Abstract
The prevalence of group B streptococcus (GBS) among pregnant women and disease burdens in neonates and adults are increasing in Korea. Colonizing isolates, collected by screening pregnant women (n=196), and clinical isolates collected from clinical patients throughout Korea (n=234), were serotyped and screened for antibiotic resistance. Serotype III (29.8%) and V (27.7%) predominated, followed by Ia (17.0%). Antibiotic resistance was higher among clinical than colonizing isolates for erythromycin (35.1% and 26.9%; P=0.10) and for clindamycin (49.4% and 42.1%; P=0.17). erm(B) occurred in 91.9% of erythromycin resistant isolates, and 84.0% of isolates resistant to clindamycin. Only five isolates (4.2%) resistant to erythromycin were susceptible to clindamycin; by contrast, and unique to Korea, 34% of isolates resistant to clindamycin were erythromycin susceptible. Among these 60 erythromycin-susceptible & clindamycin-resistant isolates, 88% was serotype III, and lnu(B) was found in 89% of strains. Four fifths of the serotype V isolates were resistant to both erythromycin and clindamycin. Further characterization of the genetic assembly of these resistance conferring genes, erm(B) and lnu(B), will be useful to establish the clonal lineages of multiple resistance genes carrying strains.
Group B streptococcus (GBS, also known as Streptococcus agalactiae) was first described as a pathogenic organism of the human body 60 yr ago (1), and was identified as the most frequent cause of neonatal sepsis and meningitis in the 1970s (2). Since then, GBS has emerged as a major pathogen for a variety of bacterial infections among pregnant women, non-pregnant adults, and the aged (3). In the United States, screening followed by intrapartum antibiotics has halved the rate of early-onset neonatal sepsis (4), but GBS remains the most common cause of early onset neonatal sepsis, and the incidence of late-onset neonatal disease and other GBS infections in pregnancy has remained unchanged. Further, the emergence of GBS resistant to second-line treatments used for those allergic to penicillin has complicated treatment decisions. Thus, a prenatal screening program followed by antibiotic treatment is only an interim solution; studies to develop an effective vaccine based on the capsular polysaccharide (CPS), which determines serotype, are ongoing (5). There are 9 (and possibly 10) known serotypes (6); the distribution of serotypes differs by geographic area.
Despite its importance as a pathogen, there are few studies of GBS in Asia generally, and Korea in particular. As has been true elsewhere, the role of GBS as a neonatal pathogen was previously overlooked in Korea; only recently did investigations identify GBS as the most common cause of neonatal bacterial meningitis (7). GBS prevalence among those pregnant women screened in Korea is about 5% (8), lower than that of Germany (16%) (9) or the United States (20%) (10). However, macrolide resistance among isolates tested has increased in the previous 10 yr (9). Moreover the prevalence of GBS in pregnant women has increased to 8% in Korea (11). Thus, there is much to be learned about the epidemiology of GBS in Korea, not only to better understand how to treat and prevent GBS disease in Korea, but because of the potential for spread of resistant strains throughout the world. In this study, we investigated the serotype characteristics, antibiotic phenotype and genotype (erm[A], erm[B], mef[A] and lnu[B]), among GBS isolates collected from pregnant women and clinical patients from year 2004 to 2007 in Korea.
The study collection included 196 colonizing isolates collected from 140 asymptomatic pregnant women (35-37 weeks of gestation) and 234 clinical isolates collected from 231 patients with GBS infection. GBS isolates were collected from pregnant women receiving prenatal care at four hospitals, Eulji Hospitals in Seoul and Daejeon, Cheil Hospital in Seoul, and Motae Women's Hospital in Daejeon.
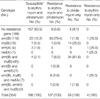
The isolates from clinical patients were sent to the Seoul Clinical Laboratories & Seoul Medical Science Institute (SCL) for microorganism culture from hospitals and clinics throughout the country between January, 2006 and March, 2007 (Table 1).
Written informed consent was obtained from all pregnant women, and the study protocol was approved by the Institutional Review Board of Eulji University Hospital (04-08 and 06-25), and Cheil Hospital (SCH-IRB-2005-24).
Mucus or discharge were collected on a swab from the vaginal mucosa (vagina introitus) of pregnant women without using a speculum and then placed in Stuart transport medium. A rectal swab was rolled two to three times around the rectal opening, and placed in a separate Stuart transport medium. About 20 mL of initial urine of pregnant women were collected in a sterile urine cup. The following protocol was used for specimen culture and bacteria identification in each laboratory and SCL. All media and supplies were purchased by the research team and distributed to participating laboratories. All isolates were cultured by using a selective media (Todd-Hewitt [TH] broth supplemented with either gentamicin [8 µg/mL] and nalidixic acid [15 µg/mL], or with colistin [10 µg/mL] and nalidixic acid [15 µg/mL]) to prevent growth of bacteria other than GBS. Urine was centrifuged and 1 mL of the bottom part was put in the selective media. Swabs of vaginal and rectal specimen were transferred directly from transport to selective media, and shaken three or four times so that the specimens were thoroughly mixed with the selective medium. The cap of the selective media was loosely closed and cultured in a 5% CO2 incubator at 35-37℃ for 18-24 hr; a negative control of selective media was cultured with each group of swabs. Tubes were checked for GBS growth after 18-24 hr, and then again after 48 hr. If bacterial growth was observed in the selective media, the bacteria were cultured on a sheep blood agar plate, that is, a tryptic soy agar with 5% defibrinated sheep blood (TSAII; KOMED Co., Sungnam, Korea). We used a catalase test followed by a latex agglutination assay (Streptex; Murex Biotech Ltd., Dartford, England) to confirm the isolate was GBS. All confirmed GBS isolates were tested for sensitivity to penicillin G, ampicillin, erythromycin, clindamycin, cefazolin (or cefuroxime) and vancomycin by using microtiter broth determinations. Erythromycin-resistant, clindamycin-susceptible isolates are tested for inducible clindamycin resistance by double-disk diffusion (D test). Interpretation is based on the protocols of Clinical and Laboratory Standards Institute (CLSI, formerly NCCLS) (12).
GBS-kit, Essum® products of Sweden was used for determining serotypes. Dot blot capsular type (13) in a microarray format (14) was performed for isolates that were categorized as non-typeable by this test (54 cases, 12.6% of the total), by using protocols described previously and serotypes were determined for all 430 GBS strains. The following isolates were used as positive controls for dot blot capsular typing: CNCTC 1/85 (Ia), DK14 (Ib), DK23 (II), M781 (III), CNCTC 1/82 (IV), CNCTC 10/84 (V), NT6 (VI), 87-603 (VII), and JM9 (VIII) (C.E. Rubens collection) (15).
GBS strains were inoculated in 9 mL of TH broth (BD, Sparks, MD, USA) and then incubated at 37℃ with 5% CO2 for 18-24 hr. Genomic DNA was extracted and purified by using sonication and heat treatment as previously described (14). The genomic DNA from 408 of the 430 strains (95%) were arrayed in duplicate on Vivid Gene Array slides with nylon membranes (Pall, Ann Arbor, MI, USA) by using the VersArray ChipWriter Compact system (Bio-Rad, Hercules, CA, USA). 22 of the isolates from the original collection were not included in the library on a slide because of low cell density during DNA extraction procedures, despite repeated attempts to culture.
Polymerase chain reaction (PCR) amplification of probe sequences was performed by the following method: DNA lysates were prepared from 3 mL of GBS overnight culture in TH broth. Each reaction mixture (48 µL) included 50 pmole of each primer, 1 µL of diluted DNA lysate, and 45 µL of Accuprime super mix II (Invitrogen, San Diego, CA, USA). Primers to detect erm(B) and mef(A) and lnu(B) were described previously (8). Primers were designed to amplify erm(A) (genes included erm[A] and erm[TR]) from available sequence 5'-AAA ATA ATA GAA ATT GGG TCA GGA AAA GGA CAT TTT ACC-3'and 5'-CCC ATT TAT AAA CGA AAA ATC TAT ACT TTT TGT AGT CCT TCT T-3'. Reactions were carried out by using a Bio-Rad MyCyclerTM by using the following conditions: denaturation at 94℃ for 30 sec, annealing at 54℃ (erm[A], erm[B] and lnu[B]) or 57℃ for 30 sec (mef[A]) for 35 cycles, and elongation at 68℃ for 1 min, followed by a final elongation at 68℃ for 6 min. A total of 10 µL of PCR product was analyzed by electrophoresis on a 1% agarose gel, stained with 0.02 µg/mL of ethidium bromide, and visualized by UV transillumination.
PCR amplification products were purified by using the QIAquick gel extraction kit and the QIAquick PCR purification kit (QIAGEN Inc., Valencia, CA, USA) and labeled with 2.5 µL of 1 mM/L fluorescein-12-dCTP (PerkinElmer, Boston, MA, USA) by using a modification of the BioPrime DNA Labeling System (Invitrogen) as previously described (16). The quantification probe (labeled with digoxigenin) consisted of a mixture of GBS housekeeping genes (adh[P], glc[K], gln[A], and phe[S]) was used to account for differences in genomic DNA concentrations across strains. The probes were hybridized in duplicate to genomic DNA arrayed on slides by using previously described methods; hybridization signals were detected by using an Arrayit ChipReader and analyzed with IconoClust software (16). The signal intensity of the spots were adjusted for background and normalized to the signal intensity of a quantification probe. Cutoffs for probe positive strains were established by using previously published methods (17). PCR was used to confirm presence or absence of antimicrobial resistance genes for strains where hybridization results were inconclusive.
We compared the frequency of serotype and antimicrobial resistance between colonized and clinical GBS strains by using the chi-square test.
Study isolates (n=430) were collected over a 3 yr period from various geographic areas in Korea (Table 1). All colonizing isolates were from pregnancy screening, whereas clinical isolates were from 'test requested' samples to the Seoul Clinical Laboratory from throughout Korea. The clinical isolates were from urine (50.4%), surgical wound (10.3%), pus or abscess (8.1%), vagina (7.7%), cervix (6.0%), blood or cerebrospinal fluid (3.9%), prostate (3.0%), sputum (1.7%), and others (9.0%). The colonizing isolates were from the urine (42.9%), vagina (27.0%), rectum (21.9%) or from combined vaginal/rectal specimens (8.2%). In several cases multiple isolates were collected from different sites in a single individual; we assumed these isolates were the same if the isolates had the same serotype, antibiotic resistance profile and antibiotic resistance genotype (erm[A], erm[B], mef[A] and lnu[B]). Six individuals had two different isolates; the remaining analyses are limited to the 376 unique isolates obtained from 371 individuals. Genotype for erythromycin and clindamycin resistance was generated for 354 isolates, because of low DNA concentration (Fig. 1).
Overall, serotype III (29.8%) and V (27.7%) predominated, followed by Ia (17.0%, Table 2). Serotype III (35.2%) predominated than serotype V (24.1%) among colonizing isolates, whereas serotype V (29.9%) was predominant, followed serotype III (26.4%) among clinical isolates, but the serotype distribution did not differ significantly between colonizing and clinical isolates (P=0.18, Table 3).
The frequency of erythromycin and clindamycin resistance was higher among clinical than colonizing isolates: 26.9% of colonizing isolates and 35.1% of clinical isolates showed resistance to erythromycin (P=0.10), while 42.1% of colonizing, and 49.4% of the clinical isolates were resistant to clindamycin (P=0.17). The resistance rates to both erythromycin and clindamycin were 24.8% of colonizing and 34.2% of clinical isolates, and the differences showed borderline significance (P=0.06). Combining colonizing and clinical isolates, the overall resistance to erythromycin was 31.9% and to clindamycin was 46.5%. All but four isolates resistant to erythromycin were also resistant to clindamycin, but 34.3% (60/175) of those resistant to clindamycin were susceptible (or showed intermediate) to erythromycin. No isolates were resistant to ampicillin, penicillin G, or vancomycin. One isolate (0.7%) showed intermediate to cefazolin, a first generation cephalosporin used to test for resistance among colonizing isolates. Clinical isolates were tested for resistance to cefuroxime sodium, a second generation cephalosporin; three isolates (1.3%) were resistant (Fig. 2).
Most erythromycin and clindamycin resistance occurred in serotypes III and V. Serotypes VII and VIII also had high levels of resistance, but the numbers in these groups are small. Serotype III strains were more resistant to clindamycin (61.6%) than to erythromycin (16.1%), with 47.3% of isolates resistant to clindamycin only and 1.8% resistant to erythromycin only (Table 2). Resistance was mainly constitutive; out of four strains that were phenotypically erythromycin resistant and clindamycin susceptible, erythromycin induced clindamycin resistance was seen in three; one strain was erm(A) positive and two strains were erm(B) positive.
Among the 376 unique isolates, 354 isolates were screened for the presence of resistance genes (Table 4). The most prevalent gene was erm(B) (46.6%, 165/354) and lnu(B) was detected in 19.8% (70/354) of strains. erm(A) (2.0%, 7/354) and mef(A) (2.3%, 8/354) occurred in less than 3% of isolates. Most erythromycin resistant isolates (91.9%, 102/111) and clindamycin resistant isolates (84.0%, 136/162) were erm(B) positive, while 14.4% (27/188) of both erythromycin and clindamycin susceptible isolates were erm(B) positive. lnu(B) was detected in 89.0% (49/55) in the isolates resistant to only clindamycin. mef(A) was not found in any of the isolates susceptible to both erythromycin and clindamycin. In all but one case, mef(A) occurred with erm(B) and lnu(B). lnu(B) was also highly associated with erm(B) (77.1%, 54/70 strains).
Among 430 isolates (376 unique isolates) from Korea collected between 2004-2007, we observed changing serotype distributions and high rates of resistance to erythromycin and clindamycin, with resistance levels varying by serotype. Clindamycin resistance is explained by presence of the lincosamide nucleotidyltransferase lnu(B), which inactivates lincosamides and clindamycin and confers resistance to clindamycin.
The distributions of serotypes observed in Korea has changed by years; Ib and III were dominant from 1979 to 1996 (18), and III was predominant and V was the next from 1997 to 2002 (19). However, in this study serotype V was predominant among clinical isolates (Table 3). The differences in serotype distribution among various populations may reflect differences in pathogenesis among the serotypes. Therefore, monitoring the serotype distribution is important for complete surveillance of GBS infections and for vaccine formulation.
Our study showed increased antibiotic resistance rate to clindamycin (35% (19) vs. 46.5%) and identified resistance to cefazolin and cefuroxime. Antibiotic resistance occurred almost exclusively among serotypes III and V; this is consistent with reports from elsewhere (4). Unlike reports from the United States, Canada, or Germany, resistance to clindamycin exceeded that for erythromycin (8, 20, 21). The "separation in prescribing and dispensing of medications" policy in Korea practiced since in August 2000 was expected to decrease antibiotic prescription and reduce the selection pressure for resistance. It is possible that problems implementing this health care policy (22) have limited the potential benefits or that the bacteria have developed compensatory mechanisms so that reversion to antibiotic sensitivity is less likely, or both.
There are two primary mechanisms known to cause erythromycin resistance in GBS: target site modification and active efflux (23, 24). Target site modification is mediated by erythromycin resistance methylase, which is encoded by the erm class genes. Macrolide efflux, which is caused by a membrane protein encoded by the mef class genes, has recently emerged among S. pyogenes and S. pneumoniae in many countries (24, 25). We observed very few isolates with mef genes, or erm genes other than erm(B). Four isolates were genotyped among five isolates which were resistant to erythromycin and susceptible to clindamycin (M phenotype); one was mef(A) positive, another was erm(A) positive, the third was erm(B) positive, and the other was erm(B), lnu(B) and mef(A) positive. The M phenotype occurred much less frequently (4.2%; 5/120) than in Canada (12.1%) (26) or Taiwan (13.7%) (27). While erm genes are also associated with inducible clindamycin resistance (along with erythromycin resistance), clindamycin resistance alone can also be conferred by lnu(B) which confers resistance via drug modification (28). lnu(B) was first described in Enterococcus faecium (28) and found in GBS by Azavedo et al. in 2001(26). The presence of lnu(B) in our collection (19.8%) likely explains resistance to clindamycin in the absence of erm genes. The high association of lnu(B) and erm(B) genes suggest that these genes are linked either physically or functionally in circulating GBS strains in Korea. The erm(B) gene is located on the Tn3872 transposon (Tn916 like) in GBS, it is not known if the lnu(B) gene in GBS is also located on a similar transposon or other mobile genetic elements (29). Interestingly all the erm(B) positive and lnu(B) positive strains belonged to serotype III. Further characterization of the genetic assembly of these resistance conferring genes and the genetic backbone of the strains carrying these genes will be useful to establish the clonal lineages of multiple resistance genes carrying strains.
Although there is substantial selection pressure for GBS to become resistant to penicillin and macrolides among countries screening and treating for GBS during pregnancy, GBS screening during pregnancy is not yet standard of care in Korea. Because it is a common inhabitant of the human microbiota, it is exposed to antibiotics taken by its human host for any reason, and can exchange genes with other microbes in the microbiota.
In conclusion, the molecular epidemiology of GBS in Korea is changing; the proportion of serotype Ib has decreased, serotype V has increased, and sertoypes VI, and VIII are emerging especially among clinical isolates. Four fifths of the serotype V isolates are resistant to both erythromycin and clindamycin and erm(B) and lnu(B) are related to erythromycin and clindamycin resistance, respectively. Ongoing monitoring for serotype and antibiotic resistance, and research to identify effective prevention and alternative treatments is an urgent matter.
Figures and Tables
Fig. 2
Frequency of antibiotic resistance among group B streptococcus isolates (n=376) collected from Korea (2004 to 2007).
*P=0.17, †P=0.10, ‡P=0.06. P values were obtained by chi-square test. All isolates were susceptible to ampicillin, penicillin G, and vancomycin.

ACKNOWLEDGMENTS
We thank SCL(Seoul Clinical Laboratories & Seoul Medical Science Institute), and the following physicians for providing some of the isolates used in this study: Ji-Hee Yu (Motae Women's Hospital, Daejeon), Jung Yeol Han, Hyun Mee Ryu, Hyun Kyong Ahn, Jin Hoon Chung, June Seek Choi and Min Hyoung Kim (Cheil General Hospital & Women's Healthcare Center, Kwandong University, Seoul); Jun-Suk Park, In-Tack Hwang, Jung-Hun Rho, Byung-Kwan Lee, and Young-Rae Song (Eulji University Hospital, Daejeon); and Seo-Yoo Hong and Won-Il Park (Eulji Hospital, Seoul). Additionally, we thank Dawn Reed for managing the database; Dr. Yong-Kyun Cho for DNA extraction (MAC-EPID, University of Michigan, Ann Arbor); and Sun Young Pai for preparing all GBS isolates (Eulji University, Daejeon).
References
1. Fry RM. Fatal infections by haemolytic streptococcus group B. Lancet. 1933. 1:199–201.
2. Baker CJ, Barrett FF, Gordon RC, Yow MD. Suppurative meningitis due to streptococci of Lancefield group B: a study of 33 infants. J Pediatr. 1973. 82:724–729.

3. Farley MM, Harvey RC, Stull T, Smith JD, Schuchat A, Wenger JD, Stephens DS. A population-based assessment of invasive disease due to group B streptococcus in nonpregnant adults. N Engl J Med. 1993. 328:1807–1811.

4. Phares CR, Lynfield R, Farley MM, Mohle-Boetani J, Harrison LH, Petit S, Craig AS, Schaffner W, Zansky SM, Gershman K, Stefonek KR, Albanese BA, Zell ER, Schuchat A, Schrag SJ. Epidemiology of invasive group B streptococcal disease in the United States, 1999-2005. JAMA. 2008. 299:2056–2065.
5. Maione D, Margarit I, Rinaudo CD, Masignani V, Mora M, Scarselli M, Tettelin H, Brettoni C, Iacobini ET, Rosini R, D'Agostino N, Miorin L, Buccato S, Mariani M, Galli G, Nogarotto R, Nardi Dei V, Vegni F, Fraser C, Mancuso G, Teti G, Madoff LC, Paoletti LC, Rappuoli R, Kasper DL, Telford JL, Grandi G. Identification of a universal Group B streptococcus vaccine by multiple genome screen. Science. 2005. 309:148–150.

6. Slotved HC, Kong F, Lambertsen L, Sauer S, Gilbert GL. Serotype IX, a proposed new Streptococcus agalactiae serotype. J Clin Microbiol. 2007. 45:2929–2936.

7. Lee HJ, Cho HK, Kim KH, Oh SH, Cha SH, Hur JK. Invasive bacterial infection in immunocompetent children in Korea: a retrospective multicenter study. 2007. In : 5th World Congress of the World Society for Pediatric Infectious Diseases-WSPID; Bangkok, Thailand. 112.
8. Gygax SE, Schuyler JA, Kimmel LE, Trama JP, Mordechai E, Adelson ME. Erythromycin and clindamycin resistance in group B streptococcal clinical isolates. Antimicrob Agents Chemother. 2006. 50:1875–1877.

9. Brimil N, Barthell E, Heindrichs U, Kuhn M, Lutticken R, Spellerberg B. Epidemiology of Streptococcus agalactiae colonization in Germany. Int J Med Microbiol. 2006. 296:39–44.

10. Schrag SJ, Whitney CG, Schuchat A. Neonatal group B streptococcal disease: how infection control teams can contribute to prevention efforts. Infect Control Hosp Epidemiol. 2000. 21:473–483.
11. Lee BK, Song YR, Kim MY, Yang JH, Shin JH, Seo YS, Oh KY, Yoon HR, Pai SY, Foxman B, Ki M. Epidemiology of group B streptococcus in Korean pregnant women. Epidemiol Infect. 2010. 138:292–298.

12. NCCLS. Performance Standard for Antimicrobial Susceptibility Testing, M100-S12. Table 2H. 2002. Wayne, PA, USA: NCCLS.
13. Borchardt SM, Foxman B, Chaffin DO, Rubens CE, Tallman PA, Manning SD, Baker CJ, Marrs CF. Comparison of DNA dot blot hybridization and lancefield capillary precipitin methods for group B streptococcal capsular typing. J Clin Microbiol. 2004. 42:146–150.

14. Zhang L, Srinivasan U, Marrs CF, Ghosh D, Gilsdorf JR, Foxman B. Library on a slide for bacterial comparative genomics. BMC Microbiol. 2004. 4:12.
15. Harris TO, Shelver DW, Bohnsack JF, Rubens CE. A novel streptococcal surface protease promotes virulence, resistance to opsonophagocytosis, and cleavage of human fibrinogen. J Clin Invest. 2003. 111:61–70.

16. Zhang L, Reddi U, Srinivasan U, Li S, Borchardt SM, Pillai P, Mehta P, Styka AN, Debusscher J, Marrs CF, Foxman B. Combining microarray technology and molecular epidemiology to identify genes associated with invasive group B streptococcus. Interdiscip Perspect Infect Dis. 2008. 314762.
17. Marrs CF, Zhang L, Tallman P, Manning SD, Somsel P, Raz P, Colodner R, Jantunen ME, Siitonen A, Saxen H, Foxman B. Variations in 10 putative uropathogen virulence genes among urinary, faecal and peri-urethral Escherichia coli. J Med Microbiol. 2002. 51:138–142.

18. Lee K, Shin JW, Chong Y, Mikamo H. Trends in serotypes and antimicrobial susceptibility of group B streptococci isolated in Korea. J Infect Chemother. 2000. 6:93–97.
19. Uh Y, Kim HY, Jang IH, Hwang GY, Yoon KJ. Correlation of serotypes and genotypes of macrolide-resistant Streptococcus agalactiae. Yonsei Med J. 2005. 46:480–483.
20. Desjardins M, Delgaty KL, Ramotar K, Seetaram C, Toye B. Prevalence and mechanisms of erythromycin resistance in group A and group B streptococcus: implications for reporting susceptibility results. J Clin Microbiol. 2004. 42:5620–5623.

21. Schoening TE, Wagner J, Arvand M. Prevalence of erythromycin and clindamycin resistance among Streptococcus agalactiae isolates in Germany. Clin Microbiol Infect. 2005. 11:579–582.

22. Kim MW, Jang HO, Chang DY, Cho JR, Kim YA, Choi HM, Kim SH, Lee JP, Hwang KJ, Kang BH. Group B streptococcal colonization rate in Korean pregnant women. Korean J Obstet Gynecol. 2006. 49:337–344.
23. Leclercq R, Courvalin P. Bacterial resistance to macrolide, lincosamide, and streptogramin antibiotics by target modification. Antimicrob Agents Chemother. 1991. 35:1267–1272.

24. Sutcliffe J, Tait-Kamradt A, Wondrack L. Streptococcus pneumoniae and Streptococcus pyogenes resistant to macrolides but sensitive to clindamycin: a common resistance pattern mediated by an efflux system. Antimicrob Agents Chemother. 1996. 40:1817–1824.

25. Kataja J, Huovinen P, Skurnik M, Seppala H. Erythromycin resistance genes in group A streptococci in Finland. The Finnish Study Group for Antimicrobial Resistance. Antimicrob Agents Chemother. 1999. 43:48–52.
26. de Azavedo JC, McGavin M, Duncan C, Low DE, McGeer A. Prevalence and mechanisms of macrolide resistance in invasive and noninvasive group B streptococcus isolates from Ontario, Canada. Antimicrob Agents Chemother. 2001. 45:3504–3508.

27. Hsueh PR, Teng LJ, Lee LN, Ho SW, Yang PC, Luh KT. High incidence of erythromycin resistance among clinical isolates of Streptococcus agalactiae in Taiwan. Antimicrob Agents Chemother. 2001. 45:3205–3208.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download