Abstract
Situs inversus totalis is a rare anomaly in which the abdominal and thoracic cavity structures are opposite their usual positions. A 41-yr-old woman, who had an ulcerating cancer on the rectum, was found as a case of situs inversus totalis. We present an overview of the operative technique for the first documented laparoscopic total mesorectal excision of a rectal cancer in the patient with situs inversus totalis. Careful consideration of the mirror-image anatomy permitted a safe operation using techniques not otherwise different from those used for the general population. Therefore, curative laparoscopic surgery for rectal cancer in this patient is feasible and safe.
Situs inversus totalis (SIT) is a rare congenital anomaly with an incidence of 1 in 5,000-20,000 (1). Several reports on surgical procedures in SIT patients have documented greater technical difficulties, as the anatomy is abnormal (2-8). Laparoscopy can prove to be an even greater technical challenge (2, 6). Although laparoscopic colorectal surgery has recently become a standard procedure, there are only four reports on laparoscopic surgery for colonic disease in patients with SIT (2-5). The majority of reported cases are laparoscopic sigmoidectomy for diverticular disease, while there is one case of a hemicolectomy with lymphadenectomy. To our knowledge, this is the first report on the feasibility of laparoscopic total mesorectal excision (TME) for a rectal cancer patient with SIT.
A 41-yr-old woman visited a local hospital, reporting bloody stool for 3 months. Colonoscopy revealed an ulcerative tumor in the lower rectum, 5 cm from the anal verge; biopsy confirmed that it was a well-differentiated adenocarcinoma. She was referred to our hospital in June 2008 for further evaluation and surgical treatment. She underwent an appendectomy at the age of 12 yr.
She was an unmarried woman. She was 159.5 cm tall and weighed 58.5 kg. The abdominal examination revealed a low midline appendectomy scar. Regarding the laboratory findings, she had no anemia (red blood cell count, 441×104 µL; hemoglobin, 14.3 g/dL; hematocrit, 42.3%) and no hepatic, renal, or electrolyte dysfunction. The serum carcinoembryonic antigen was not elevated (0.8 ng/mL; reference range, 0 to 4.7 ng/mL). A chest radiography showed dextrocardia and a right subphrenic gastric bubble (Fig. 1). Abdominopelvic computed tomography showed complete transposition of the abdominal viscera, confirming situs inversus totalis (Fig. 2).
In July 2008, a laparoscopic low anterior resection with a radical lymphadenectomy was performed by a right-handed surgeon, who had performed more than 500 laparoscopic colectomies at the time. After general anesthesia was induced, the patient was placed in a modified lithotomy position, with both arms tucked at her sides. The operator and endoscopist were situated on the left, and the first assistant was on the right, the reverse of the locations for orthotopic patients. A 12-mm supraumbilical port was placed, and a 30° telescope was introduced into the peritoneal cavity. There were severe adhesions between the omentum and peritoneal surface resulting from the previous operation. As expected, the sigmoid colon was observed on the right side, along with the spleen. The liver was in the left upper quadrant. Additional trocars included a 12-mm trocar in the left flank and a 5-mm trocar in the left iliac fossa as working ports for the operator, and a 12-mm trocar in the right iliac fossa and 5-mm trocar in the right flank for traction. The sigmoid colon was mobilized using ultrasonic dissection. The right ureter was clearly identified and was avoided during dissection (Fig. 3). The inferior mesenteric artery was isolated and divided at its origin (Fig. 4), and the inferior mesenteric vein and colic artery were divided using LigaSure™, (Valleylab, Boulder, CO, USA) (Fig. 5). The sigmoid and descending colons were mobilized up to the level of the inferior border of the pancreas using a medial-to-lateral dissection technique (Fig. 6). And then the operator and endoscopist positioned themselves on the right with the first assistant on the left to mobilize the rectum and make the anastomosis, because the operator was right-handed. The TME was performed, and the distal rectum was divided using articulating endoscopic linear stapler (Endopath Endo-Cutter®; Ethicon Endo-Surgery Inc., Cincinnati, OH, USA). Using an extension (about 5 cm) to a trocar site in the right iliac fossa, the specimen was extracted and amputated (Fig. 7). A pursestring suture was used to hold the anvil of a circular stapling device in the proximal colon. The colon was returned to the abdomen, and the abdominal incision was closed. After restoring the pneumoperitoneum, a 29-mm end-to-end anastomotic stapling device (CDH29®; Ethicon Endo-Surgery Inc., Cincinnati, OH, USA) was inserted anally, and the anastomosis was completed (Fig. 8). The operating time was 250 min, and the blood loss was 120 mL; that differed from the typical findings in orthotopic patients because of either the severe intra-abdominal adhesions or the position change by the surgeons.
Macroscopically, the tumor was a 45×40-mm ulcerated lesion in the rectum (Fig. 9). Histological examination of the resected specimen disclosed a well-differentiated adenocarcinoma with pericolic fat tissue invasion, but no lymph node metastasis (pT3N0, LN 0/9); the proximal, distal, and circumferential resection margins were 7, 0.7, and 0.2 cm, respectively.
After an uneventful postoperative course, she was started on a clear liquid diet on postoperative day 3 and was discharged home on postoperative day 8.
Laparoscopic surgery in patients with SIT remains a technical challenge for the surgeon and is relatively rare, with few reported cases. Most of these are laparoscopic cholecystectomies (6-8), and only six advanced laparoscopic procedures have been described, including three sigmoidectomies for diverticulitis, a hemicolectomy for colon cancer, a gastrectomy for gastric cancer, and a gastric bypass for morbid obesity (2-5, 9, 10). These procedures are extremely uncommon as a result of the small patient population and a reluctance to attempt laparoscopy due to the altered anastomotic orientation (4). Iwamura et al. (11) reported rectal cancer surgery using an open procedure in a patient with SIT, but no cases of laparoscopic TME in this population have been reported.
A laparoscopic colectomy is a good option for patients with SIT (2-4), but it requires thorough preoperative planning, including assessment of the anastomosis and the positions of surgeons and instruments. Clearly, the surgeon's experience with advanced laparoscopic surgery is a crucial factor affecting the choice of the operating method.
Oms and Badia (6) reported a potential advantage for left-handed surgeons during laparoscopic surgery in patients with SIT, although Jobanputra et al. (4) suggested that right-handed surgeons should not hesitate to perform this procedure because of the challenging anastomosis. We agree with this because, after carefully recognizing the mirror-image anatomy, the surgical technique itself did not differ from the typical situation.
In rectal cancer patients with SIT, despite the unfamiliar anatomy, the laparoscopic TME may be an acceptable alternative to open surgery. These patients should not be denied the benefits of minimal-invasive surgery, assuming that it can be performed safely. Laparoscopic TME is a safe and feasible option for patients with SIT.
Figures and Tables
Fig. 2
Computed tomography disclosing complete transposition of the abdominal viscera: (A) coronal view and (B) axial view.
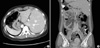
Fig. 3
Origin of the inferior mesenteric artery (IMA) from the right side of the abdominal aorta. CIA, common iliac artery.
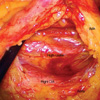
Fig. 7
Extracorporeal extraction of the specimen through a 12-mm port in the right lower quadrant of the abdomen.

References
1. Nursal TZ, Baykal A, Iret D, Aran O. Laparoscopic cholecystectomy in a patient with situs inversus totalis. J Laparoendosc Adv Surg Tech A. 2001. 11:239–241.

2. Kobus C, Targarona EM, Bendahan GE, Alonso V, Balague C, Vela S, Garriga J, Trias M. Laparoscopic surgery in situs inversus: a literature review and a report of laparoscopic sigmoidectomy for diverticulitis in situs inversus. Langenbecks Arch Surg. 2004. 389:396–399.

3. Fujiwara Y, Fukunaga Y, Higashino M, Tanimura S, Takemura M, Tanaka Y, Osugi H. Laparoscopic hemicolectomy in a patient with situs inversus totalis. World J Gastroenterol. 2007. 13:5035–5037.

4. Jobanputra S, Safar B, Wexner SD. Laparoscopic diverticular resection with situs inversus totalis (SIT): report of a case. Surg Innov. 2007. 14:284–286.

5. Davies H, Slater GH, Bailey M. Laparascopic sigmoid colectomy for diverticular disease in a patient with situs inversus. Surg Endosc. 2003. 17:160–161.

6. Oms LM, Badia JM. Laparoscopic cholecystectomy in situs inversus totalis: the importance of being left-handed. Surg Endosc. 2003. 17:1859–1861.

7. Al-Jumaily M, Hoche F. Laparoscopic cholecystectomy in situs inversus totalis: is it safe? J Laparoendosc Adv Surg Tech A. 2001. 11:229–231.

8. Machado NO, Chopra P. Laparoscopic cholecystectomy in a patient with situs inversus totalis: feasibility and technical difficulties. JSLS. 2006. 10:386–391.
9. Yamaguchi S, Orita H, Yamaoka T, Mii S, Sakata H, Hashizume M. Laparoscope-assisted distal gastrectomy for early gastric cancer in a 76-year-old man with situs inversus totalis. Surg Endosc. 2003. 17:352–353.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download