Abstract
In 2009, infection with the liver fluke Clonorchis sinensis (C. sinensis) was classified as "carcinogenic to humans" (Group 1) based on its involvement in the etiology of cholangiocarcinoma by the International Agency for Research on Cancer. However, little is known about the descriptive epidemiology of cholangiocarcinoma in Korea. We examined incidence trends of intrahepatic and extrahepatic cholangiocarcinomas, using data from the Korea National Cancer Incidence database for 1999-2005. The prevalence of C. sinensis infection was estimated from a recent population-based survey in rural endemic areas. Cholangiocarcinoma incidence rates are currently rising, even while primary liver cancer incidence rates are decreasing. Annual percent changes in cholangiocarcinoma incidence rates were 8% for males and 11% in females. Known areas of C. sinensis endemicity showed high incidence rates of cholangiocarcinoma. The positivity of C. sinensis eggs in stool samples from endemic areas was more than 25% of adults tested during 2005-2008. From a meta-analysis, the summary odds ratio for cholangiocarcinoma due to C. sinensis infection was 4.7 (95% confidence interval: 2.2-9.8). Approximately 10% of cholangiocarcinomas in Korea were caused by chronic C. sinensis infections. More specific policies, including health education and an extensive effort for early detection in endemic areas, are needed.
The two liver flukes Clonorchis sinensis (C. sinensis) and Opisthorchis viverrini (O. viverrini) are members of the Opisthorchiidae family (1). These species are considered to be of major social and economic relevance for both humans and animals in Asian countries including China, Korea, Vietnam, Laos, and Thailand (2). In 1994, infection with O. viverrini was classified by the International Agency for Research on Cancer (IARC) as "carcinogenic to humans" (Group 1) based on its involvement in the etiology of cholangiocarcinoma (CCA). Alternatively, infection with C. sinensis was classified as "probably carcinogenic to humans" (Group 2A) because there was only limited evidence for the carcinogenicity of this worm in humans (3).
In Volume 100B from February of 2009, the IARC Monograph Working Group reassessed the carcinogenicity of infection with liver flukes by applying a comprehensive review of all of the available published literature (4). Prevalence of infection with C. sinensis was shown to correlate with the incidence of CCA (5), and several case-control studies showed a high risk for this cancer (6-8).
Therefore, infections with O. viverrini and C. sinensis are now both classified in Group 1 by the IARC, based on "sufficient evidence in humans" for CCA.
Beginning in the 1970's, several papers reported a high correlation between CCA and clonorchiasis in the southern part of the Korean Peninsula (9, 10).
However, little is known about the existing distribution and trend of incidence, and related risk factors of CCA in Korea, a nation where C. sinensis infection is highly prevalent.
In the present paper, incidence rates of CCA and the prevalence of infection with C. sinensis are described in an attempt to evaluate the burden of CCA related to infection with C. sinensis in Korea.
We extracted intrahepatic CCA cases (International Classification of Disease (ICD) 10 code C22.1 (11), ICD-Oncology (ICD-O) (12) code 8160, including adenocarcinoma (ICD-O codes 8140, 8161, 8260, 8440, 8480, and 8560), duct carcinoma (ICD-O code 8500), and Klatskin tumor (ICD-O codes 8162), and extrahepatic CCA: ICD 10 code C24.0) from the Korea National Cancer Incidence Database (KNCIDB). We examined all of the records of CCA reported from 1999 through 2005. Next, we computed the age-standardized incidence rates per 100,000 person-years on the basis of the world standard population. To compare changes in incidence between 1999 and 2005, we calculated the estimated annual percentage change (EAPC). Incidence rates were separately analyzed by sex and region for two calendar periods (1999-2002 and 2003-2005) because Korean national incidence rates in Cancer Incidence in Five Continents volume 9 published by IARC covered the 1999-2002 period and the incidence rates for 2003-2005 were published in 2009 (13, 14).
During 2005-2008, a total of 4,234 subjects (age range: 30-89; mean age: 59.9 yr) were recruited as a part of population-based cohort construction in areas of Haman and Sanchong in Gyeongsangnam-do which was known endemic of C. sinensis; from the basin of the Nakdong River. A trained research assistant interviewed each participant about the demographic characteristics, alcohol drinking and tobacco smoking habits, dietary habits including raw fresh-water fish, and disease history. Stool samples were also collected for laboratory examination. Additionally, informed consent was obtained from all participants, and the study protocol was approved by the National Cancer Center of Korea.
Stool samples were examined using the formalin-ether sedimentation method to identify the presence of C. sinensis eggs. Also, data from national surveys of intestinal parasites from 1971 (1st report) to 2004 (7th report) were used for an estimation of the population-attributable fraction.
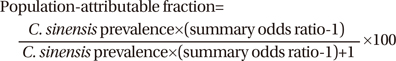
Using published data from cross-sectional (9, 10) and case-control studies (6-8) of CCA with C. sinensis infection, meta-analysis was performed to estimate the risk of CCA. Pooled odds ratios (ORs) with 95% confidence intervals (CIs) were estimated on the basis of both fixed- and random-effect models. Heterogeneity analysis was then carried out to verify if there was a significant difference between studies. The Stata version 10.0 (StataCorp, TX, USA) and Comprehensive Meta-Analysis version 2 (Biostat, NJ, USA) software programs were used for the metaanalysis. Using the formula below, the attributable fraction was estimated using information about the prevalence of C. sinensis infection in 1981 (15) and relative risk estimates from meta-analysis. The calculated attributable fraction was applied to the number of incidence cases of CCA in 2005 in consideration of the latency period.
Since 1999, the annual average incidence of primary liver cancer was 10,500 cases for males and 3,500 cases for females. In addition, a decreasing trend was observed, with an EAPC of approximately -2%. Intrahepatic CCA accounted for approximately 10% of liver cancers (8.8% for males and 10.6% for females) and this proportion increased by year, with levels of 11.6% for males and 22.7% for females in 2005. Intrahepatic CCA rates increased gradually from 2001 (with EAPCs of 7.9% and 10.6% for males and females, respectively); however, the extrahepatic CCA rates were stable during the same period (Table 1). There were approximately 2.5- to 3.0-fold variations by region, with Gyeongsangnam-do having the highest incidence rates for males (Table 2). The increase in the incidence of female cases (168.6%) was higher than that seen for males (149.7%) in recent years (2003-2005) compared to the earlier years examined (1999-2002). Very sharp increases in cases involving both males and females age 50 and over were observed during the time period of 2003 thro-ugh 2005 (Fig. 1).
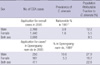
Overall C. sinensis egg positivity in stool was measured at 28.2% (27.6% in 2005; 34.5% in 2006; 25.4% in 2007; 21.7% in 2008) among adults ages 30 and over (the age-standardized prevalence rates were 35.0% and 20.8% for males and females, respectively). A higher prevalence was observed in the 40- to 59-yr-old age group in both males and females (Table 3).
Table 4, Fig. 2 illustrate the risk estimates for CCA according to C. sinensis infection status. The overall odds ratio for CCA due to C. sinensis infection was 4.7 (95% CI: 2.2-9.8). In 2005, 9.5% of CCA cases were attributable to infection with C. sinensis (12.2% for males, 5.5% for females) (Table 5). In the endemic areas, the population-attributable fraction was much higher, at levels of 27.9% and 16.2% for males and females, respectively.
The age-standardized incidence rates of intrahepatic CCA in Korea were 4.1 per 100,000 males and 1.8 per 100,000 females, respectively, from 1999 to 2005 and these are between two and four times higher than those in the United States (e.g., in the 1996-2000 period, White males, 0.92/100,000; Black males, 0.93/100,000; White females, 0.57/100,000; Black females, 0.39/100,000) (16) and England and Wales (e.g., in the 1999-2001 period, males, 1.33/100,000; females, 1.06/100,000) (17). Increases in intrahepatic CCA were observed in our study, correlating well with studies conducted in the United States, England, and Wales (16, 17). The reasons for increases in CCA incidence are not clear. Some part of this increase may be attributed to changes in the coding system, from ICD-O-2 to ICD-O-3, but these changes were not drastic (18). More rapid increases among the elderly might be attributed to complete and accurate cancer registration (14). The CCA incidence was higher in males than in females but the increase in CCA incidence was bigger in females than in males. This might be caused that the greater percent change due to relatively small numbers of CCA case in females than in males. It needs further studies.
Since 1971, national surveys of intestinal parasitic infections have monitored the overall prevalence of C. sinensis in Korea (15). Areas heavily endemic for clonorchiasis in Korea are scattered throughout the country, with the most extensive and intensive endemic regions found mainly along the Nakdong River and the lower reaches of the rivers located in Gyeongsangnam-do (19). The infection status of C. sinensis has shown little change over 25 yr, despite the development of effective antihelminthics such as praziquantel. The repeated consumption of fresh-water fish is one of the main contributing factors for the high prevalence of clonorchiasis, even after intervention with praziquantel (5).
In an ecological study conducted during 2000-2004 in Korea, C. sinensis prevalence (2.1% in Chuncheon, 7.8% in Chungju, and 31.3% in Haman) correlated strongly with CCA incidence rates (0.3, 1.8, and 5.5 per 100,000 persons, respectively) (5).
In Korea, the national liver cancer surveillance program for high-risk patients began in 2002 and is comprised of carriers of hepatitis B virus or C virus. Any individuals with current or prior C. sinensis infection are also part of the high-risk group for the contraction of primary liver cancer in areas endemic for C. sinensis. Therefore, these high-risk individuals should be included in the surveillance program.
Apart from clonorchiasis, a main risk factor of CCA, the other known risk factors include chronic infection with hepatitis B and C viruses (HBV and HCV), liver cirrhosis, chronic non-alcoholic liver disease, obesity and hepatolithiasis (4, 20, 21). A possible association between HBV and HCV-known to cause hepatocellular carcinoma- and CCA was reported by IARC as there is only limited human evidence (4). Both intrahepatic CCA and extrahepatic CCA are well-known complications of Primary Scleosing Cholangitis (PSC) in Western countries (22).
Among these risk factors, hepatolithiasis is a very uncommon disease in the West, in contrast, intra- and extrahepatic bile duct stones are much more common in Eastern Asia (23). Hepatolithiasis is strongly associated with CCA with proportions varying from 10% in Japan, 35% in Korea to more than 60% in Taiwan (China) (24-26).
In conclusion, approximately 10% of CCA cases are estimated due to infection with C. sinensis (12% for males, 6% for females). In contrast, C. sinensis infection causes a quarter of CCA cases in the endemic area. Even though the control of C. sinensis is successful due to very effective chemotherapy using praziquantel, CCA risk has been continuously increasing, particularly in areas hyper-endemic for C. sinensis infection. A more straightforward policy for the prevention of C. sinensis infestation that includes health education to avoid repeated consumption of raw freshwater fish and an extensive effort for early detection targeting those who are currently or have been infected with C. sinensis in endemic areas is strongly needed.
Figures and Tables
Fig. 1
Age specific incidence rates of cholangiocarcinoma by sex for 1999-2000 and 2003-2005. (A) Intrahepatic, (B) Extrahepatic.

Table 1
Number of cases and age-standardized incidence rates of liver cancer (C22), intrahepatic cholangiocarcinoma (C22.1), and extrahepatic cholangiocarcinoma (C24.0) in Korea, 1999-2005

Table 2
Age-standardized incidence rates of cholangiocarcinoma (CCA) by region in Korea over two time periods: 1999-2002 and 2003-2005
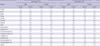
Table 3
Prevalence of Clonorchis sinensis among residents in the endemic area, Gyeongsangnam-do: 2005-2008

Table 4
Summary of study characteristics for cholangiocarcinoma according to Clonorchis sinensis infection status in Korea

Table 5
Clonorchis sinensis infection-attributable cholangiocarcinoma in Korea, 2005
*C. sinensis prevalence in 1981 (Total=2.6%, M=3.8%, F=1.6%) (Ref [15]); †cases with patients age 30 or over; ‡% among patients age 30 or over.
(Source: Prevalence of intestinal parasitic infections in Korea: the 3rd report. The Ministry of Health and Social Affairs. The Korea Association of Parasite Eradication. 1981).
CCA, cholangiocarcinoma.
References
2. Lun ZR, Gasser RB, Lai DH, Li AX, Zhu XQ, Yu XB, Fang YY. Clonorchiasis: a key foodborne zoonosis in China. Lancet Infect Dis. 2005. 5:31–41.

3. International Agency for Research on Cancer. Schistosomes, liver flukes and Helicobactor pylori. IARC monographs on the evaluation of carcinogenic risks to humans. 1994. vol. 61. Lyon France: International Agency for Research on Cancer.
4. Bouvard V, Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, Benbrahim-Tallaa L, Guha N, Freeman C, Galichet L, Cogliano V. A review of human carcinogens-Part B: biological agents. Lancet Oncol. 2009. 10:321–322.

5. Lim MK, Ju YH, Franceschi S, Oh JK, Kong HJ, Hwang SS, Park SK, Cho SI, Sohn WM, Kim DI, Yoo KY, Hong ST, Shin HR. Clonorchis sinensis infection and increasing risk of cholangiocarcinoma in the Republic of Korea. Am J Trop Med Hyg. 2006. 75:93–96.

6. Shin HR, Lee CU, Park HJ, Seol SY, Chung JM, Choi HC, Ahn YO, Shigemastu T. Hepatitis B and C virus, Clonorchis sinensis for the risk of liver cancer: a case-control study in Pusan, Korea. Int J Epidemiol. 1996. 25:933–940.

7. Choi D, Lim JH, Lee KT, Lee JK, Choi SH, Heo JS, Jang KT, Lee NY, Kim S, Hong ST. Cholangiocarcinoma and Clonorchis sinensis infection: a case-control study in Korea. J Hepatol. 2006. 44:1066–1073.

8. Lee TY, Lee SS, Jung SW, Jeon SH, Yun SC, Oh HC, Kwon S, Lee SK, Seo DW, Kim MH, Suh DJ. Hepatitis B virus infection and intrahepatic cholangiocarcinoma in Korea: a case-control study. Am J Gastroenterol. 2008. 103:1716–1720.

9. Kim YI, Yang DH, Chang KR. Relationship between Clonorchis sinensis infestation and cholangiocarcinoma of the liver in Korea. Seoul J Med. 1974. 15:247–253. (in Korean).
10. Chung CS, Lee SK. An epidemiological study of primary liver carcinomas in Busan area with special reference to clonorchis. Korean J Pathol. 1976. 10:33–46.
11. World Health Organization. International Classification of Diseases. 1992. vol. 10. Geneva: World Health Organization.
12. Fritz A, Percy C, Jack A, Shanmugaratnam K, Parkin M. International classification of diseases for oncology (ICD-O). 2000. 3rd ed. Geneva, Switzerland: World Health Organization.
13. Shin HR, Won YJ, Jung KW, Park JG, Hong EK, Suh CI, Lee SY, Kim KY, Seo SW, Lee JK. Cancer Incidence in Korea (1999-2002). Cancer Incidence in Five Continents. 2007. Volume IX. Lyon: International Agency for Research on Cancer.
14. Won YJ, Sung J, Jung KW, Kong HJ, Park SK, Shin HR, Park EC, Ahn YO, Hwang IK, Lee DH, Choi JS, Kim WC, Lee TY, Yoo CI, Bae JM, Kim ON, Park IS, Kong IS, Lee DH, Lee JS. Nationwide Cancer Incidence in Korea, 2003-2005. Cancer Res Treat. 2009. 41:122–131.

15. Kim TS, Cho SH, Huh S, Kong Y, Sohn WM, Hwang SS, Chai JY, Lee SH, Park YK, Oh DK, Lee JK. A nationwide survey on the prevalence of intestinal parasitic infections in the Republic of Korea, 2004. Korean J Parasitol. 2009. 47:37–47.

16. McGlynn KA, Tarone RE, El-Serag HB. A comparison of trends in the incidence of hepatocellular carcinoma and intrahepatic cholangiocarcinoma in the United States. Cancer Epidemiol Biomarkers Prev. 2006. 15:1198–1203.

17. West J, Wood H, Logan RF, Quinn M, Aithal GP. Trends in the incidence of primary liver and biliary tract cancers in England and Wales 1971-2001. Brit J Cancer. 2006. 94:1751–1758.

18. Welzel TM, McGlynn KA, Hsing AW, O'Brien TR, Pfeiffer RM. Impact of classification of hilar cholangiocarcinomas (Klatskin tumors) on the incidence of intra- and extrahepatic cholangiocarcinoma in the United States. J Natl Cancer Inst. 2006. 98:873–875.

21. Khan SA, Toledano MB, Taylor-Robinson SD. Epidemiology, risk factors, and pathogenesis of cholangiocarcinoma. HPB (Oxford). 2008. 10:77–82.

22. de Groen PC, Gores GJ, LaRusso NF, Gunderson LL, Nagorney DM. Biliary tract cancers. N Engl J Med. 1999. 341:1368–1378.

23. Okuda K, Nakanuma Y, Miyazaki M. Cholangiocarcinoma: recent progress. Part 1: epidemiology and etiology. J Gastroenterol Hepatol. 2002. 17:1049–1055.

24. Chen MF, Jan YY, Jeng LB, Hwang TL, Wang CS, Chen SC, Chao TC, Chen HM, Lee WC, Yeh TS, Lo YF. Intrahepatic cholangiocarcinoma in Taiwan. J Hepatobiliary Pancreat Surg. 1999. 6:136–141.

25. Kubo S, Kinoshita H, Hirohashi K, Hamba H. Hepatolithiasis associated with cholangiocarcinoma. World J Surg. 1995. 19:637–641.

26. Kim YT, Byun JS, Kim J, Jang YH, Lee WJ, Ryu JK, Kim SW, Yoon YB, Kim CY. Factors predicting concurrent cholangiocarcinomas associated withhepatolithiasis. Hepatogastroenterology. 2003. 50:8–12.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download