described previous literatures (16), except that we modified the score of frontal/executive function from 70 to 60. The total score was 290 and consisted of subscores from each cognitive domain as follows: attention, 17; language and related function, 27; visuospatial function, 36; memory, 150; and frontal/executive function, 60.
MRI was performed based on the protocol of MRI acquisition for CREDOS registration; T1 axial, T2 axial, fluid attenuated inversion recovery (FLAIR) axial, gradient echo axial, and thin-slice (0.5-1 mm) T1 coronal series. We evaluated the severity of white matter hyperintensities (WMH) according to the modified Fazekas and Scheltens scale on the T2 axial or FLAIR images. WMH were evaluated in periventricular white matter (PWM, P rating) and deep white matter (DWM, D rating) areas separately and the D and P ratings were combined to provide a final ischemia score. DWM lesions were divided into D1 (DWM < 10 mm), D2 (10 ≤ DWM < 25 mm), and D3 (≥ 25 mm) based on the longest diameter of lesions. PWM lesions were classified into P1 (cap and band < 5 mm), P2 (between P1 and P3), and P3 (cap or band ≥ 10 mm) based on the size of cap and band, which were perpendicular and horizontal to the ventricle, respectively. The results were combined to provide a representative rating as minimal (D1P1, D1P2), moderate (neither minimal nor severe group), or severe (D3P3). In our study, MRI of all patients met the rating of minimal or moderate ischemia and the patients with severe ischemia (D3P3) were excluded.
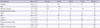
Table 1 shows the demographic and clinical characteristics of the 1,786 patients. The most prevalent age group was the 8th decade, which consisted of 926 patients (51.8%). Female patients attributed to 67.0% and 18.8 percent of the patients were categorized as early-onset AD (EOAD, < 65 yr old). APOE genotyping was performed in 957 patients, of whom 410 (42.8%) were positive for ε4 with 68 (7.1%) patients being homozygous for ε4 and 342 (35.8%) patients being heterozygous for ε4. There were 337 patients (18.9%) who had a family history of dementia. Patients who used the mobile phone accounted for 51.3% (917/1,786), while those who drove motor vehicles represented 6.8% (122/1,786). Those who were known to have occupations were 212 patients (11.9%). Regarding the body mass index (BMI), there were 424 (23.7%) patients who had BMI of 25 or greater. Vision was preserved in 48.3% of the patients and hearing in 83.7%.
Among the caregivers, the spouse looked after the patient in 28.9%, while the son, daughter, daughter-in-law constituted 23.9%, 26.5%, and 15.6%, respectively. Female made up 62.7% of the caregivers. Seven hundred and fifty-five (42.3%) caregivers did not reside with the patients. The largest age group of caregivers was the 5th decade (503; 28.1%) while the second largest was the 6th decade (392; 21.9%).
Among the vascular risk factors, hypertension (48.9%) and diabetes mellitus (22.3%) were most frequent in our patients, followed by current alcohol drinker (19.4%), family history of stroke (18.5%), cardiac disease (14.6%), and hypercholesterolemia (13.8%), in the order of frequency (Table 2). At least any one of these vascular risk factors was found in 1,106 (61.9%). The mean total cholesterol level was 194.8 ± 135.2 mg/mL and the mean LDL cholesterol level was 116.3 ± 70.3 mg/mL. Other than cardiovascular risk factors, anemia (23.9%) was the most commonly associated medical condition, followed by cancer (20.2%), renal disease (16.1%), and fracture of long bone (9.7%), in the order of frequency. Depression was also one of the items of comorbidity evaluation and according to the patients or their caregivers, only 66 patients (3.7%) reported to have previous or current depression.
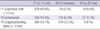
Table 3 shows the characteristics of cognition, ADL indices, and neuropsychiatric symptoms of AD patients. The mean CDR and CDR-SB were 0.9 and 5.1, respectively. The mean K-MMSE score was 19.2 and the mean GDS was 4.1. The mean total score of SNSB-D, the mean score of verbal memory of SNSB-D, and the mean score of visual memory of SNSB-D was 99.0, 11.3, and 5.7, respectively.
The number of patients assessed as CDR 0.5, 1, and 2 were 809 (45.3%), 770 (43.1%) and 207 (11.6%), respectively. The number of patients assessed as GDS 3, 4, 5, and 6 were 404 (22.6%), 798 (44.7%), 510 (28.6%), and 74 (4.1%). Mean Hachinski ischemic score was 2.4 and GDS-d was 14.8. Although there were only 66 patients (3.7%) who had histories of previous or current depression on the comorbidity evaluation as described already, there were 693 patients (38.8%) who scored 18 or more on GDS-d which suggested clinically moderate depression, and there were 903 patients (50.6%) with depression in NPI. Neuropsychiatric symptoms were found in 85.7% of the patients. Depression (50.6%), apathy (49.6%), irritability (42.0%), and anxiety (41.35%) were common among the patients with neuropsychiatric problems (Fig. 1). The mean Barthel ADL index was 19.0 ± 2.2 and the mean Instrumental ADL index in current state and in potential ability was 17.6 ± 9.8 and 14.4 ± 9.4, respectively.
D1 was observed in 1,375 patients (77.0%) and P1 was shown in 888 patients (49.7%). D3 was identified in only 41 patients (2.3%) and P3 in 499 patients (27.9%). The ischemia level was minimal in 1,095 patients (61.2%) and moderate in 691 patients (38.8%) (Table 4).
This is the first nationwide hospital-based study depicting the clinicoepidemiological profile of mild-to-moderate AD in Korea. Up until now, obtaining a bird's eye view of AD across the country had been difficult. There have been several reports on the prevalence and subtypes of dementia in Korea, but they were community-based, rather than being hospital-based, and focused only on the clinical and neuropsychological profiles (2, 3, 17). Furthermore, even in nationally representative studies from the Western countries, large-sampled, hospital-based studies with in-depth assessment including neuroimaging studies were rare. In contrast, our study was based on not only clinical and comprehensive neuropsychological profiles, but also neuroimaging studies.
Old age is a well-known risk factor of AD throughout the world, while, in Europe and Asian countries, women have been identified to be more prone to the development of dementia (18, 19). The findings in our AD population were in accordance with those results, in that the prevalence increased with age up to the 8th decade and that women were affected twice as much as men. The largest age group involved in our study was the 8th decade, which possibly might have been even older had it not been for the higher morbidity and mortality in the older population. Those older than 79 yr of age are more prone to comorbid medical illnesses and more severe dementia, which could make the family members more reluctant to seek medical attention, particularly the dementia clinic.
Another interesting finding of our study is that the proportion of EOAD was higher than expected, accounting for 18.8% of AD. Given that this study was based on the hospital-based registry into consideration, the proportion may be overestimated. However, in Korea, studies focusing on the prevalence of early-onset dementia are lacking, as opposed to those on the prevalence of dementia in the elderly people. Therefore, the result of this study could provide another important consideration in the policy-making process. Although patients with EOAD may be affected more severely in terms of economical and social status, by and large they have been neglected in terms of facilities or government subsidies. As mentioned earlier, the number of demented patients in Korea is estimated to be a million in 2027 and the number of AD patients will roughly reach 600,000. Therefore, the estimated number of EOAD patients which accounts for nearly one fifth of AD will be almost 120,000. Furthermore, our results showed that the family history of dementia was higher in early onset (23.9%) than in late onset AD (18.9%). In the Western countries, the incidence of probable EOAD per 100,000 was reported to be 7.2-22.6 (20, 21), constituting about 6% of AD patients. In addition to these practical implications, the clinical, genetic and neuroimaging profile of this population may be different from those of late-onset AD and should be further worked out in detail.
Considering the strong association between vascular risk factors and AD, we need to control modifiable factors such as hypertension, diabetes, and hyperlipidemia in general population more strictly. In this study, we found that almost half (48.9%) of mild-to-moderate AD had hypertension. Diabetes (22.3%) was the second most common vascular factor in AD patients. Hyperlipidemia was found in 13.8% of AD patients. MRI analysis revealed that a significant portion of AD patients (38.8%) had a moderate degree of white matter high signal intensities, suggesting that concomitant cerebrovascular lesions are not rare. There is growing evidence that vascular risk factors such as hypertension (22), hyperlipidemia (23), and diabetes mellitus (24) are implicated in the development of AD. Composites of the risk factors seem to increase the risk for dementia in a dose-dependent fasion (25). In addition, identification and management of these vascular factors are of clinical importance since vascular factors may have potential modifiability and could promote clinical expressions of of AD (26). It was difficult to compare between vascular factors in this study and those in the Western countries because of methological issues. The studies concerning cardiovascular risk factors in AD reported in the Western world were not cross-sectional, but mostly longitudinal ones unlike our study. The results from longitudinal studies suggest that single factor or multiple vascular risk factors was robustly associated with the increased risk of dementia (23, 25).
Neuropsychiatric symptoms are common in AD. Several studies have estimated the prevalence of the neuropsychiatric symptoms of AD to be from 70% to 90% (27, 28). Apathy, depression, irritability and agitation were frequently reported symptoms in previous studies, while euphoria was the least frequent (28). In our study, 85.7% of the patients had exhibited at least one neuropsychiatric symptom in the previous month. Depression, apathy, irritability, and anxiety were the most common symptoms, and euphoria was the least common behavioral abnormality. However, as opposed to the previous studies (28) that reported apathy to be the number one behavioral change, depression was the most frequent behavioral change in our population. According to the structured interview for apathy, only 7% met criteria for apathy, which was significantly lower than other studies for mild dementia patients (29). Because apathy and depression are frequently associated and share key symptoms, it is difficult to make definitive distinctions between them (30). It is noted that when the caregivers were given a single question as to whether the patients had a history of previous or current depression, only 3.7% responded "yes". However, the figure rose to over half when assessed by NPI which explores the presence of depression with more detailed questions. Therefore, this discrepancy suggests that depression is the most frequent but underestimated symptom in mild-to-moderate AD patients in Korea.
There are some limitations to this study. First of all, although it was a nationwide study, the results were derived from hospitalbased data, which may not represent the population as a whole, and consequently result in a selection bias. Therefore, the findings of this study cannot be generalized to the whole Korean population. Secondly, there is a possibility that patients with mixed AD and cerebrovascular disease may have been unintentionally included in our study, since we did not exclude the patients with moderate ischemia from the study. Up to now, there is no confirmative method available to differentiate these two conditions on clinical grounds. Furthermore, the inclusion of AD patients with mild to moderate ischemia instead of those with no ischemia may better reflect AD patients in the real world, since it is widely believed that AD with cerebrovascular lesion is more common than pure Alzheimer's disease. Thirdly, the documented clinical information of the subjects included in the study lacked in the data regarding the presence or absence of a family history of Down syndrome, the use of anti-oxidant agents or estrogen replacement, and information concerning leisure activities of the patients. In addition, information concerning the use of cholinesterase inhibitors was not available for analysis.
This is the first attempt in Korea that has implemented a well-designed and systemized clinico-epidemiologic study that includes laboratory tests and MRI findings, guaranteeing the diagnostic precision of a large number of patients labeled as mild-to-moderate AD. This study could shed new light on the indigenous characteristics of AD and underline the importance of vascular factors in AD in Korea. Additionally, not only will it serve as a reference for future epidemiological or clinical studies, it will also provide an important basis for government policy-making. Further longitudinal study using this registry is needed to investigate the natural course of AD in Korea.
Figures and Tables
Fig. 1
The frequency of Neuropsychiatric Inventory items. Del, delusion; Hal, hallucination; Agt, agitation; Dep, depression; Anx, anxiety; Eup, euphoria; Apa, apathy; Dis, disinhibition; Irrit, irritability; Mot, aberrant motor behavior; Sle, sleep; App, appetite.

Table 2
Vascular risk factors and other comorbid conditions in patients with Alzheimer's disease based on the caregiver's statement

Table 3
Baseline characteristics of cognitive, functional and neuropsychological assessment (n = 1,786)
SD, standard deviation; K-MMSE, Korean version of Mini-Mental State Examination; CDR, clinical dementia rating; KDSQ, Korean Dementia Screening Questionnaire; BADL, Barthel activities of daily living index; S-IADL-C, Seoul instrumental activities of daily living-current capacities; S-IADL-P, Seoul instrumental activities of daily living-potential capacities; K-NPI, Korean version of Neuropsychiatric inventory.
AUTHOR SUMMARY
Clinical Characteristics of a Nationwide Hospital-based Registry of Mild-to-Moderate Alzheimer's Disease Patients in Korea: A CREDOS (Clinical Research Center for Dementia of South Korea) Study
Hee Kyung Park, Ji-Young Kim, Seol-Heui Han, Duk L. Na, Hae-Kwan Cheong, Seong Yoon Kim, SangYun Kim, Chang Hyung Hong, Do-Kwan Kim, Bon D. Ku, So Young Moon, Jun-Young Lee, Yong S. Shim, Young Chul Youn, Eun-Joo Kim, Beoung-Chae Kim, Kee Hyung Park, Kyung R. Cha, Sang Won Seo and Jae-Hong Lee
This nationwide study shows the demographics and clinical characteristics of mild-to-moderate Alzheimer's disease (AD) patients from the Clinical Research Center for Dementia of South Korea (CREDOS) cohort. We found that the most common age group was the 8th decade and the percentage of females was 67%. With regard to vascular risk factors, hypertension and diabetes were the most common factors in AD. Brain MRI revealed moderate white matter ischemia in about 40% of the patients, suggesting that mixed AD with cerebrovascular disorder may be more common than previously thought. These findings derived from the hospital-based registry enabled us to obtain a bird's eye view of Korean AD patients, and provided an access to more accurate demographic picture of AD in Korea.
References
1. The Ministry of Health Wefare and Family Affairs. Nationwide study on the prevalence of dementia in Korean elders. 2008. Seoul: The Ministry.
2. Suh GH, Kim JK, Cho MJ. Community study of dementia in the older Korean rural population. Aust N Z J Psychiatry. 2003. 37:606–612.
3. Jhoo JH, Kim KW, Huh Y, Lee SB, Park JH, Lee JJ, Choi EA, Han C, Choo IH, Youn JC, Lee DY, Woo JI. Prevalence of dementia and its subtypes in an elderly urban Korean population: results from the Korean Longitudinal Study on Health and Aging (KLoSHA). Dement Geriatr Cogn Disord. 2008. 26:270–276.
4. Kim KW, Park JH, Kim MH, Kim MD, Kim BJ, Kim SK, Kim JL, Moon SW, Bae JN, Woo JI, Ryu SH, Yoon JC, Lee NJ, Lee DY, Lee DW, Lee SB, Lee JJ, Lee JY, Lee CU, Chang SM, Jhoo JH, Cho MJ. A nationwide survey on the prevalence of dementia and mild cognitive impairment in South Korea. J Alzheimers Dis. 2011. 23:281–291.
5. McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984. 34:939–944.
6. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 1994. 4th ed. Washington DC: American Psychiatric Association.
7. Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993. 43:2412–2414.
8. Kang Y, Na DL, Hahn S. A validity study on the Korean mini-mental state examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997. 15:300–308.
9. Reisberg B, Ferris SH, de Leon MJ, Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982. 139:1136–1139.
10. Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982. 17:37–49.
11. Yang DW, Cho BL, Chey JY, Kim SY, Kim BS. The development and validation of Korean Dementia Screening Questionnaire (KDSQ). J Korean Neurol Assoc. 2002. 20:135–141.
12. Ku HM, Kim JH, Kwon EJ, Kim SH, Lee HS, Ko HJ, Jo S, Kim DK. A study on the reliability and validity of Seoul-Instrumental Activities of Daily Living (S-IADL). J Korean Neuropsychiatr Assoc. 2004. 43:189–199.
13. Choi SH, Na DL, Kwon HM, Yoon SJ, Jeong JH, Ha CK. The Korean version of the neuropsychiatric inventory: a scoring tool for neuropsychiatric disturbance in dementia patients. J Korean Med Sci. 2000. 15:609–615.
14. Hong YJ, Yoon B, Shim YS, Cho AH, Shin HE, Kim YI, Kim SY, Yang DW. APOE ε4 allele status in Korea dementia patients with severe white matter hyperintensities. J Alzheimers Dis. 2011. 24:519–524.
15. Kang Y, Na D. Seoul neuropsychological screening battery. 2003. Incheon: Human Brain Research & Consulting Co..
16. Ahn HJ, Chin J, Park A, Lee BH, Suh MK, Seo SW, Na DL. Seoul Neuropsychological Screening Battery-dementia version (SNSB-D): a useful tool for assessing and monitoring cognitive impairments in dementia patients. J Korean Med Sci. 2010. 25:1071–1076.
17. Lee DY, Lee JH, Ju YS, Lee KU, Kim KW, Jhoo JH, Yoon JC, Ha J, Woo JI. The prevalence of dementia in older people in an urban population of Korea: the Seoul study. J Am Geriatr Soc. 2002. 50:1233–1239.
18. Kalaria RN, Maestre GE, Arizaga R, Friedland RP, Galasko D, Hall K, Luchsinger JA, Ogunniyi A, Perry EK, Potocnik F, Prince M, Stewart R, Wimo A, Zhang ZX, Antuono P. Alzheimer's disease and vascular dementia in developing countries: prevalence, management, and risk factors. Lancet Neurol. 2008. 7:812–826.
19. Qiu C, Kivipelto M, von Strauss E. Epidemiology of Alzheimer's disease: occurrence, determinants, and strategies toward intervention. Dialogues Clin Neurosci. 2009. 11:111–128.
20. McGonigal G, Thomas B, McQuade C, Starr JM, MacLennan WJ, Whalley LJ. Epidemiology of Alzheimer's presenile dementia in Scotland, 1974-88. BMJ. 1993. 306:680–683.
21. Newens AJ, Forster DP, Kay DW, Kirkup W, Bates D, Edwardson J. Clinically diagnosed presenile dementia of the Alzheimer type in the Northern Health Region: ascertainment, prevalence, incidence and survival. Psychol Med. 1993. 23:631–644.
22. Kennelly SP, Lawlor BA, Kenny RA. Blood pressure and the risk for dementia: a double edged sword. Ageing Res Rev. 2009. 8:61–70.
23. Whitmer RA, Sidney S, Selby J, Johnston SC, Yaffe K. Midlife cardiovascular risk factors and risk of dementia in late life. Neurology. 2005. 64:277–281.
24. Biessels GJ, Staekenborg S, Brunner E, Brayne C, Scheltens P. Risk of dementia in diabetes mellitus: a systematic review. Lancet Neurol. 2006. 5:64–74.
25. Beeri MS, Ravona-Springer R, Silverman JM, Haroutunian V. The effects of cardiovascular risk factors on cognitive compromise. Dialogues Clin Neurosci. 2009. 11:201–212.
26. Qiu C, Winblad B, Fratiglioni L. The age-dependent relation of blood pressure to cognitive function and dementia. Lancet Neurol. 2005. 4:487–499.
27. Tatsch MF, Bottino CM, Azevedo D, Hototian SR, Moscoso MA, Folquitto JC, Scalco AZ, Louzã MR. Neuropsychiatric symptoms in Alzheimer disease and cognitively impaired, nondemented elderly from a community-based sample in Brazil: prevalence and relationship with dementia severity. Am J Geriatr Psychiatry. 2006. 14:438–445.
28. Mega MS, Cummings JL, Fiorello T, Gornbein J. The spectrum of behavioral changes in Alzheimer's disease. Neurology. 1996. 46:130–135.
29. Starkstein SE, Ingram L, Garau ML, Mizrahi R. On the overlap between apathy and depression in dementia. J Neurol Neurosurg Psychiatry. 2005. 76:1070–1074.
30. Tagariello P, Girardi P, Amore M. Depression and apathy in dementia: same syndrome or different constructs? A critical review. Arch Gerontol Geriatr. 2009. 49:246–249.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download